Approach
Diagnosis is based classically on signs and symptoms of obstructive hydrocephalus and, less frequently, cerebellar dysfunction, in the presence of a contrast-enhancing mass in the posterior fossa of the brain. This is most commonly within the fourth ventricle and midline vermis of the cerebellum, and less frequently in isolation within the lateral hemispheres of the cerebellum, or invading the dorsal aspect of the brain stem and projecting outward into the fourth ventricle and cerebellum.[25][26][27][28][29][30][31] Symptoms can be present for weeks to months prior to the diagnosis.
History
Very young children may not be able to express how they are feeling, so it will often be the parents/caregivers who describe changes in their child's behavior (e.g., irritability, decreased social interaction). Obstructive hydrocephalus caused by the tumor results in headaches, lethargy, nausea, and vomiting, and is present in >80% of patients at presentation. Headaches and vomiting classically occur in the morning and get better during the day, although symptoms may occur at any time of day. Vomiting occurs in the absence of fever or other signs of an infection, and often relieves the headache.[24] Patients may also report visual disturbance, most commonly diplopia. Those with metastatic disease in the spinal cord may present with back pain, weakness, and/or bowel or bladder dysfunction.
Physical exam
Exam is often normal. If signs are present, they are usually related to the obstructive hydrocephalus (e.g., impaired horizontal gaze or diplopia due to a sixth nerve palsy, papilledema) rather than the tumor itself (e.g., ataxia, nystagmus, head tilt, dysmetria). Infants <18 months of age can present with rapid increase in head circumference or bulging anterior fontanelle. Patients presenting with only cranial neuropathies rarely have a medulloblastoma and are more likely to have a brainstem glioma.
Investigations
Magnetic resonance imaging (MRI) of the brain is the preferred test.[3][25] CT is useful for rapid assessment in the acute setting, or if MRI is unavailable/contraindicated; however, MRI is the diagnostic standard for evaluation of the tumor and assessment of associated brain or spinal metastases. The advantages of CT over MRI are that it is quicker, does not require sedation, and is easier to obtain urgently. The advantage of MRI over CT is that it gives a better anatomic view of the brain with no exposure to radiation.[32] CT is not appropriate for staging tumors.
A CT or MRI of the brain should be ordered in:[24]
Patients with morning headaches, intermittent headaches increasing in frequency or intensity, or persistent daily headaches lasting >1 week
Infants with an increasing head circumference or a bulging fontanelle
Patients with impaired upward gaze
Unexplained persistent nausea and vomiting
Ataxic patients or worsening coordination and balance.
A careful metastatic evaluation with a nonenhanced and contrast-enhanced MRI of the brain and whole spine is mandatory.[3] Brain MRI may be complemented by advanced neuroimaging techniques such as MR perfusion imaging, MR spectroscopy, and positron emission tomography scan (PET), to enhance diagnostic capability, differentiate active neoplasm, and guide biopsy.
Cerebrospinal fluid (CSF) should be examined for tumor cells for all patients following recovery from surgery even if brain and spine MRI show no evidence of metastatic tumor.[33] CSF taken by lumbar puncture at least 10 days after surgery has been shown to be more reliable than ventricular CSF for staging purposes.[3][25][34]
Postoperative MRI is essential to evaluate the extent of resection and should be performed within 72 hours of tumor resection, ideally within the first 24 hours, after which time postoperative changes render interpretation of residual disease difficult.[3] If it cannot be performed in that timeframe, then it should not be performed for at least 10 days after surgery.[Figure caption and citation for the preceding image starts]: MRI: axial view of medulloblastoma, T1WI with gadolinium, showing an avidly enhancing solid and cystic lesion filling the fourth ventricleFrom the collection of Peter B. Storm; used with permission [Citation ends].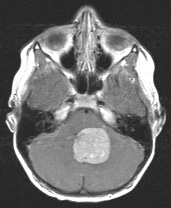 [Figure caption and citation for the preceding image starts]: MRI: coronal view of medulloblastoma, T1WI with gadolinium, showing an avidly enhancing solid and cystic lesion filling the fourth ventricle; obstructive hydrocephalus presentFrom the collection of Peter B. Storm; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: MRI: coronal view of medulloblastoma, T1WI with gadolinium, showing an avidly enhancing solid and cystic lesion filling the fourth ventricle; obstructive hydrocephalus presentFrom the collection of Peter B. Storm; used with permission [Citation ends].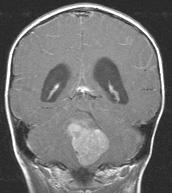 [Figure caption and citation for the preceding image starts]: MRI: sagittal view of medulloblastoma, T1WI with gadolinium, showing multiple avidly enhancing drop metastases from the patient's posterior fourth ventricular medulloblastomaFrom the collection of Peter B. Storm; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: MRI: sagittal view of medulloblastoma, T1WI with gadolinium, showing multiple avidly enhancing drop metastases from the patient's posterior fourth ventricular medulloblastomaFrom the collection of Peter B. Storm; used with permission [Citation ends].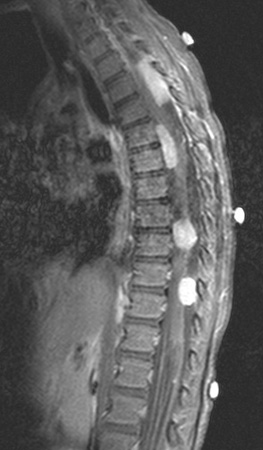
Pathology
The tumor should be surgically resected in all patients to obtain a diagnosis and prognosis based on the histologic subclass.[3][25] Diagnosis is based on the pathologist's review of the gross specimen, the microscopic findings, and immunohistochemical staining.[4] Analysis may include next generation whole exome/genome DNA sequencing, RNA sequencing and DNA methylation. A blood sample from the patient for corresponding germline sequencing should also be obtained and analyzed in concert with the tumor sample.
Use of this content is subject to our disclaimer