Tests
1st tests to order
serum bilirubin
Test
Conjugated bilirubin is elevated in obstructive jaundice.
Result
elevated
serum alkaline phosphatase
Test
Suggests obstructive (or cholestatic) pattern of elevated LFTs.
Result
elevated
serum gamma-GT
Test
Suggests obstructive (or cholestatic) pattern of elevated LFTs.
Result
elevated
serum aminotransferase
Test
May be minimally elevated. High elevations are seen more frequently in intrahepatic cholangiocarcinoma with direct hepatic invasion.[30]
Result
elevated
serum prothrombin time
Test
Caused by prolonged obstruction of the common bile or hepatic duct and a subsequent reduction in fat-soluble vitamins (A, D, E, and K).
Result
increased
serum CA 19-9
Test
Elevated in up to 85% of patients with cholangiocarcinoma. Also elevated in pancreatic or gastric malignancy, in severe hepatic injury from any cause, and with obstructive jaundice without malignancy. However, if levels continue to be elevated after biliary decompression, this suggests malignancy. Significantly elevated levels (>1000 U/mL) may indicate presence of metastatic disease.[7][41] In patients with primary sclerosing cholangitis and suspected cholangiocarcinoma, a value of >100 units/mL has a sensitivity of 75% and specificity of 80%.[42]
Result
elevated
serum carcinoembryonic antigen (CEA)
Test
Also elevated in inflammatory bowel disease, other tumors, and severe liver injury.
Result
elevated
serum CA-125
Test
Detectable in up to 65% of patients.
Result
elevated
abdominal ultrasound
Test
Identifies malignant versus benign lesions with a sensitivity of 92% and a specificity of 93%.[43][Figure caption and citation for the preceding image starts]: Gallbladder ultrasound of mass (arrows)From the collection of Dr Joseph Espat; used with permission [Citation ends].
Result
diagnosis suspected when intrahepatic ducts are dilated; intrahepatic cholangiocarcinoma may be seen as a mass lesion
abdominal CT
Test
CT identifies a primary lesion in approximately 59% of patients.[44] Cross-sectional imaging of the liver with CT or MRI is essential for evaluation of the primary mass, presence of metastases, vascular invasion, and resectability.[7][34]
Result
intrahepatic mass lesion, dilated intrahepatic ducts, and localized lymphadenopathy may be seen
abdominal MRI
Test
MRI is often utilized to differentiate between solid and cystic biliary contents. Furthermore, MRI can provide additional information regarding tumor size, extent of bile duct involvement, vascular patency, extrahepatic extension, nodal or distant metastases, and the presence of lobar atrophy. MRI diagnostic performance is comparable to CT.[33] Cross-sectional imaging of the liver with CT or MRI is essential for evaluation of the primary mass, presence of metastases, vascular invasion, and resectability.[7][34]
Result
local extent of tumor (the tumor is hypointense in T1- and hyperintense in T2-weighted image), hepatic parenchymal abnormalities, and liver metastases can be seen
Tests to consider
endoscopic ultrasound (EUS)
Test
EUS allows examination of the extrahepatic bile duct and tissue acquisition by fine needle aspiration from the primary mass and lymph nodes.[7] Endoscopic-ultrasound guided, or percutaneous, biopsies should be avoided in patients with perihilar cholangiocarcinoma who are potential transplant candidates, due to the risk of tumor dissemination.[7]
Result
characterizes size and location of tumor
MR angiography
Test
Preoperative imaging with MR angiography is a noninvasive method for staging cholangiocarcinoma, and therefore also helps determine resectability.
Result
staging tool
ERCP
Test
Tissue diagnosis in 40% to 70%.[Figure caption and citation for the preceding image starts]: ERCP image of hilar cholangiocarcinoma: Klatskin tumor with stricture of duct bifurcation (arrows)From the collection of Dr Joseph Espat; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: ERCP image of hepatic duct cholangiocarcinoma with duct stricture (arrows)From the collection of Dr Joseph Espat; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ERCP image of hepatic duct cholangiocarcinoma with duct stricture (arrows)From the collection of Dr Joseph Espat; used with permission [Citation ends].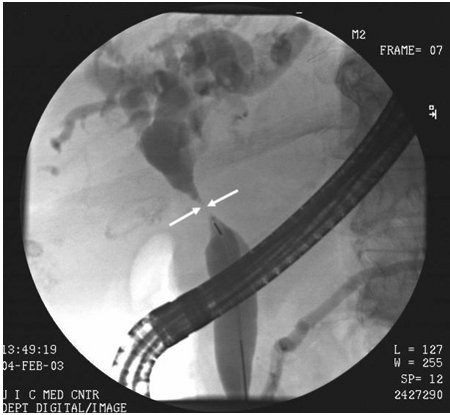
Staining for carcinoembryonic antigen (CEA), CA 19-9, or CA-50 aids in making a pathologic diagnosis.[6][9][14][20]
Result
a filling defect or area of narrowing will be seen if a tumor is present
MRCP
Test
Sensitivity comparable to PTC.[45] MRCP has the advantage of being noninvasive and does not carry the risks that ERCP or PTC do. The main disadvantage of MRCP is that it is diagnostic only, and no therapeutic options can be performed.
Result
can show extent of duct involvement above and below the obstruction
percutaneous transhepatic catheterization (PTC)
Test
Diagnostic sensitivity as high as 92%.[46] An invasive procedure that is used when the tumor causes complete obstruction of the biliary tree, and ERCP is unable to assess the biliary tree proximal to the tumor.
Result
may show dilated intrahepatic ducts with irregular filling defects and strictures at site of occlusion
positron emission tomography (PET)
Test
PET is useful in the diagnosis of many cancers; however, current literature cautions against the use of PET for determining the malignant potential of primary liver cancers. Literature on PET more strongly supports the role of restaging hepatobiliary malignancies and identifying metastatic disease.[7][38]
Sensitivity is low in cholangiocarcinoma.
Result
evidence of malignancy
Immunostaining
Test
Immunostaining of pathologic specimens to detect markers of hepatocellular carcinoma (e.g., GPC3, HSP70, and glutamine synthetase) or progenitor cell features (e.g., K19, EpCAM) is recommended to distinguish intrahepatic cholangiocarcinoma from mixed hepatocellular-cholangiocarcinoma tumors if this information will change management.
Result
may help to distinguish intrahepatic cholangiocarcinoma from mixed hepatocellular cholangiocarcinoma
Emerging tests
optical coherence tomography (OCT)
Test
Infrared light used to obtain scans that can correlate with histology.
Result
variable
peroral cholangioscopy
Test
In development for diagnostic imaging and for pathologic diagnosis.
Result
variable
duodenoscope-assisted cholangioscopy
Test
Evaluates the inside of the bile duct using the duodenal approach, as would be used for a stent placement. The FDA recommends duodenoscopes that have disposable, rather than fixed, endcaps to help limit device contamination.
Result
variable
Use of this content is subject to our disclaimer