Approach
The history should include a description of the typical attacks, including their nature, duration, triggers and associated auditory symptoms (e.g., hearing loss, tinnitus, and aural pressure).
The exam should include otoscopy, eye exam, central nervous system exam, and specific tests depending on the patient's presentation.
The diagnosis of dizziness is usually made on the basis of the history and exam only. Investigations may not be necessary. Magnetic resonance imaging (MRI) of the brain and internal auditory meatus may be helpful to detect neurologic pathology. Vestibular function tests are indicated in some cases. Tests of cardiovascular function are necessary if a cardiovascular cause is suspected.
History: characteristics of the current episode
The traditional approach to assessment is to classify the type of dizziness, with vertigo indicating a vestibular cause, disequilibrium a neurologic cause and presyncope a cardiovascular cause.[109] However, symptom types overlap substantially and patients most often report feeling off-balance or unsteady. Over 60% of patients experience more than one type of dizziness.[2] Nearly two thirds of of patients with cardiovascular causes of dizziness also report vertigo, and vertigo is the only type of dizziness described in 37% of these patients.[52]
An initial approach that considers trigger (positional or not) and timing (episodic or continuous) may be more useful as a first step than classifying the symptoms according to type (true vertigo, presyncope, or dysequilibrium).[109][110]
Duration of each episode of vertigo
Seconds: may be due to benign paroxysmal positional vertigo (BPPV)[12]
Seconds to minutes: may be due to labyrinthitis or vestibular neuronitis[12]
Hours: may be due to Meniere disease[12]
Months: persistent postural-perceptual dizziness (PPPD) symptoms last for 3 months or more.[111]
Check for triggers
Vertigo associated with BPPV occurs on head movement (e.g., bending down or looking up quickly) and is relieved by keeping the head still. Ask about turning or laying down in bed; vertiginous attacks triggered by turning or laying down in bed, together with dizziness lasting less than one minute, may help identify BPPV.[112]
In labyrinthitis, symptoms are exacerbated by head movement, but are also present at rest.
PPPD symptoms are exacerbated by being upright, active or passive motion independent of direction or position, and complex or moving visual stimuli. Triggered by conditions that cause vestibular symptoms or affect balance, including neuro-otologic illness and psychological distress.[111]
Dizziness on getting up quickly may be associated with orthostatic hypotension, postural orthostatic tachycardia syndrome, and presyncope.[113]
Mild attacks of vertebrobasilar insufficiency may be associated with orthostatic hypotension.
People with autonomic dysregulation present with dizziness on standing upright for prolonged periods, swimming, or running.
Vertigo induced by loud sounds or coughing may be due to semicircular canal dehiscence.
"TiTrATE" is an acronym for "timing, triggers, and a targeted examination." The authors of the acronym consider new onset vertigo as one of four distinct clinical syndromes, defined according to timing and triggers.
Timing refers to the onset, duration, and evolution of the dizziness. Triggers are actions, movements, or situations that provoke the onset of dizziness in patients who have intermittent symptoms.
These syndromes are:
Triggered episodic vestibular syndrome (e.g., BPPV, orthostatic hypotension)
Discrete episodes of dizziness lasting seconds
Precipitated by a specific action or event
Recommended examination includes Dix-Hallpike test (see below), lying and standing blood pressure
Spontaneous episodic vestibular syndrome (e.g., vestibular migraine, panic attacks, Meniere disease, cardiac arrhythmia)
Discrete episodes of dizziness lasting minutes to hours[15]
Most events have no clear trigger
Diagnosis made from history
Post-exposure acute vestibular syndrome (e.g., head injury, aminoglycoside exposure)
Persistent dizziness lasting days to weeks
History of trauma or toxin exposure
Diagnosis made from history
Spontaneous acute vestibular syndrome (e.g., vestibular neuritis, posterior circulation stroke)
Persistent dizziness lasting days to weeks
Associated nausea, nystagmus, gait unsteadiness and head motion intolerance
Recommended examination includes the head impulse, nystagmus, test of skew (HINTS) assessment.[8]
Presence of other otologic symptoms
Hearing loss may occur in Meniere disease, labyrinthitis, posterior fossa tumors, cholesteatoma, superior semicircular canal dehiscence (SCDS), and granulomatosis with polyangiitis (formerly known as Wegener's granulomatosis).
Tinnitus may occur in Meniere disease, labyrinthitis, posterior fossa tumors and cholesteatoma.[114]
Aural fullness occurs in Meniere disease.
Hyperacusis to bone-conducted sounds and autophony may occur in semicircular canal dehiscence.
Fever, otalgia, and otorrhea may occur in acute otitis media associated with labyrinthitis.
Malodorous ear discharge occurs in cholesteatoma.
Determine how the episodes began
Patients with a preceding upper respiratory infection may have viral neuritis or labyrinthitis.[115]
Patients with a history of sea, air, or train travel prior to the onset of symptoms and with symptoms occurring on disembarking may have mal de debarquement syndrome.[116]
Patients with a history of trauma or barotraumas (e.g., scuba divers or pilots) may have a perilymphatic fistula.[24]
Ask about other more general symptoms associated with the vertigo
The phrase "Dangerous Ds" can be a useful reminder of some of the red-flag symptoms that indicate a serious central cause for vertigo. These are:
Diplopia
Dysarthria
Dysmetria
Dysphagia
Dysphonia[8]
Associated chest pain, exertional presyncope, and dyspnea suggest a cardiovascular etiology.[117]
Nausea is often associated with peripheral vestibular disorders as a part of the autonomic response.
Vestibular migraine may be associated with aura, visual disturbance, photophobia, or phonophobia, with or without headaches.[118]
Posterior fossa tumors may cause headache.[114]
Patients with idiopathic intracranial hypertension are often obese and may complain of clumsiness, imbalance, headache and transient poor vision.
Patients with Cogan syndrome have ocular symptoms including photophobia, ocular discomfort and redness.[119]
Patients with granulomatosis with polyangiitis (formerly known as Wegener's granulomatosis) may present with nasal crusting, ulceration or epistaxis.
Recurrent genital and oral ulceration and uveitis occur in Behcet disease.
Psychiatric symptoms
Panic disorder with agoraphobia, personality disorders, or generalized anxiety is often present in patients complaining of dizziness. One study of 40 patients reported that an anxious, introverted temperament was strongly associated with chronic, subjective dizziness.[120]
If the dizziness is psychogenic, patients may describe symptoms of excessive anxiety or fear. A hospital and anxiety depression scale of >8 is diagnostic.[121]
Phobic postural vertigo is characterized by dizziness on standing and walking, despite normal clinical balance tests.
Patients may describe avoidance behavior to specific stimuli.[62]
Patients with psychophysiological dizziness may describe an initial labyrinthine disorder with persisting symptoms.
History: identification of cause
History of trauma or surgery
Dizziness may be a complication of stapedectomy and cochlear implantation.[122][123]
Patients who have had previous mastoid surgery with a mastoid cavity are prone to dizziness with ear infections.
A perilymphatic fistula may occur after stapes surgery, head trauma or barotrauma.[24]
Post-traumatic vertigo generally occurs as a result of blunt head trauma. Patients may present with symptoms of BPPV, a traumatic perilymphatic fistula or post-traumatic Meniere disease.[81] Vertigo can also occur as part of a post concussion syndrome.
Patients with SCDS may present after head trauma.
Orthostatic hypotension is a recognized complication after bariatric surgery.[58]
History of other medical illnesses
Diabetes mellitus may be associated with attacks of dizziness related to hypoglycemic episodes.[65]
Systemic lupus erythematosus may also be associated with dizziness.[66][67]
Dizziness occurs as an initial symptom in 5% of people with multiple sclerosis and occurs in 50% of patients at some point during the disease.[3]
Patients with a history of migraine are more likely to have migraine-associated vertigo.[118]
A history of certain connective tissue disorders, such as Ehlers-Danlos syndrome, Marfan syndrome, osteogenesis imperfecta, and fibromuscular dysplasia predispose patients to cervical artery dissection. Hypertension, recent infection, or trauma are also predisposing factors.[42][43]
Family history of illness
There may be a family history of migraine.
Known or contact with infectious disease
Secondary syphilis may present with bilateral sensorineural hearing loss or vertigo. Patients with otosyphilis often present with vertigo. Late neurosyphilis may present with hearing loss, fluctuating hearing, or vestibular symptoms.[68]
Audiovestibular symptoms (including sensorineural hearing loss) may be caused by reactivation of latent HSV-1 infection, and may be preceded by herpetic skin lesions.[68]
COVID-19 infection is associated with dizziness.[49][124][125][126]
Medication and drug history, and possible toxin exposure
Drugs associated with ototoxicity (e.g., aminoglycoside antibiotics), particularly if these have been administered concomitantly with loop diuretics or aspirin, and chemotherapeutic agents (e.g., cisplatin).
Anesthetic medication, antiarrhythmic medication, and drugs of misuse may cause patients to feel dizzy.
Oxcarbazepine and topiramate increase the risk of balance disorders.[77]
Drugs associated with orthostatic hypotension: antihypertensive medication, alpha-blockers, beta-blockers, nitrates, antipsychotics, opioids, antiparkinsonian drugs, and phosphodiesterase inhibitors.[78][79][127]
Alcohol intoxication can cause dizziness.
Accidental exposure to faulty or inadequately vented residential boilers, central heating systems, cookers, fireplaces, and chimneys may cause carbon monoxide poisoning.
Risk factors for cardiovascular disease or stroke
History of neoplastic disease
Physical exam: HINTS
HINTS is a set of three examinations: the head impulse test, characterization of spontaneous nystagmus, and test of skew. It can be performed quickly at the bedside and does not require any equipment.[129] It is a sensitive test for stroke in patients who have symptoms suggesting a vestibular cause of dizziness (e.g., vertigo, nausea or vomiting, unsteady gait, head-motion intolerance, nystagmus) and who have one or more risk factors for stroke.[83] HINTS has been found to identify stroke with a high degree of sensitivity and specificity in patients with acute vestibular symptoms if a healthcare professional with training and experience in the use of this test is available, and may rule out stroke more effectively than early diffusion-weighted MRI.[34][83] However, HINTS assessment alone does not reliably rule out stroke when used by emergency physicians.[84]
Head impulse test
The examiner turns the patient's head as rapidly as possible 15 degrees to one side and observes the patient's ability to keep fixating on a distant target. With a peripheral vestibular lesion, a saccade occurs as the vestibulo-ocular reflex fails, the patient cannot keep focusing on the target, and a catch-up movement occurs. After a cerebellar stroke, no catch-up saccade occurs: the head impulse test is negative. [Figure caption and citation for the preceding image starts]: Head impulse test. A: The right ear has intact peripheral vestibular function. When the head is turned to the right, the vestibulo-ocular reflex moves the eyes to maintain visual fixation. B: The right ear now has impaired vestibular function. When the head is turned to the right, the eyes move with it, breaking visual fixation, and a refixation saccade is seen as the eyes dart back to the examiner's face. This indicates a peripheral vestibular disorder on the right sideReproduced with permission from Nelson JA, Viirre E. The clinical differentiation of cerebellar infarction from common vertigo syndromes. West J Emerg Med. 2009 Nov;10(4):273-7. [Citation ends].
Characterization of spontaneous nystagmus
In vestibular neuritis, spontaneous nystagmus is torsional to horizontal and beating away from the side of the lesion. The nystagmus typically increases on looking toward the direction of the nystagmus, and decreases on looking away from the direction of the nystagmus (Alexander’s law).[109]
A central vestibular lesion produces vertical, bidirectional or pure rotatory nystagmus.
In bidirectional nystagmus, the fast phase is to the left when the patient looks to the left, and to the right when the patient looks to the right.
Both vestibular neuritis and central causes of vertigo can cause spontaneous horizontal nystagmus and gaze-evoked horizontal nystagmus.
Test of skew
Skew deviation is vertical ocular misalignment resulting from a right-left imbalance of vestibular tone
Perform an alternating cover test by asking the patient to fix on a target (such as your nose), then cover and uncover each eye in turn.
If the eyes are misaligned, after uncovering the affected eye it will move to refocus on the target. This is a positive result.
If the eye does not move after it is uncovered, this is normal. This is a negative test of skew.
Based on the HINTS model, one algorithm suggests that stroke should be considered in patients presenting with acute-onset dizziness if:[85]
There is a central pattern of nystagmus
There is skew deviation
There is a negative head impulse test (in patients with nystagmus)
There are any central nervous system signs on focused neurologic exam, or
The patient is unable to sit or walk unaided.
In the absence of these symptoms, patients in the accident and emergency department setting may be treated as having vestibular neuritis.[85]
Physical exam: ear
Ear exam
The tympanic membrane in acute otitis media is erythematous, opaque, and bulging. [Figure caption and citation for the preceding image starts]: Erythematous bulging tympanic membrane due to acute otitis mediaFrom the collection of Richard Buckingham, MD; used with permission [Citation ends].

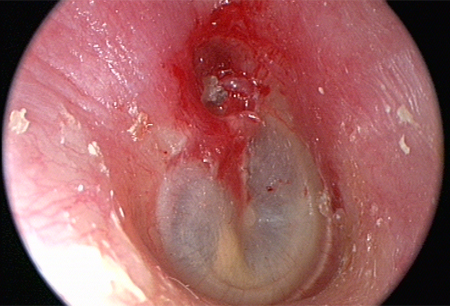
Crust or keratin in the attic (upper part of the middle ear), the pars flaccida, or the pars tensa (usually posterior superior aspect) suggests cholesteatoma. The tympanic membrane may be perforated. [Figure caption and citation for the preceding image starts]: Cholesteatoma in attic (upper part of the middle ear)From the collection of Susan A. Douglas, MBBS; used with permission [Citation ends].
There may be fluid or blood in the middle ear, and/or cerebrospinal fluid (CSF) otorrhea, if the dizziness is related to trauma.
People with granulomatosis with polyangiitis (formerly known as Wegener granulomatosis) may have signs of serous otitis media or chronic otitis media.
Tuning fork tests
Used to determine whether hearing loss is conductive or sensorineural.
Weber’s test: a 512-Hz tuning fork is placed on the forehead or maxillary teeth, and the patient is asked to state in which ear the sound is louder. The sound will be perceived in the affected ear when a unilateral conductive hearing loss is present or in the unaffected ear when there is a unilateral sensorineural hearing loss.
Rinne's testing allows the examiner to determine whether any hearing loss is secondary to middle ear (conductive hearing loss) or inner ear/eighth cranial nerve (sensorineural hearing loss) causes. The base of a 512-Hz tuning fork is placed on the mastoid and the patient indicates when he or she no longer hears the sound. Once the sound is no longer audible, the tuning fork is placed in front of the ear and the patient is asked whether he or she hears the sound. If the sound is louder when the tuning fork is on the mastoid, then the patient has a conductive hearing loss. If the sound is louder with the fork in front of the ear, hearing loss is sensorineural or normal. The result of this test is combined with the result of the Weber test to interpret the type of hearing loss.
The fistula test
Performed by applying pressure on the tragus to occlude the ear, or by pneumatic otoscopy (exerting pressure on each ear canal with a rubber bulb attached to an auriscope), thereby putting pressure on the middle ear.
A positive result of induced dizziness and nystagmus occurs with SCDS, postsurgical dizziness, or perilymphatic fistula.
Fistula test may be positive in people with cholesteatoma.
A positive fistula test provides support for doing a temporal bone computed tomography (CT).
Physical exam: eye
Observation of eye movements
Ophthalmoplegia with palsies of cranial nerves III, IV, or VI may occur with multiple sclerosis or with an intracranial lesion.[3]
Neurologic signs such as diplopia, disconjugate gaze, Horner syndrome, and gait ataxia are in keeping with a central lesion.
The presence of nystagmus may indicate peripheral or central pathology.
A central vestibular lesion produces vertical, bidirectional, or pure rotatory nystagmus.
Abnormal saccades and smooth pursuit may also indicate central pathology such as cerebellar disorders.
Sound- or pressure-induced nystagmus in the plane of the semicircular canal (positive Tullio and Hennebert tests) are a key finding in patients with SCDS.[23]
Fundoscopy
Papilledema may be present in idiopathic intracranial hypertension (pseudotumor cerebri)
Exam of the eyes with Frenzel glasses
These glasses use +30 diopter lenses to blur the patient's vision, remove optical fixation, and uncover vestibular nystagmus.[130][131]
It may be possible to use an ophthalmoscope instead of the Frenzel glasses to blur vision.
Infrared video goggles may be used instead of Frenzel glasses. [Figure caption and citation for the preceding image starts]: Frenzel glassesFrom Jung I, Kim J-S. Approach to dizziness in the emergency department. Clin Exp Emerg Med. 2015 Jun 30; 2(2):75-88; used with permission [Citation ends].

Exam of dynamic visual acuity
This tests the vestibulo-ocular reflex by observing the effect of head rotation on visual acuity (e.g., by reading the letters on a Snellen chart).[115]
Abnormal results indicate a bilateral vestibular failure.
Observation of the eyes may lead to suspicion for other ophthalmological conditions, such as interstitial keratitis in Cogan syndrome or uveitis in Behcet disease.
Physical exam: clinical balance tests
The Dix-Hallpike test
This is the gold standard test for the diagnosis of posterior canal BPPV.[10]
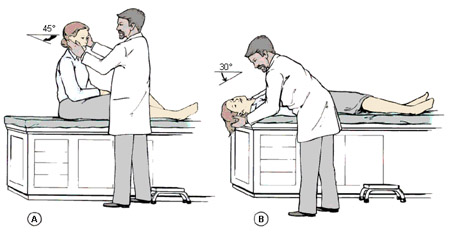
The test is performed with the patient sitting the upright on a bed; for the right side, the examiner stands on the patient’s right side, rotates the patient’s head 45 degrees to the right, and then moves the patient, whose eyes are open, to the supine right-ear down position, and then extends the patient’s neck slightly so that the chin points slightly upward. Patient's symptoms are noted and any nystagmus is observed. The test is repeated on the left with the examiner standing on the patient’s left side.[10]
Classically, the onset of peripheral nystagmus and symptoms is delayed by about 5 to 20 seconds. The provoked vertigo and nystagmus increase then resolve within 60 seconds.[10] The nystagmus fatigues on repeat testing, although this is not recommended because it unnecessarily subjects patients to further symptoms.[10]
BPPV is typically due to posterior canal pathology. If the pathology affects the horizontal canal, the nystagmus may be more persistent and less fatigable.
When symptoms are due to central pathology, the test causes nystagmus that is not fatigable, is down-beating, and is associated with minimal vertigo.
The Dix-Hallpike test has been shown to have a positive predictive value of 83% and a negative predictive value of 52% for the diagnosis of BPPV.[132][Figure caption and citation for the preceding image starts]: Dix-Hallpike maneuverParnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93; used with permission [Citation ends].
Supine lateral head turns
If the Dix-Hallpike test is negative in a patient who has a history suggestive of BPPV, perform supine lateral head turns to test for lateral semicircular canal BPPV.[10] Position the patient supine with the head in the neutral position, then quickly rotate the head 90 degrees to one side while observing the patient’s eyes for nystagmus. The head is returned to the face up position, allowing all dizziness and nystagmus to subside; the head is then turned rapidly to the opposite side.[10]
In most cases of lateral semicircular canal BPPV, there is intense horizontal nystagmus beating toward the undermost (affected) ear when the patient is rolled to the affected side. When the patient is rolled to the unaffected side, there is less intense horizontal nystagmus beating toward the undermost ear.[10]
Physical exam: central nervous system
Exam of the other cranial nerves
Facial nerve palsy may occur with cerebellopontine angle tumors, granulomatosis with polyangiitis (formerly known as Wegener’s granulomatosis) and cholesteatoma.
Dysarthria can be a sign of posterior circulation stroke, vertebrobasilar insufficiency or vertebral artery dissection.
Facial numbness may occur in posterior circulation stroke.
Loss of pain and temperature sensation of the ipsilateral face occurs in Wallenberg syndrome (lateral medullary infarction).[38]
Neurologic exam
Exam of cerebellar function is usually tested with the finger-to-nose test and rapid alternating hand movements.[131] This may be abnormal in cerebellar lesions.
Ipsilateral limb ataxia and loss of pain and temperature sensation of the contralateral trunk occurs in Wallenberg syndrome (lateral medullary infarction).[38]
Various neurologic signs may be present in people with multiple sclerosis (e.g., altered gait, weakness, nystagmus, cranial nerve palsies).
Signs of peripheral neuropathy may occur in patients with diabetes mellitus (e.g., numbness and presence of painless injuries).
Bizarre changes (e.g., "wooden soldier" or "scissor gait") may occur in psychogenic lesions.
Romberg and Unterberger (Fukuda) tests
Provides information about the patient's balance with the eyes closed.
Romberg test: the patient attempts to maintain a standing position with the feet together, eyes closed, and arms outstretched. The test is positive if the patient cannot maintain balance.
Unterberger test: the patient performs stationary stepping with eyes closed for up to 1 minute. A tendency to veer toward the affected side occurs after a unilateral vestibular loss.
These are nonspecific tests that can be abnormal in peripheral or central lesions.[115]
Patients with cerebellar infarction usually cannot stand without support, even with the eyes open, whereas a patient with acute vestibular neuritis or labyrinthitis can.
Physical exam: cardiovascular system and general exam
Cardiovascular exam
Check for an irregular pulse, which could indicate an arrhythmia.
Check lying and standing blood pressure (BP) and pulse should be checked in patients with postural symptoms. A fall in systolic BP of at least 20 mmHg or diastolic BP of at least 10 mmHg within 3 minutes of standing indicates orthostatic hypotension.[56]
Where postural symptoms resemble those of orthostatic hypotension, but orthostatic hypotension is not demonstrated, an increased heart rate on standing may indicate postural orthostatic tachycardia syndrome.[60]
Auscultate for carotid bruits and cardiac murmurs.
General exam may reveal evidence of other conditions (e.g., oral ulcers with Behcet disease; evidence of multisystem involvement with systemic lupus erythematosus).
Investigations: pure-tone audiogram
Demonstrates any associated hearing loss.
A unilateral sensorineural hearing loss may occur in labyrinthitis and Meniere disease (low frequency).
Unilateral or asymmetrical sensorineural hearing loss should prompt investigation for a posterior fossa tumor (e.g., acoustic neuroma).[114]
Investigations: imaging of the head
CT scan of the petrous temporal bones
A high-resolution thin-slice CT scan is useful in patients with suspected SCDS.[88][133]
Useful in the diagnosis of middle ear or mastoid disease. May be helpful to confirm cholesteatoma.[134]
Should be performed if temporal bone fracture is suspected.[135]
CT scan of the brain
Usual initial imaging investigation for patients with suspected acute stroke if the patient has had symptoms for fewer than six hours. Noncontrast CT detects intracranial hemorrhage and large infarcts, allowing the treating clinician to make management decisions quickly.[86][89]
The American Heart Association/American Stroke Association guidelines recommend that all patients admitted to hospital with suspected acute stroke should have brain imaging on arrival to hospital and in most cases, noncontrast CT will provide the necessary information to make decisions about acute management.[86]
The National Institute for Health and Care Excellence in the UK advises that patients with suspected acute stroke should have brain imaging with a noncontrast CT within one hour if any of the following apply:[87]
Indications for thrombolysis or thrombectomy
On anticoagulant treatment
Known bleeding tendency
Glasgow Coma Score below 13
Unexplained progressive or fluctuating symptoms
Papilledema, neck stiffness, or fever
Severe headache at onset of stroke symptoms
MRI of internal auditory meatus and brain
Contrast-enhanced MRI with MR angiography is recommended for patients who have a suspected acute stroke. MRI can determine the age of the infarct and evaluate other causes for the symptoms. It is more sensitive than CT for acute infarct.[88][89] If the patient has had stroke symptoms for less than six hours, noncontrast CT is often performed first.[89] If the patient has had stroke symptoms for longer than six hours, MRI is recommended as the initial investigation.[89] MRI can be performed without contrast for patients with renal failure or contrast allergy.[89]
Contrast-enhanced MRI is the investigation of choice for suspected posterior fossa tumors.[134]
Demonstrates malformations (e.g., Arnold-Chiari malformation type 1).
Demyelinating lesions may be seen on MRI in people with multiple sclerosis.
Advances in MRI techniques enable visualization of endolymphatic hydrops.[136]
MRI angiography may be performed in cases of suspected vertebrobasilar insufficiency (demonstrating occlusion of the cerebellar arteries), Wallenberg syndrome (demonstrating occlusion of the ipsilateral vertebral artery), or vertebral artery dissection.
Investigations: vestibular function tests
There are numerous tests available, such as electronystagmography (ENG), caloric testing, video head impulse test (vHIT), and vestibular evoked myogenic potentials.
The tests can be useful in cases of diagnostic uncertainty to demonstrate a unilateral or bilateral vestibular loss.
Typically, a directional preponderance (nystagmus greater in one direction than the other) of 26% to 30% indicates significant asymmetry, and a canal paresis (reduced function) of 22% to 25% indicates a unilateral vestibular loss.[115]
Computerized dynamic posturography testing: utilizes a computerized controlled platform and visual booth to evaluate sensory and motor components of balance.[131] The test results in 6 abnormal sensory patterns useful for clinical diagnosis and rehabilitation.
Rotatory chair testing: an adjunctive balance test that may be used if ENG is abnormal.
Electrocochleography: may be useful in the diagnosis of Meniere disease. The transtympanic test is a more invasive type of electrocochleography and is a more sensitive test than extra-tympanic electrocochleography.
Acoustic reflex assessment: involves exposing the patient to loud noise to observe the muscle that causes movement of the stapes to protect the ear. It is a secondary assessment of stapes function and would be abnormal in people with otosclerosis (pathological temporal bone remodeling) and normal in people with SCDS.
vHIT: this tests the vestibulo-ocular reflex of all the semicircular canals.[137]
Vestibular evoked myogenic potential: indicated only when SCDS is suspected.[138] In this case, increased amplitude may be demonstrated.[133]
Investigations: cardiovascular
ECG
Recommended in patients when a cardiac cause of dizziness is suspected.
How to perform an ECG: animated demonstrationHow to record an ECG. Demonstrates placement of chest and limb electrodes.
Echocardiography
May be useful for patients with syncope where cardiac pathology is suspected.[139]
Cardiac monitoring
Indicated in patients with presyncope where an arrhythmia is suspected.
Tilt-table testing
Further investigations in specific circumstances
Antinuclear antibodies, double-stranded DNA, Smith antigen if systemic lupus erythematosus is suspected.[141]
Antineutrophil cytoplasmic antibody (ANCA) and biopsy of lesions for histology if granulomatosis with polyangiitis [formerly known as Wegener granulomatosis] is suspected.
Treponemal antibody tests if syphilis infection is suspected.
Blood glucose monitoring and HbA1c in patients with diabetes mellitus who have dizzy episodes possibly related to hypoglycemia. A lower than expected HbA1c is suggestive but not diagnostic of hypoglycemic episodes. Self-monitored blood glucose levels are required for confirmation.
Blood glucose must be checked in all patients with a suspected stroke.[86]
Assess carboxyhemoglobin levels using a carbon monoxide oximeter in cases of suspected carbon monoxide poisoning.[108]
Serum drug levels may be appropriate if the symptoms are thought to be medication- or drug-related.
Slit-lamp ophthalmoscopic exam
Necessary if the diagnosis of Cogan syndrome is considered.
Exploratory tympanotomy
May be done to investigate the cause of postsurgical dizziness or when there is a suspected diagnosis of perilymphatic fistula.
Lumbar puncture and measurement of CSF pressure
Required to diagnose benign intracranial hypertension and normal pressure hydrocephalus.
Diagnostic lumbar puncture in adults: animated demonstrationHow to perform a diagnostic lumbar puncture in adults. Includes a discussion of patient positioning, choice of needle, and measurement of opening and closing pressure.
Cisternography
Performed to demonstrate the absence of obstruction of the cerebral aqueduct or of CSF outflow from the 4th ventricle in people with normal pressure hydrocephalus.
Use of this content is subject to our disclaimer

