Approach
The primary care physician will make the diagnosis in most cases of vitiligo. Only in atypical cases will the expertise of a dermatologist be required.[34]
History
The clinical evaluation is supported by history to exclude other genetic, inflammatory, or trauma-induced disorders. Evidence suggests enquiring about the following:[14]
Extent, duration, and spread of lesions
Potential triggers and risk factors (such as family history, trauma, use of chemical hair dyes, infection)
Previous episodes and treatments
A diagnosis of, or symptoms suggestive of, comorbid autoimmune disease.
Age younger than 30 years and a family history of vitiligo or related autoimmune diseases are strong risk factors for development of vitiligo.[1][6] Up to 20% of patients with vitiligo have at least one first-degree relative with the condition.[8][9]
Studies suggest a family history of autoimmune disorders in up to 20% of patients with vitiligo.[8][35][36] The disease most often associated with vitiligo is autoimmune thyroid disease.[31][30] Less commonly associated conditions include pernicious anemia, systemic lupus erythematosus, alopecia areata, type 1 diabetes, and Addison disease.
Physical exam
Perform a full skin exam with and without Wood lamp (see below) to determine subtype of disease, skin type, and disease severity measured by body surface area affected.
The hallmark of vitiligo is completely depigmented, rather than hypopigmented skin.
Exam of the whole skin may reveal involvement at any site, although the face, genitals, acral, and periorificial skin are most commonly affected. Three different levels of pigmentation may be observed in so-called trichrome vitiligo, in which a rim of hypopigmented epidermis typically surrounds completely achromic areas of skin.
Halo (Sutton) nevus is found 10 times more commonly in patients with vitiligo.[31]
Erythema, edema, and blistering of the affected areas from sunburn can also be presenting signs. Depigmentation may affect the epithelium of the retina and the choroid in up to 40% of patients, although true ocular symptoms are very rare. Uveitis is also an associated finding in patients with vitiligo.[37][Figure caption and citation for the preceding image starts]: Focal vitiligo on wristFrom Dr John E. Harris' personal collection [Citation ends]. [Figure caption and citation for the preceding image starts]: Typical periocular vitiligo with poliosis of several eyelashesPhotograph from the collection of Sarah Stein, MD, University of Chicago, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Typical periocular vitiligo with poliosis of several eyelashesPhotograph from the collection of Sarah Stein, MD, University of Chicago, used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Depigmentation of the handFrom Dr Bernhard Ortel's personal collection [Citation ends].
[Figure caption and citation for the preceding image starts]: Depigmentation of the handFrom Dr Bernhard Ortel's personal collection [Citation ends]. [Figure caption and citation for the preceding image starts]: Typical distribution of vitiligo: periungual skin, knuckles, and wristPhotograph from the collection of Sarah Stein, MD, University of Chicago, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Typical distribution of vitiligo: periungual skin, knuckles, and wristPhotograph from the collection of Sarah Stein, MD, University of Chicago, used with permission [Citation ends].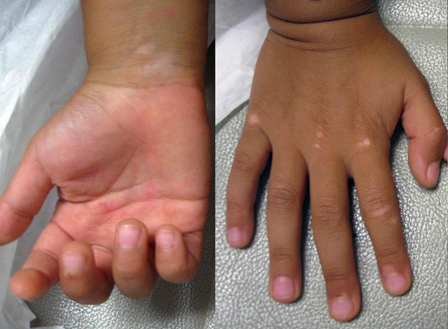 [Figure caption and citation for the preceding image starts]: Perianal and genital skin involvement in generalized vitiligoPhotograph from the collection of Sarah Stein, MD, University of Chicago, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Perianal and genital skin involvement in generalized vitiligoPhotograph from the collection of Sarah Stein, MD, University of Chicago, used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Trichrome vitiligo. There are areas of hypopigmentation between normal skin and depigmented skinFrom Dr John E. Harris' personal collection [Citation ends].
[Figure caption and citation for the preceding image starts]: Trichrome vitiligo. There are areas of hypopigmentation between normal skin and depigmented skinFrom Dr John E. Harris' personal collection [Citation ends]. [Figure caption and citation for the preceding image starts]: Classic appearance of a halo nevusFrom Dr John E. Harris' personal collection [Citation ends].
[Figure caption and citation for the preceding image starts]: Classic appearance of a halo nevusFrom Dr John E. Harris' personal collection [Citation ends]. [Figure caption and citation for the preceding image starts]: Halo of depigmentation around congenital nevus in black childPhotograph from the collection of Sarah Stein, MD, University of Chicago, used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Halo of depigmentation around congenital nevus in black childPhotograph from the collection of Sarah Stein, MD, University of Chicago, used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Distribution patterns in vitiligoFrom Dr Bernhard Ortel's personal collection [Citation ends].
[Figure caption and citation for the preceding image starts]: Distribution patterns in vitiligoFrom Dr Bernhard Ortel's personal collection [Citation ends].
Wood lamp exam
Wood lamp (black light) emits UV-A radiation (315-400 nm) with a peak at 365 nm and almost no visible light. Two criteria are helpful in diagnosing vitiligo:
Enhancement: due to the loss of epidermal pigment and the limited penetration depth of UV-A, Wood lamp accentuates the contrast between involved and uninvolved skin
Fluorescence: a distinctive bluish fluorescence that is seen in vitiligo but not in skin that is simply hypopigmented.[Figure caption and citation for the preceding image starts]: Accentuation of clinical features by Wood lamp examFrom Dr Bernhard Ortel's personal collection [Citation ends].

Laboratory investigations
The association between vitiligo and autoimmune thyroiditis is relatively common. Clinical evaluation for thyroid disease should be done in all patients, but routine screening for thyroid dysfunction in patients with no symptoms of thyroid disease is not recommended.[38]
Serologic testing for other conditions is of limited value in the diagnosis of vitiligo.
Skin biopsy
A skin biopsy is rarely needed to make the diagnosis of vitiligo.
Fontana-Masson stain highlights melanin pigment in the epidermis, although melanocytes are best identified using special stains.
Dihydroxy-phenylalanine stain of frozen sections may reveal unpigmented melanocytes by showing tyrosinase activity.
Use of this content is subject to our disclaimer