History and exam
Key diagnostic factors
common
single or multiple scaly macules or plaques
Most commonly, lesions are pink, skin-colored, or yellowish, ill-defined, irregularly shaped, small (1 to 5 mm), rough, scaly macules or plaques, on sun-exposed areas of skin. [Figure caption and citation for the preceding image starts]: Regular actinic keratosisFrom the collection of the Department of Dermatology and Cutaneous Surgery, University of Miami Miller School of Medicine [Citation ends].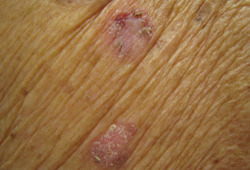
scaly lesions with a hyperkeratotic surface
May present as a hyperkeratotic lesion. [Figure caption and citation for the preceding image starts]: Hyperkeratotic actinic keratosisFrom the collection of the Department of Dermatology and Cutaneous Surgery, University of Miami Miller School of Medicine [Citation ends].
well-defined, scaly, brown lesions
Pigmented AKs resemble solar lentigo.[1]
lesions resembling seborrheic keratosis, melanocytic nevus, and early malignant melanoma
Spreading pigmented AKs may occur.[5]
hypertrophic conical-shaped protuberances growing from the surface of the skin
Typical of a cutaneous horn.
scaly red roughness with induration, fissuring, and ulceration of the lower lip and the vermilion border
lesion on sun-exposed area of body
The forehead, bald areas of the scalp, ears, lower lip, and dorsum of the hands and forearms are the most common anatomic areas involved.[38]
uncommon
skin-colored, papillomatous, elevated wartlike papules
Typical of verrucous AKs.
plaques with very mild scale over very thin shiny skin
Typical of atrophic AKs.
violaceous well-defined papules with fine white lines on the surface
Typical of lichen planus-like or lichenoid AKs.
Other diagnostic factors
common
evidence of sun damage to skin
Solar elastosis, cutaneous furrowing, and wrinkles are more likely to be present in sun-exposed areas.[4]
uncommon
pruritus or bleeding
Mild pruritus may be present.
Bleeding may occur if lesions are scratched.
Risk factors
strong
chronic exposure to UVB radiation
Causes damage to keratinocyte DNA, and induces mutations on the tumor suppressor gene p53, leading to the perpetuation and clonal expansion of keratinocytes with damaged DNA.[31][36][37]
More than 80% of AKs are located on the head and neck, and on the dorsum of forearms and hands (chronic UV-exposed areas).[38]
There is an inverse risk of developing AKs with latitude; risk decreases with increasing distance from the equator (latitude 0°).[39][40]
light-colored skin, freckling, and albinism
Melanin absorbs UVB rays to help protect human skin from developing AKs.[28][30] People with light-colored skin (Fitzpatrick skin types I and II) are 6 times more likely to develop AKs than darker skin types.[22] Freckling in childhood leads to increased risk for developing AKs.[16][17][41]
After acute sun exposure, patients who burn without tanning are twice as likely to develop AKs as those who tan without burning.[22]
The incidence of AKs in people with albinism >20 years old is 91%.[15][16][17][42]
age >40 years
immunocompromise
Use of this content is subject to our disclaimer
