LCH covers a wide range of clinical presentations and may affect any organ or system of the body.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
The aim of the initial evaluation is to define the extent of the disease: that is, to determine whether the disease is single-system or multisystem, and identify which organs are involved.
Clinical manifestations: general considerations
A careful history should be taken, bearing in mind that some manifestations (e.g., skin rash, polyuria, polydipsia) may have started months, or even years, before the initial presentation.[4]Goyal G, Tazi A, Go RS, et al. International expert consensus recommendations for the diagnosis and treatment of Langerhans cell histiocytosis in adults. Blood. 2022 Apr 28;139(17):2601-21.
https://ashpublications.org/blood/article/139/17/2601/484364/International-expert-consensus-recommendations-for
http://www.ncbi.nlm.nih.gov/pubmed/35271698?tool=bestpractice.com
The clinician should enquire about symptoms of:[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
Pain
Swelling
Skin rash
Fever
Loss of appetite
Faltering growth
Poor weight gain
Diarrhea
Otorrhea
Polydipsia
Polyuria
Respiratory symptoms
Irritability
Neurologic changes
Behavioral changes.
History of smoking should be elicited, because it increases the risk of lung involvement in adolescents and adults.[23]Bernstrand C, Cederlund K, Sandstedt B, et al. Pulmonary abnormalities at long-term follow-up of patients with Langerhans cell histiocytosis. Med Pediatr Oncol. 2001 Apr;36(4):459-68.
http://www.ncbi.nlm.nih.gov/pubmed/11260569?tool=bestpractice.com
A history of trauma to the skin or bone should be noted to help rule out other causes of the presenting symptoms.
Single-system disease involves one organ system only. Approximately 70% of patients ages <15 years have single-system disease, most commonly with bone involvement.[10]Stuurman KE, Lau L, Doda W, et al. Evaluation of the natural history and long term complications of patients with Langerhans cell histiocystosis of bone. Proceedings of the XIX meeting of the Histiocyte Society. Philadelphia, PA: Histiocyte Society; 2003.
Multisystem disease occurs in two or more organs.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
Most adults have multisystem disease, commonly with skin and lung involvement.[12]Arico M, Girschikofsky M, Genereau T, et al. Langerhans cell histiocytosis in adults. Report from the International Registry of the Histiocyte Society. Eur J Cancer. 2003 Nov;39(16):2341-8.
http://www.ncbi.nlm.nih.gov/pubmed/14556926?tool=bestpractice.com
Multisystem disease with bone marrow involvement is also very common in children ages <2 years.[25]Gadner H, Grois N, Pötschger U, et al. Improved outcome in multisystem Langerhans cell histiocytosis is associated with therapy intensification. Blood. 2008 Mar 1;111(5):2556-62.
https://ashpublications.org/blood/article/111/5/2556/109907/Improved-outcome-in-multisystem-Langerhans-cell
http://www.ncbi.nlm.nih.gov/pubmed/18089850?tool=bestpractice.com
Specific organs are considered high-risk in children because the associated mortality rates in those who do not respond to treatment are high. High-risk organs include the liver, spleen, and bone marrow.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
On physical exam, height and weight percentiles should be measured and recorded. A full ear, nose, and throat and dental/mouth evaluation should be performed, as well as an examination of other mucocutaneous junctions including the anal and vaginal areas. The whole body should be examined for the presence of skin rashes, bone lesions, and soft-tissue masses. A complete neurologic exam should also be performed.
Clinical manifestations: bone involvement
The most common type of single-system disease in children, but may also be present in multisystem disease. Bone lesions are present in 80% of patients, most commonly on the scalp.[10]Stuurman KE, Lau L, Doda W, et al. Evaluation of the natural history and long term complications of patients with Langerhans cell histiocystosis of bone. Proceedings of the XIX meeting of the Histiocyte Society. Philadelphia, PA: Histiocyte Society; 2003. Lytic osseous lesions are seen in 30% to 50% of adults, and can occur as single-system or multisystem disease.[12]Arico M, Girschikofsky M, Genereau T, et al. Langerhans cell histiocytosis in adults. Report from the International Registry of the Histiocyte Society. Eur J Cancer. 2003 Nov;39(16):2341-8.
http://www.ncbi.nlm.nih.gov/pubmed/14556926?tool=bestpractice.com
Pain and/or swelling in the affected area(s) are common. The most common site of swelling is over the skull bones and this is usually painless. The lesions may be unifocal (single bone) or multifocal (>1 bone), and approximately 50% of bone lesions are asymptomatic and are only revealed on an x-ray.[10]Stuurman KE, Lau L, Doda W, et al. Evaluation of the natural history and long term complications of patients with Langerhans cell histiocystosis of bone. Proceedings of the XIX meeting of the Histiocyte Society. Philadelphia, PA: Histiocyte Society; 2003.[26]Kilpatrick SE, Wenger DE, Gilchrist GS, et al. Langerhans' cell histiocytosis (Histiocytosis X) of bone. A clinicopathologic analysis of 263 pediatric and adult cases. Cancer. 1995 Dec 15;76(12):2471-84.
https://acsjournals.onlinelibrary.wiley.com/doi/epdf/10.1002/1097-0142%2819951215%2976%3A12%3C2471%3A%3AAID-CNCR2820761211%3E3.0.CO%3B2-Z
http://www.ncbi.nlm.nih.gov/pubmed/8625073?tool=bestpractice.com
LCH is the most common cause of vertebra plana (i.e., spondylitis with reduction of the vertebral body to a thin disk) in children. This leads to compression and collapse of the vertebral body. Neurologic complications may arise from extension of Langerhans cells into the extradural space. Pathologic fractures are rare.
Central nervous system (CNS)-risk bones are bones in which, if lesions are present, patients have a 3-fold higher risk of developing CNS disease in children (the most common manifestation being diabetes insipidus). These bones are the facial bones or bones of the anterior/middle cranial fossa (i.e., temporal, sphenoidal, ethmoidal, zygomatic, and orbital bones).[27]Grois N, Potschger U, Prosch H, et al. Risk factors for diabetes insipidus in Langerhans cell histiocytosis. Pediatr Blood Cancer. 2006 Feb;46(2):228-33.
http://www.ncbi.nlm.nih.gov/pubmed/16047354?tool=bestpractice.com
Clinical manifestations: skin involvement
A common type of single-system disease in children, but may also be present in multisystem disease, especially in neonates.[28]Lau L, Krafchik B, Trebo MM, et al. Cutaneous Langerhans cell histiocytosis in children under one year. Pediatr Blood Cancer. 2006 Jan;46(1):66-71.
http://www.ncbi.nlm.nih.gov/pubmed/16261594?tool=bestpractice.com
Skin is the second most commonly involved organ in the pediatric group, and skin lesions are present in up to 50% of patients, usually on the scalp.[29]Munn S, Chu AC. Langerhans cell histiocytosis of the skin. Hematol Oncol Clin North Am. 1998 Apr;12(2):269-86.
http://www.ncbi.nlm.nih.gov/pubmed/9561900?tool=bestpractice.com
The most common lesion in the first few months of life is a papulosquamous rash that affects the scalp, skin folds, and midline of the trunk. This is easily mistaken for seborrheic dermatitis (or cradle cap in infants) or possibly a Candida infection.[30]Poompuen S, Chaiyarit J, Techasatian L. Diverse cutaneous manifestation of Langerhans cell histiocytosis: a 10-year retrospective cohort study. Eur J Pediatr. 2019 May;178(5):771-6.
http://www.ncbi.nlm.nih.gov/pubmed/30826864?tool=bestpractice.com
[31]National Organization for Rare Disorders. Langerhans cell histiocytosis. 2021 [internet publication].
https://rarediseases.org/rare-diseases/langerhans-cell-histiocytosis
A single or multiple violaceous papulonodular, and sometimes vesicular, rash may also occur, but is rare and may disappear spontaneously. This is known as Hashimoto-Pritzker disease.[32]Hashimoto K, Bale GF, Hawkins HK, et al. Congenital self-healing reticulohistiocytosis (Hashimoto-Pritzker type). Int J Dermatol. 1986 Oct;25(8):516-23.
http://www.ncbi.nlm.nih.gov/pubmed/3533803?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Langerhans cell histiocytosis rash on an infant's abdomenReproduced with permission from Science Photo Library [Citation ends].
Among adults, isolated skin involvement is less common, and mostly seen as a part of multisystem disease (30% to 50%).[12]Arico M, Girschikofsky M, Genereau T, et al. Langerhans cell histiocytosis in adults. Report from the International Registry of the Histiocyte Society. Eur J Cancer. 2003 Nov;39(16):2341-8.
http://www.ncbi.nlm.nih.gov/pubmed/14556926?tool=bestpractice.com
Perianal or genital involvement is more common in adults, and can be very disabling and resistant to treatment.[33]Hamdan M, Qiao JC, Fikfak V. Adult-onset perianal Langerhans cell histiocytosis presenting as pruritus ani: a case report and review of the literature. J Med Case Rep. 2021 Jul 22;15(1):357.
https://jmedicalcasereports.biomedcentral.com/articles/10.1186/s13256-021-02924-0
http://www.ncbi.nlm.nih.gov/pubmed/34289900?tool=bestpractice.com
Clinical manifestations: lung involvement
An uncommon type of single-system disease in children, but often present in multisystem disease, especially in infants. It occurs in 15% of children; however, it is more common in adults (40% to 50%), especially heavy smokers.[34]Suri HS, Yi ES, Nowakowski GS, et al. Pulmonary Langerhans cell histiocytosis. Orphanet J Rare Dis. 2012 Mar 19;7:16.
https://ojrd.biomedcentral.com/articles/10.1186/1750-1172-7-16
http://www.ncbi.nlm.nih.gov/pubmed/22429393?tool=bestpractice.com
Patients commonly present with cough or dyspnea.[35]Vassallo R, Ryu JH, Schroeder DR, et al. Clinical outcomes of pulmonary Langerhans'-cell histiocytosis in adults. N Engl J Med. 2002 Feb 14;346(7):484-90.
https://www.nejm.org/doi/full/10.1056/NEJMoa012087
http://www.ncbi.nlm.nih.gov/pubmed/11844849?tool=bestpractice.com
A minority of patients report malaise, fatigue, fever, or weight loss. Chest pain may indicate a spontaneous pneumothorax.[35]Vassallo R, Ryu JH, Schroeder DR, et al. Clinical outcomes of pulmonary Langerhans'-cell histiocytosis in adults. N Engl J Med. 2002 Feb 14;346(7):484-90.
https://www.nejm.org/doi/full/10.1056/NEJMoa012087
http://www.ncbi.nlm.nih.gov/pubmed/11844849?tool=bestpractice.com
Clinical manifestations: CNS involvement
A common type of single-system disease, but CNS involvement may also be present in multisystem disease.
Diabetes insipidus is the most common manifestation, due to posterior pituitary gland involvement. It is more common in patients with multisystem disease and those with craniofacial bone lesions, especially of the orbit and skull base.[27]Grois N, Potschger U, Prosch H, et al. Risk factors for diabetes insipidus in Langerhans cell histiocytosis. Pediatr Blood Cancer. 2006 Feb;46(2):228-33.
http://www.ncbi.nlm.nih.gov/pubmed/16047354?tool=bestpractice.com
The risk is high in patients when the disease has been active for a long period of time, or when the disease is reactivated. These patients generally present with polyuria and polydipsia. Patients may also present with headache, faltering growth, or delayed puberty.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
Among children, those with mastoid, temporal, and orbital bone lesions and diabetes insipidus are at increased risk of developing a CNS neurodegenerative syndrome. This occurs in up to 4% of patients and manifests as ataxia, dysmetria, and dysarthria.[3]Allen CE, Merad M, McClain KL. Langerhans-cell histiocytosis. N Engl J Med. 2018 Aug 30;379(9):856-68.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6334777
http://www.ncbi.nlm.nih.gov/pubmed/30157397?tool=bestpractice.com
[36]Yeh EA, Greenberg J, Abla O, et al; North American Consortium for Histiocytosis. Evaluation and treatment of Langerhans cell histiocytosis patients with central nervous system abnormalities: current views and new vistas. Pediatr Blood Cancer. 2018 Jan;65(1):e26784.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.26784
http://www.ncbi.nlm.nih.gov/pubmed/28944988?tool=bestpractice.com
The patient may also present with seizures, focal neurologic deficits, cognitive impairment, changes in behavior, or progressive cerebellar symptoms such as nystagmus, dysarthria, and hypotonia.[3]Allen CE, Merad M, McClain KL. Langerhans-cell histiocytosis. N Engl J Med. 2018 Aug 30;379(9):856-68.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6334777
http://www.ncbi.nlm.nih.gov/pubmed/30157397?tool=bestpractice.com
[37]Barthez MA, Araujo E, Donadieu J. Langerhans cell histiocytosis and the central nervous system in childhood: evolution and prognostic factors. Results of a collaborative study. J Child Neurol. 2000 Mar;15(3):150-6.
http://www.ncbi.nlm.nih.gov/pubmed/10757469?tool=bestpractice.com
Clinical manifestations: lymph node involvement
This is usually part of multisystem disease, but can also occur in isolation, or is sometimes associated with a single bone lesion.[38]Edelweiss M, Medeiros LJ, Suster S, et al. Lymph node involvement by Langerhans cell histiocytosis: a clinicopathologic and immunohistochemical study of 20 cases. Hum Pathol. 2007 Oct;38(10):1463-9.
http://www.ncbi.nlm.nih.gov/pubmed/17669469?tool=bestpractice.com
[39]Kakkar S, Kapila K, Verma K. Langerhans cell histiocytosis in lymph nodes. Cytomorphologic diagnosis and pitfalls. Acta Cytol. 2001 May-Jun;45(3):327-32.
http://www.ncbi.nlm.nih.gov/pubmed/11393062?tool=bestpractice.com
It may affect single or multiple lymph nodes. Lymphadenopathy is seen on exam. Superior vena cava syndrome can result from mediastinal lymph node or thymic enlargement.[40]Mogul M, Hartman G, Donaldson S, et al. Langerhans' cell histiocytosis presenting with the superior vena cava syndrome: a case report. Med Pediatr Oncol. 1993;21(6):456-9.
http://www.ncbi.nlm.nih.gov/pubmed/8515729?tool=bestpractice.com
Careful analysis of phenotype and histopathology is recommended to differentiate reactive Langerhans cells in LCH from primary malignant histiocytosis of the lymph node.
Clinical manifestations: liver/spleen involvement
This is more common in multisystem disease. It affects 10% to 20% of patients with LCH.[41]Ziogas IA, Kakos CD, Wu WK, et al. Liver transplantation for Langerhans cell histiocytosis: a US population-based analysis and systematic review of the literature. Liver Transpl. 2021 Aug;27(8):1181-90.
http://www.ncbi.nlm.nih.gov/pubmed/33484600?tool=bestpractice.com
Chronic liver disease in these patients is typically sclerosing cholangitis, which can progress to biliary cholangitis and sometimes to fatal liver failure.[41]Ziogas IA, Kakos CD, Wu WK, et al. Liver transplantation for Langerhans cell histiocytosis: a US population-based analysis and systematic review of the literature. Liver Transpl. 2021 Aug;27(8):1181-90.
http://www.ncbi.nlm.nih.gov/pubmed/33484600?tool=bestpractice.com
Hepatosplenomegaly is seen on exam, and patients may have jaundice or ascites.[42]Leung AKC, Lam JM, Leong KF. Childhood Langerhans cell histiocytosis: a disease with many faces. World J Pediatr. 2019 Dec;15(6):536-45.
http://www.ncbi.nlm.nih.gov/pubmed/31456157?tool=bestpractice.com
The liver and spleen are considered high-risk organs.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
Clinical manifestations: bone marrow involvement
This is more common in multisystem disease. Most patients are young children presenting with cytopenias (i.e., neutropenia, anemia, or thrombocytopenia) and diffuse disease in the skin, liver, spleen, and lymph nodes.[43]McClain K, Ramsay NK, Robison L, et al. Bone marrow involvement in histiocytosis X. Med Pediatr Oncol. 1983;11(3):167-71.
http://www.ncbi.nlm.nih.gov/pubmed/6602270?tool=bestpractice.com
Bone marrow is considered a high-risk organ.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
Involvement is a major component of the most severe forms of disease and is present in 70% of pediatric patients who die from LCH.[44]Willis B, Ablin A, Weinberg V, et al. Disease course and late sequelae of Langerhans' cell histiocytosis: 25-year experience at the University of California, San Francisco. J Clin Oncol. 1996 Jul;14(7):2073-82.
http://www.ncbi.nlm.nih.gov/pubmed/8683239?tool=bestpractice.com
In adults, presence of peripheral blood count abnormalities may suggest bone marrow infiltration by LCH or another myeloid neoplasm.
Clinical manifestations: other organ systems
Eye involvement
More common in multisystem disease.
Seen in 14% of children, and generally presents with visual disturbances, such as diplopia.[45]Nanduri V, Titgemeyer C, Brock P. Long term outcome of orbital involvement in Langerhans' cell histiocytosis. In: Proceedings of the XVII meeting of the Histiocyte Society. Stresa, Italy; 2001:176. Intrinsic eye involvement is exceptional.
Patients may also present with proptosis, periorbital swelling and erythema, diplopia, or ophthalmoplegia.[46]Lakatos K, Sterlich K, Pötschger U, et al. Langerhans cell histiocytosis of the orbit: spectrum of clinical and imaging findings. J Pediatr. 2021 Mar;230:174-81;e1.
http://www.ncbi.nlm.nih.gov/pubmed/33157073?tool=bestpractice.com
Orbital disease must be differentiated from acute infection, inflammatory pseudotumor, rhabdomyosarcoma, and metastatic neuroblastoma.
Ear involvement
More common in multisystem disease.
The presence of otitis externa can be due to extension of the skin rash into the ear canal and secondary infection with Pseudomonas aeruginosa.[47]McCullough WP, Pollock AN. Langerhans cell histiocytosis presenting as chronic otitis externa. Pediatr Emerg Care. 2017 Jan;33(1):67-9.
http://www.ncbi.nlm.nih.gov/pubmed/28045847?tool=bestpractice.com
Ear pain is a typical symptom.
Middle ear involvement can occur secondary to lesions in the petrous temporal or mastoid bones, causing intermittent ear discharge.[48]Guo Y, Ning F, Wang G, et al. Retrospective study of Langerhans cell histiocytosis in ear, nose and neck. Am J Otolaryngol. 2020 Mar-Apr;41(2):102369.
http://www.ncbi.nlm.nih.gov/pubmed/31870640?tool=bestpractice.com
Perforation of tympanic membranes can also occur.
Inner ear involvement can present with deafness, or with behavioral disturbances in younger children.[49]Nanduri VR, Pritchard J, Chong WK, et al. Labyrinthine involvement in Langerhans' cell histiocytosis. Int J Pediatr Otorhinolaryngol. 1998 Nov 15;46(1-2):109-15.
http://www.ncbi.nlm.nih.gov/pubmed/10190711?tool=bestpractice.com
Oral involvement
More common in multisystem disease.
Oral lesions are uncommon but may precede the onset of disease in other parts of the body. Gingival hypertrophy and ulcers of the palate, tongue, or lips may be seen.[50]Neves-Silva R, Fernandes DT, Fonseca FP, et al. Oral manifestations of Langerhans cell histiocytosis: a case series. Spec Care Dentist. 2018 Nov;38(6):426-33.
http://www.ncbi.nlm.nih.gov/pubmed/30207399?tool=bestpractice.com
Other
Gastrointestinal involvement is more common in multisystem disease, and bloody diarrhea is the most common presenting symptom.[51]Egeler RM, Schipper ME, Heymans HS. Gastrointestinal involvement in Langerhans' cell histiocytosis (Histiocytosis X): a clinical report of three cases. Eur J Pediatr. 1990 Feb;149(5):325-9.
http://www.ncbi.nlm.nih.gov/pubmed/2178934?tool=bestpractice.com
Patients may present with massive thyroid enlargement; however, this is rare.[52]Burnett A, Carney D, Mukhopadhyay S, et al. Thyroid involvement with Langerhans cell histiocytosis in a 3-year-old male. Pediatr Blood Cancer. 2008 Mar;50(3):726-7.
http://www.ncbi.nlm.nih.gov/pubmed/16944476?tool=bestpractice.com
Investigations
Initial investigations: children
A complete blood count (CBC) should be ordered to check for the presence of cytopenias, which may indicate bone marrow involvement.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
Liver function tests (LFTs), serum albumin, serum creatinine, blood urea nitrogen (BUN), electrolytes, erythrocyte sedimentation rate, and coagulation studies should be ordered in all patients to screen for organ involvement, assess degree of systemic inflammation, and establish baseline measurements.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
Subsequent investigations: children
Early morning urine specific gravity and osmolality (following an overnight fast), blood electrolytes, and water deprivation test are indicated in children if there is a history of polydipsia or polyuria, to detect central diabetes insipidus.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
Additional pituitary function testing (e.g., follicle-stimulating hormone [FSH], luteinizing hormone [LH], testosterone or estradiol, corticotropin and morning cortisol, thyrotropin and free thyroxine, prolactin, and insulin-like growth factor 1) may be indicated if another endocrine abnormality is suspected.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
Pulmonary function tests should be performed in patients with pulmonary involvement. Bronchoalveolar lavage and lung biopsy are reserved for cases where the diagnosis is uncertain.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
An echocardiogram is indicated in patients with pulmonary LCH to rule out pulmonary hypertension.
Audiometry is indicated in patients with suspected ear involvement.
Liver imaging and/or biopsy may be indicated if LFTs are abnormal (transaminases or bilirubin >5 times the upper limit of normal); consult a hepatologist for advice.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
Gastrointestinal endoscopy and/or biopsy may be considered for children with unexplained chronic diarrhea, evidence of malabsorption, or faltering growth.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
Neuropsychometric assessment is indicated for children with neurologic abnormalities.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
Initial investigations: adults
A CBC with differential should be ordered initially in all patients to check for the presence of cytopenias, which may indicate bone marrow involvement with LCH or a concomitant myeloid neoplasm.[53]Goyal G, Young JR, Koster MJ, et al. The Mayo Clinic Histiocytosis Working Group consensus statement for the diagnosis and evaluation of adult patients with histiocytic neoplasms: Erdheim-Chester disease, Langerhans cell histiocytosis, and Rosai-Dorfman disease. Mayo Clin Proc. 2019 Oct;94(10):2054-71.
https://www.mayoclinicproceedings.org/article/S0025-6196(19)30273-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/31472931?tool=bestpractice.com
LFTs, serum creatinine, BUN, electrolytes, calcium, and inflammatory markers should be ordered in all patients to screen for organ involvement and establish baseline measurements.[53]Goyal G, Young JR, Koster MJ, et al. The Mayo Clinic Histiocytosis Working Group consensus statement for the diagnosis and evaluation of adult patients with histiocytic neoplasms: Erdheim-Chester disease, Langerhans cell histiocytosis, and Rosai-Dorfman disease. Mayo Clin Proc. 2019 Oct;94(10):2054-71.
https://www.mayoclinicproceedings.org/article/S0025-6196(19)30273-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/31472931?tool=bestpractice.com
[54]Girschikofsky M, Arico M, Castillo D, et al. Management of adult patients with Langerhans cell histiocytosis: recommendations from an expert panel on behalf of Euro-Histio-Net. Orphanet J Rare Dis. 2013 May 14;8:72.
https://ojrd.biomedcentral.com/articles/10.1186/1750-1172-8-72
http://www.ncbi.nlm.nih.gov/pubmed/23672541?tool=bestpractice.com
BRAF V600E mutation analysis should be performed on tissue biopsy where available. For cases that are negative for BRAF V600E, next-generation sequencing studies for mitogen-activated protein kinase/extracellular signal-regulated kinase (MAPK-ERK) pathway mutations should be conducted on tissue biopsy specimens.[4]Goyal G, Tazi A, Go RS, et al. International expert consensus recommendations for the diagnosis and treatment of Langerhans cell histiocytosis in adults. Blood. 2022 Apr 28;139(17):2601-21.
https://ashpublications.org/blood/article/139/17/2601/484364/International-expert-consensus-recommendations-for
http://www.ncbi.nlm.nih.gov/pubmed/35271698?tool=bestpractice.com
[53]Goyal G, Young JR, Koster MJ, et al. The Mayo Clinic Histiocytosis Working Group consensus statement for the diagnosis and evaluation of adult patients with histiocytic neoplasms: Erdheim-Chester disease, Langerhans cell histiocytosis, and Rosai-Dorfman disease. Mayo Clin Proc. 2019 Oct;94(10):2054-71.
https://www.mayoclinicproceedings.org/article/S0025-6196(19)30273-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/31472931?tool=bestpractice.com
Endocrine evaluations are recommended in all adult patients with newly diagnosed LCH to detect pituitary involvement, especially in the presence of polyuria and polydipsia. These include: morning urine and serum osmolality to detect diabetes insipidus; FSH and LH; testosterone or estradiol; corticotropin and morning cortisol; thyrotropin and free thyroxine; prolactin; and insulin-like growth factor 1.[53]Goyal G, Young JR, Koster MJ, et al. The Mayo Clinic Histiocytosis Working Group consensus statement for the diagnosis and evaluation of adult patients with histiocytic neoplasms: Erdheim-Chester disease, Langerhans cell histiocytosis, and Rosai-Dorfman disease. Mayo Clin Proc. 2019 Oct;94(10):2054-71.
https://www.mayoclinicproceedings.org/article/S0025-6196(19)30273-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/31472931?tool=bestpractice.com
Imaging
Initial imaging: children
Skeletal radiograph survey is recommended to detect bone lesions.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
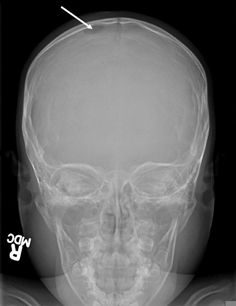
The classical appearance on x-ray is a punched-out lytic lesion, most commonly in the skull, with sharply demarcated margins, and little or no periosteal reaction.[55]Azouz EM, Saigal G, Rodriguez MM, et al. Langerhans' cell histiocytosis: pathology, imaging and treatment of skeletal involvement. Pediatr Radiol. 2005 Feb;35(2):103-15.
http://www.ncbi.nlm.nih.gov/pubmed/15289942?tool=bestpractice.com
Commonly, there is an associated mass that can extend intracranially and may cause brain compression. By contrast, lesions involving the orbit, mastoid, or other areas of the skull base are often extensive and irregular, with a soft-tissue component that must be differentiated from a malignant tumor.[55]Azouz EM, Saigal G, Rodriguez MM, et al. Langerhans' cell histiocytosis: pathology, imaging and treatment of skeletal involvement. Pediatr Radiol. 2005 Feb;35(2):103-15.
http://www.ncbi.nlm.nih.gov/pubmed/15289942?tool=bestpractice.com
Lesions in long bones may present with aggressive features and poorly defined borders, with or without a large soft-tissue mass that must also be distinguished from malignancy.[55]Azouz EM, Saigal G, Rodriguez MM, et al. Langerhans' cell histiocytosis: pathology, imaging and treatment of skeletal involvement. Pediatr Radiol. 2005 Feb;35(2):103-15.
http://www.ncbi.nlm.nih.gov/pubmed/15289942?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Skull x-ray showing lytic bone lesion in the right posterior parietal area of the skullFrom the personal collection of Oussama Abla, MD; used with permission [Citation ends].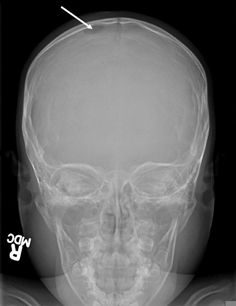
A chest x-ray should be performed to detect lung involvement.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
On chest x-ray, cysts may be visible within the infiltrates, predominating in the middle and upper lung fields, and sparing the costophrenic angles.[56]Lacronique J, Roth C, Battesti JP, et al. Chest radiological features of pulmonary histiocytosis X: a report based on 50 adult cases. Thorax. 1982 Feb;37(2):104-9.
https://thorax.bmj.com/content/thoraxjnl/37/2/104.full.pdf
http://www.ncbi.nlm.nih.gov/pubmed/6979115?tool=bestpractice.com
Pneumothorax, or a lytic lesion in a rib, may also be visible.
Abdominal ultrasound should be performed to assess the size and structure of the liver and spleen, and evaluate the intra-abdominal lymph nodes.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
Subsequent imaging: children
A high-resolution computed tomography (CT) scan of the lung is indicated for patients with pulmonary symptoms or abnormal chest x-ray. In children with known multisystem LCH, low-dose CT is sufficient to assess lung involvement and minimizes radiation exposure.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
A magnetic resonance imaging (MRI) scan of the head should be requested for children with suspected craniofacial bone lesions (including the mandible and maxilla). MRI may characterize the bony lesions and detect involvement of the brain and pituitary gland.[57]Porto L, Schöning S, Hattingen E, et al. Central nervous system imaging in childhood Langerhans cell histiocytosis - a reference center analysis. Radiol Oncol. 2015 Sep;49(3):242-9.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4577220
http://www.ncbi.nlm.nih.gov/pubmed/26401129?tool=bestpractice.com
MRI head should also be performed for patients with visual, neurologic, or suspected endocrine abnormalities.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
CT of an affected craniofacial bone and the skull base should be performed if MRI is unavailable.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
CT is useful to delineate uncertain lesions on skull x-ray, particularly if orbital, ear, or mastoid involvement is suspected. Contrast images will demarcate the soft-tissue involvement and periosteal reaction.
MRI spine should be performed in all pediatric patients with suspected vertebral lesions to exclude spinal cord compression and detect any soft-tissue masses.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
Initial imaging: adults
Full-body (vertex to toes) fluorodeoxyglucose positron emission tomography (FDG-PET) is recommended to stage disease and determine a suitable biopsy site. FDG-PET uptake is increased in regions affected by LCH.[53]Goyal G, Young JR, Koster MJ, et al. The Mayo Clinic Histiocytosis Working Group consensus statement for the diagnosis and evaluation of adult patients with histiocytic neoplasms: Erdheim-Chester disease, Langerhans cell histiocytosis, and Rosai-Dorfman disease. Mayo Clin Proc. 2019 Oct;94(10):2054-71.
https://www.mayoclinicproceedings.org/article/S0025-6196(19)30273-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/31472931?tool=bestpractice.com
MRI head with gadolinium contrast is performed to detect CNS involvement among patients with neurologic symptoms or symptoms suggestive of pituitary dysfunction.[53]Goyal G, Young JR, Koster MJ, et al. The Mayo Clinic Histiocytosis Working Group consensus statement for the diagnosis and evaluation of adult patients with histiocytic neoplasms: Erdheim-Chester disease, Langerhans cell histiocytosis, and Rosai-Dorfman disease. Mayo Clin Proc. 2019 Oct;94(10):2054-71.
https://www.mayoclinicproceedings.org/article/S0025-6196(19)30273-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/31472931?tool=bestpractice.com
High-resolution CT chest is indicated for suspected pulmonary LCH.[53]Goyal G, Young JR, Koster MJ, et al. The Mayo Clinic Histiocytosis Working Group consensus statement for the diagnosis and evaluation of adult patients with histiocytic neoplasms: Erdheim-Chester disease, Langerhans cell histiocytosis, and Rosai-Dorfman disease. Mayo Clin Proc. 2019 Oct;94(10):2054-71.
https://www.mayoclinicproceedings.org/article/S0025-6196(19)30273-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/31472931?tool=bestpractice.com
Subsequent imaging: adults
Organ-specific imaging (CT or MRI) may be needed in addition to the FDG-PET imaging to better assess structural changes associated with the disease.[53]Goyal G, Young JR, Koster MJ, et al. The Mayo Clinic Histiocytosis Working Group consensus statement for the diagnosis and evaluation of adult patients with histiocytic neoplasms: Erdheim-Chester disease, Langerhans cell histiocytosis, and Rosai-Dorfman disease. Mayo Clin Proc. 2019 Oct;94(10):2054-71.
https://www.mayoclinicproceedings.org/article/S0025-6196(19)30273-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/31472931?tool=bestpractice.com
[58]Ribeiro MJ, Idbaih A, Thomas C, et al. 18F-FDG PET in neurodegenerative Langerhans cell histiocytosis: results and potential interest for an early diagnosis of the disease.J Neurol. 2008 Apr;255(4):575-80.
http://www.ncbi.nlm.nih.gov/pubmed/18227990?tool=bestpractice.com
Tissue biopsy
A definitive diagnosis is made by tissue biopsy of a lytic bone lesion, skin lesion, or lymph node. Lesional cells should demonstrate positivity for CD1a and CD207 (langerin) using immunohistochemical techniques.[1]Emile JF, Abla O, Fraitag S, et al. Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood. 2016 Jun 2;127(22):2672-81.
https://ashpublications.org/blood/article/127/22/2672/35156/Revised-classification-of-histiocytoses-and
http://www.ncbi.nlm.nih.gov/pubmed/26966089?tool=bestpractice.com
Lesional tissue should be tested for BRAF V600E mutation by immunohistochemistry or molecular assays. Negative or equivocal immunohistochemistry results should be confirmed using molecular assays. Next-generation sequencing for MAPK-ERK pathway mutations should be conducted in patients anticipated to initiate systemic therapy.[53]Goyal G, Young JR, Koster MJ, et al. The Mayo Clinic Histiocytosis Working Group consensus statement for the diagnosis and evaluation of adult patients with histiocytic neoplasms: Erdheim-Chester disease, Langerhans cell histiocytosis, and Rosai-Dorfman disease. Mayo Clin Proc. 2019 Oct;94(10):2054-71.
https://www.mayoclinicproceedings.org/article/S0025-6196(19)30273-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/31472931?tool=bestpractice.com
In instances where tissue specimen is inadequate, peripheral blood analysis using cell-free DNA next-generation sequencing is a reasonable alternative.
Patients with hematologic cytopenias/cytosis should have a bone marrow aspirate and biopsy, to exclude other myeloid neoplasms.[2]Haupt R, Minkov M, Astigarraga I, et al; Euro Histio Network. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013 Feb;60(2):175-84.
https://onlinelibrary.wiley.com/doi/10.1002/pbc.24367
http://www.ncbi.nlm.nih.gov/pubmed/23109216?tool=bestpractice.com
[53]Goyal G, Young JR, Koster MJ, et al. The Mayo Clinic Histiocytosis Working Group consensus statement for the diagnosis and evaluation of adult patients with histiocytic neoplasms: Erdheim-Chester disease, Langerhans cell histiocytosis, and Rosai-Dorfman disease. Mayo Clin Proc. 2019 Oct;94(10):2054-71.
https://www.mayoclinicproceedings.org/article/S0025-6196(19)30273-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/31472931?tool=bestpractice.com
The presence of clusters of large CD1a-positive cells in the marrow is diagnostic for LCH.