Etiology
Langerhans cells are epidermal dendritic cells that present antigen to, and activate, antigen-specific T lymphocytes. They are found in most organs. LCH is considered an inflammatory myeloid neoplasia. The condition is caused by a clonal proliferation of myeloid precursor cells, which differentiate into pathologic Langerhans cells in lesions.[13][14]
Activating mutations in the mitogen-activated protein kinase (MAPK) pathway, in particular BRAF (B-Raf proto-oncogene) V600E, have been identified in 50% to 60% cases of LCH.[15][16][17] BRAF is a cytoplasmic tyrosine kinase involved in growth factor signal transduction. Activating mutations, such as BRAF V600E, lead to increased transcription of BCL-2 like 1 (BCL2L1), which inhibits apoptosis, and decreased transcription of C-C motif chemokine receptor 7 (CCR7), which stimulates dendritic cell maturation and stimulates mobilization of activated Langerhans cells to draining lymph nodes.[3][18][19] The resultant accumulation of pathologic dendritic cells contributes to local and systemic inflammation, and may infiltrate or damage the surrounding tissue.[3][20]
Activating MAPK pathway mutations can occur at different stages of myeloid differentiation. Mutations in pluripotent hematopoietic stem cells (expressing CD34) are hypothesized to cause high-risk LCH, while mutations in dendritic cell precursors and monocytes (expressing CD11c or CD14) are thought to give rise to low-risk LCH.[13][16]
Pathophysiology
LCH is characterized by granulomatous lesions containing clonal proliferation of pathologic Langerhans cells, expressing CD1a, CD207 (langerin), and S100. LCH cells are large with a kidney-shaped nucleus.[14] [Figure caption and citation for the preceding image starts]: Very high magnification micrograph of Langerhans cell histiocytosis. H&E stain. It is characterized by Langerhans-type histiocytes that have a reniform (kidney-shaped) nucleus and stain with S100 and CD1aNephron. Reproduced under a creative commons license CC BY-SA 3.0: https://creativecommons.org/licenses/by-sa/3.0/deed.en [Citation ends].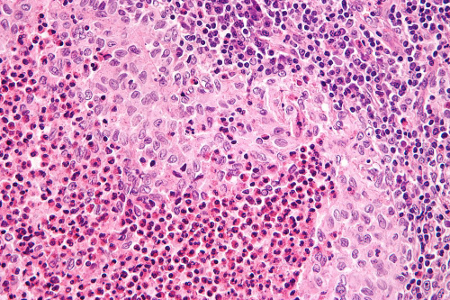
Neoplastic Langerhans cells activate and recruit other inflammatory cells, leading to development of an inflammatory infiltrate including activated T cells, eosinophils, neutrophils, and macrophages.[14] Local immune dysregulation develops, characterized by increased proinflammatory cytokine expression, tissue remodeling, and neo-angiogenesis.[21] Environmental factors, such as tobacco smoke or infection, contribute to the development and persistence of the inflammation.[20][22] Tobacco smoke causes accumulation of Langerhans cells in the lungs, and induces proinflammatory cytokine production, which leads to histiocytic granuloma formation.[20]
Classification
Histiocyte Society: histiocytosis classification[1]
L (Langerhans) group
Langerhans cell histiocytosis (LCH)
LCH single system
LCH lung positive
LCH multiple systems (MS) risk organ (RO) positive
LCH MS RO negative
Associated with another myeloproliferative/myelodysplastic disorder
Indeterminate cell histiocytosis
Erdheim Chester disease (ECD) classical type
ECD without bone involvement
ECD associated with another myeloproliferative/myelodysplastic disorder
Extracutaneous or disseminated juvenile xanthogranuloma with mitogen-activated protein kinase (MAPK)-activating or anaplastic lymphoma kinase (ALK) translocations
Mixed ECD and LCH
C (cutaneous) group
Cutaneous non-LCH histiocytoses
Xanthgranuloma family
Non-xanthogranuloma family
Cutaneous non-LCH histiocytoses with a major systemic component
Xanthoma disseminatum
Multicentric reticulocytosis
M (malignant) group
Primary malignant histiocytosis
Secondary malignant histiocytosis
R (Rosai-Dorfman disease and miscellaneous noncutaneous, non-Langerhans cell histiocytoses) group
Familial Rosai-Dorfman disease (RDD)
Classical (nodal) RDD
Extranodal RDD
Neoplasia-associated RDD
Immune disease-associated RDD
H (hemophagocytic lymphohistiocytosis and macrophage activation syndrome) group
Primary hemophagocytic lymphohistiocytosis (HLH)
Secondary HLH
Euro Histio Net: clinical classification of pediatric LCH[2]
Single-system:
One organ system involved
Usually bone, skin, lymph nodes, lungs, or the thyroid or pituitary gland.
Multisystem:
2 or more organ systems involved
Can be with or without involvement of risk organs.
Risk organs:
Specific organs are considered high-risk, because the associated mortality rates in those who do not respond to treatment are high
High-risk organs include the liver, spleen, and bone marrow.
Histiocyte Society: clinical classification of LCH in adults[4]
Unifocal LCH: solitary lesion involving any organ
Single-system pulmonary LCH: isolated lung involvement (predominantly smoking related)
Single-system multifocal LCH: >1 lesion involving any organ
Multisystem LCH: ≥2 organ/system involvement.
Use of this content is subject to our disclaimer