Approach
Characteristic history and slit lamp findings are often sufficient for diagnosis. Note that dry eye disease is frequently present with meibomian gland dysfunction and should be assessed.[1][15] See Dry eye disease.
History
Generally reveals bilateral ocular burning, itching, foreign body sensation, mild photophobia, crusting on the eyelids, and redness of lid margins. Although symptoms often overlap with those of dry eyes (e.g., contact lens intolerance), blepharitis tends to cause symptoms that are worse in the morning, whereas aqueous deficient dry eye typically causes symptoms that are worse later in the day.[1] In severe disease, corneal changes can occur, leading to reduced vision. With associated dry eye syndrome or seborrheic dermatitis, patients may report eye dryness or scaly changes of the scalp, respectively. Disease is typically chronic with intermittent exacerbations. There may be a history of dermatological conditions, such as rosacea or eczema, or of prior intraocular or lid surgery or injury.[1]
Physical examination
External exam may reveal eye crusting. Chalazion may be associated with underlying blepharitis. Facial erythema, facial telangiectasia, papules, and pustules are seen with associated acne rosacea. Flaking and greasy skin of the scalp, retroauricular area, glabella, and nasolabial folds are typical with associated seborrheic dermatitis.
Slit lamp findings
Slit lamp exam is required to confirm the diagnosis and exclude other causes.
Findings are usually bilateral, but they can be asymmetric.
Lid erythema, lid telangiectasias, collarettes around the lashes, capped meibomian glands, tear film debris, and frothy discharge are common findings.
Conjunctival hyperemia and unstable tear film with rapid tear break-up time may be present.
In severe blepharitis, corneal punctate epithelial erosions, vascularization, scarring, ulceration, phlyctenule, and perforation can be seen.[Figure caption and citation for the preceding image starts]: Anterior blepharitis: collarettes with lid erythemaFrom the collection of Dr E. Akpek [Citation ends]. [Figure caption and citation for the preceding image starts]: Corneal complication: punctate epithelial erosions that stain with fluoresceinFrom the collection of Dr E. Akpek [Citation ends].
[Figure caption and citation for the preceding image starts]: Corneal complication: punctate epithelial erosions that stain with fluoresceinFrom the collection of Dr E. Akpek [Citation ends].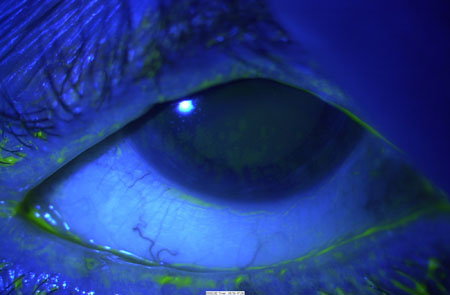 [Figure caption and citation for the preceding image starts]: Posterior blepharitis: inspissated meibomian glands and lid telangiectasiaFrom the collection of Dr E. Akpek [Citation ends].
[Figure caption and citation for the preceding image starts]: Posterior blepharitis: inspissated meibomian glands and lid telangiectasiaFrom the collection of Dr E. Akpek [Citation ends]. Eye swabs are not required.
Eye swabs are not required.
Lid biopsy
In atypical unilateral disease, lid biopsy may be warranted to exclude other disorders, including basal cell, squamous cell, or sebaceous cell carcinoma. This includes unilateral lid changes, significant lid architecture alteration, lash changes or loss, recurrent chalazion, and for refractory blepharitis.[33][34]
Lid margin culture
May be indicated in patients: 1) with recurrent anterior blepharitis and severe inflammation, or 2) not responding to initial therapy (i.e., to isolate the causative organism).[1]
Microscopic evaluation of epilated eyelashes
Demodex mites are reported to be present in 94% of ophthalmology outpatients, correlating with the presence of cylindrical dandruff (92% affected), collarettes (58%), and blepharitis (14%).[9] Epilated eyelashes can be evaluated for the presence of mites, especially in patients with cylindrical collarettes around the lashes.[35] However, given that collarettes are pathognomonic of Demodex infection, a Delphi panel agreed that epilation and direct visualization of mites was unnecessary for diagnosis if collarettes are seen on slit lamp exam.[36]
Use of this content is subject to our disclaimer