Approach
The diagnosis is initially made on clinical grounds. EDS is present from birth and is often diagnosed in childhood, but in some cases may be detected only in adulthood. Many affected people do not develop symptoms at all, or they develop only minor symptoms during their lifetime.
Musculoskeletal and skin manifestations are the primary features; cardiovascular and gastrointestinal (GI) autonomic dysfunctions, as well as other manifestations, are considered supportive findings.
Apart from joint hypermobility, no feature is universally present in any form of EDS. Due to the involvement of various organ systems, patients may initially present to a variety of different medical specialties.[15]
[Figure caption and citation for the preceding image starts]: Possible features of Ehlers-Danlos syndromesCreated by BMJ Knowledge Centre [Citation ends].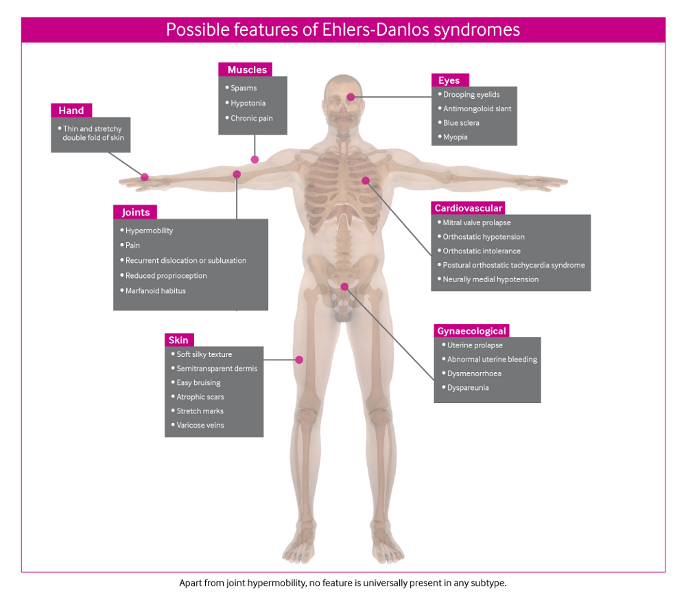
Family history of joint hypermobility is highly suggestive; the pattern of inheritance for the common subtypes is usually autosomal dominant, so that 50% of offspring of an affected person would be expected to inherit the gene and develop the phenotype.[13] However, the rare subtypes of EDS are autosomal recessive.
Musculoskeletal manifestations
Joint hypermobility
Considered a feature of all subtypes of EDS. Usually less obvious in vascular EDS (vEDS), except in the hands. Most hypermobile people are not aware of the fact and assume that everyone is as flexible as they are.
A history of delayed walking (beyond age 18 months), often with the omission of crawling and/or the substitution of bottom-shuffling, is common in hypermobile infants. They are often clumsy and fidgety. Once walking is initiated, the motor delay resolves. Hypermobile children tire easily and often want to be carried; they may have joint and/or muscle pain after exercise (growing pains).
The presence of joint hypermobility can be established directly by calculating the Beighton 9-point score, which is based on the ability to perform a series of maneuvers. A score of 5/9 or higher is usually taken to indicate generalized hypermobility.[16]
Dorsiflex the 5th metacarpophalangeal joint to 90° or greater (1 point for each side). [Figure caption and citation for the preceding image starts]: Joint hypermobility demonstrated by hyperextension of fifth metacarpophalangeal jointFrom the collection of Dr Rodney Grahame; used with permission [Citation ends].

Oppose the thumb to the volar aspect of the ipsilateral forearm (1 point for each side). [Figure caption and citation for the preceding image starts]: Joint hypermobility demonstrated by opposition of thumb to volar aspect of forearmFrom the collection of Dr Rodney Grahame; used with permission [Citation ends].

Hyperextend the elbow to 10° or greater (1 point for each side). [Figure caption and citation for the preceding image starts]: Joint hypermobility demonstrated by hyperextension of elbow to >90°From the collection of Dr Rodney Grahame; used with permission [Citation ends].

Hyperextend the knee to 10° or greater (1 point for each side). [Figure caption and citation for the preceding image starts]: Joint hypermobility demonstrated by hyperextension of kneeFrom the collection of Dr Rodney Grahame; used with permission [Citation ends].

Place the hands flat on the floor with the knees fully extended (1 point). [Figure caption and citation for the preceding image starts]: Joint hypermobility demonstrated by placing hands flat on floor with knees fully extendedFrom the collection of Dr Rodney Grahame; used with permission [Citation ends].

Hypermobility should also be sought in joints outside the 5 sites that form part of the Beighton scoring system, as each hypermobile joint identified will add evidence of joint hypermobility. Some useful maneuvers in this context include:
Passive external rotation of the shoulder to 90° or greater
Lateral flexion of cervical spine to 60° or greater
Rotation of thoracic spine to 90° or greater
Dorsiflexion of first metatarsophalangeal joint to 90° or greater
Flattening on the longitudinal arch of the feet with pronation of the foot on weight-bearing.
Joint hypermobility can also be determined indirectly by using the 5-question questionnaire. An answer in the affirmative to 2 or more questions suggests hypermobility with a sensitivity of 80% to 85% and a specificity of 80% to 90%.[17]
Can you now (or could you ever) place your hands flat on the floor without bending your knees? [Figure caption and citation for the preceding image starts]: Joint hypermobility demonstrated by placing hands flat on floor with knees fully extendedFrom the collection of Dr Rodney Grahame; used with permission [Citation ends].

Can you now (or could you ever) bend your thumb to touch your forearm? [Figure caption and citation for the preceding image starts]: Joint hypermobility demonstrated by opposition of thumb to volar aspect of forearmFrom the collection of Dr Rodney Grahame; used with permission [Citation ends].

As a child did you amuse your friends by contorting your body into strange shapes or could you do the splits?
As a child or teenager did your shoulder or kneecap dislocate on more than 1 occasion?
Do you consider yourself double-jointed?
Beighton scoreA video demonstration of Beighton score in a hypermobile Ehlers-Danlos syndrome patient.
It is important to be aware that this list of maneuvers is by no means complete, and any or all joint laxity elicited on physical exam may be relevant. Furthermore, it should be noted that various factors such as male gender, older age, muscle spasm, prior injury/surgery, and arthritic degeneration can all mask underlying joint laxity.
Joint pains
Older patients usually present with multiple-site joint or spinal pain often brought on by unaccustomed, though not necessarily excessive, physical activity and in the absence of signs of inflammation.
Unlike inflammatory joint disease (IJD) there is no visible joint swelling, warmth, or redness and no complaint of early morning stiffness unless there is an associated tendonitis. Contrary to what is seen in IJD, the joints move well and, despite pain, may retain their hypermobility.
The history should include the nature and effectiveness of pain relief, interventions to date, and any past experiences with local anesthetic use, as apparent resistance to the effects of local anesthetics is seen in about two-thirds of patients.[18]
Joint dislocation or subluxation
Because ligaments are lax, joints are unstable and dislocate or sublux easily and repeatedly, in some cases several times a day. Therefore, recurrent joint dislocation or subluxation is a common presentation.
Joint proprioception
The mutated collagen in proprioceptors leads to impaired signaling that causes deficits in joint position and sense.[19][20] This leads to incoordination of movement during normal and physically strenuous activities, which in turn may cause injury to the tissues and joints.
Muscle spasm
Tender (or nontender) muscle spasm can often be palpated in the neck and paravertebral muscles, and sometimes also in the muscles surrounding particularly unstable and/or painful joints.[21]
Chronic pain syndrome
This may develop as a consequence of trauma and is characterized by progressively severe chronic pain (whole-body pain not relieved by analgesics is common), often with fibromyalgia-like tender points on palpation, accompanied by severe fatigue, autonomic dysfunction, and psychosocial morbidity (anxiety, depression, phobias). A key element is kinesiophobia, avoiding movement as a means of avoiding pain. The result is a progressive decline in health and quality of life.
Seen in about one quarter of patients attending hypermobility clinics.[22]
Marfanoid habitus
This may be present in association with EDS (usually incomplete). It is a common finding in hypermobile and kyphoscoliotic EDS but is not necessary for diagnosis of EDS. Features include:[23]
High arched palate
Arachnodactyly
Wrist sign (Walker): positive if able to wrap the thumb and fifth finger of 1 hand around the opposite wrist such that the nailbeds of the digits overlap with each other
Thumb sign (Steinberg): positive if the adducted thumb across the palm projects beyond the ulnar border in the clenched hand.
Pectus excavatum or carinatum
Scoliosis: a sign of kyphoscoliotic EDS; it may be present in other EDS variants, albeit to a milder degree.
Arm span to height ratio >1.05
Tall stature with reduced upper segment to lower segment (US/LS) ratio of <0.85
Foot length (heel to first toe) to height ratio >0.15
Hand length (wrist crease to third finger) to height ratio >0.11.
Weakness of supporting structures
This is due to weak, lax, and less-effective connective tissues, and can manifest as:
Eye signs: drooping eyelids or antimongoloid slant, blue sclera, myopia
Muscle hypotonia: muscles may feel doughy on palpation
Mitral valve prolapse: presence of midsystolic click or late systolic murmur on cardiac auscultation
Varicose veins
Abdominal wall, inguinal, or paraumbilical hernia
Uterine or rectal prolapse.
Significant injury: because the tissues are more fragile than normal, they are at particular risk of traumatic or overuse injury. Therefore, injuries that would be inadequate to damage ligament, tendon, muscle, bone, or skin in the general population may result in significant damage.
Skin manifestations
Examination of the skin is the most reliable method of diagnosing EDS.
The skin texture usually feels soft and silky to the touch (usually the only skin finding associated with hEDS). The dermis is often semitransparent.
Easy bruising is common; the patient often notices bruising but does not recall any precipitating injury. A double fold of skin picked up on the dorsum of the hand is frequently felt to be thin. In addition, when the double fold of skin is lifted away from the dorsum of the hand, it shows more stretchiness than the skin of people who do not have EDS.[Figure caption and citation for the preceding image starts]: Increased skin stretchiness demonstrated; common finding in EDSFrom the collection of Dr Rodney Grahame; used with permission [Citation ends]. Skin involvement is key to establishing the diagnosis of classical EDS. Skin fragility with atrophic scarring and impaired wound healing are hallmark features of classical EDS and constitute the major diagnostic criteria.[24]
Skin involvement is key to establishing the diagnosis of classical EDS. Skin fragility with atrophic scarring and impaired wound healing are hallmark features of classical EDS and constitute the major diagnostic criteria.[24]
Characteristically, stretch marks (striae atrophicae) appear during maximal adolescent growth (between the ages of 11 and 13 years) on thighs, flanks, breasts, and occasionally shoulders and knees.
Scars (from previous surgery, lacerations, abrasions, chicken pox, or BCG immunization) are typically atrophic; they have less collagen, are usually thin in depth and wide in breadth, and wrinkle when squeezed between the examiner's index finger and thumb.
Patients may also present with delayed or incomplete wound healing, usually involving the laying down of scar tissue or collagen. In addition, wound dehiscence can occur due to fragility of the soft tissues.
Autonomic abnormalities
Cardiovascular
Evidence suggests association of autonomic dysfunction and hEDS.[25] Abnormalities include:
Orthostatic hypotension (OH): blood pressure decrease of >20/10 mmHg within 3 minutes of standing
Orthostatic intolerance (OI): development of symptoms within 10 minutes of upright posture that improve upon lying down; often associated with acrocyanosis (dusky color) and swollen legs (due to pooling of blood) that resolves on lying flat
Postural orthostatic tachycardia syndrome (POTS): >30-bpm increase in pulse on standing or >120 bpm within 10 minutes of head-up tilt-table testing, both in the absence of orthostatic hypotension that might trigger a normal tachycardic response.[26][27]
Neurally mediated hypotension (NMH): also referred to as vasovagal syncope or neurocardiogenic syncope; can be triggered by orthostatic stress, emotional stress, urination, coughing, swallowing, and physical exercise. A head-up tilt-table can confirm the diagnosis.
Gastrointestinal
Patients may have signs and symptoms suggesting a gastrointestinal disorder such as:
gastritis/GERD (heartburn and acid regurgitation)
gastroparesis (chronic nausea, vomiting, epigastric pain, bloating, and early satiety)
irritable bowel syndrome (recurrent abdominal pain or discomfort associated with a change in stool frequency or form; pain or discomfort may be relieved by defecation)
rectal evacuatory disorder (characterized by difficulty with defecation, with or without need for manual evacuation and laxatives).
Though gastrointestinal symptoms can occur in all EDS subtypes, perforations and bleeding complications of the gastrointestinal tract are more commonly seen in vEDS while features of functional gastrointestinal disorders are more prevalent in patients with hEDS.[28][29]
Gynecologic manifestations
Most women with hEDS experience significant gynecologic symptoms. The most common complaints include abnormal bleeding, dysmenorrhea, and dyspareunia. Some also report a diagnosis of endometriosis, but it is unclear if there is an increased prevalence of endometriosis in this population, as systematic studies are lacking.
The rate of conception is thought to be normal, but there may be a higher rate of spontaneous miscarriage. Overall, there appears to be no evidence of increased prevalence of poor obstetric outcomes compared with those of the general population, and cesarean deliveries are not indicated purely because of the diagnosis of hEDS.
There is growing evidence that hormones may play a role in modifying symptom severity, as many women experience worsening of symptoms just prior to menstruation.[30]
Investigations
Diagnosis is usually based on clinical grounds; therefore, investigations are primarily supportive. Genetic testing for the subtypes other than hEDS is available and may confirm diagnosis.[5]
Molecular testing
Should be undertaken using panel-based tests or whole exome/genome sequencing.
If sequencing tests are negative, copy number variant analysis should be pursued using multiplex ligation-dependent probe amplification (MLPA), quantitative polymerase chain reaction (qPCR), or targeted array analysis.
Molecular testing helps confirmation of diagnosis, particularly given the heterogeneity of the different EDS subtypes, and provides information on inheritance patterns, recurrence risk, and prognosis, which will help guide management for the patient.
If there are existing genetic test results, do not perform repeat testing unless there is uncertainty about the existing result, e.g., the result is inconsistent with the patient’s clinical presentation or the test methodology has changed.[31]
Imaging studies and other investigations
Plain film radiograph of the spine is usually necessary in patients presenting with spinal pain or with scoliosis noted on physical exam.
An echocardiogram helps rule out mitral valve prolapse and aortic root dilation (found in patients with both classical EDS and hEDS), and should be performed periodically, particularly in childhood and adolescence.[32]
Tests for gastrointestinal autonomic dysfunction and associated gastrointestinal conditions may be considered; they include barium enema, colonoscopy, CT colonography, and/or evacuating proctography.
Other investigations may be warranted based on presenting symptoms, such as a complete blood count and clotting screen if there is a history of easy bruising.
Tilt-table testing may be appropriate for patients with suspected cardiovascular autonomic dysfunction.
Use of this content is subject to our disclaimer
