Initial consideration should be given to the 3 most common causes of olfactory loss: prior viral infection, head injury, and chronic rhinosinusitis.[25]Patel ZM, Holbrook EH, Turner JH, et al. International consensus statement on allergy and rhinology: olfaction. Int Forum Allergy Rhinol. 2022 Apr;12(4):327-680.
https://onlinelibrary.wiley.com/doi/10.1002/alr.22929
http://www.ncbi.nlm.nih.gov/pubmed/35373533?tool=bestpractice.com
Each of these 3 causes accounts for 10% to 20% of cases.[16]Deems DA, Doty RL, Settle RG, et al. Smell and taste disorders, a study of 750 patients from the University of Pennsylvania Smell and Taste Center. Arch Otolaryngol Head Neck Surg. 1991;117:519-528.
http://www.ncbi.nlm.nih.gov/pubmed/2021470?tool=bestpractice.com
[17]Seiden AM, Duncan HJ. The diagnosis of a conductive olfactory loss. Laryngoscope. 2001 Jan;111(1):9-14.
http://www.ncbi.nlm.nih.gov/pubmed/11192906?tool=bestpractice.com
[18]Hoekman PK, Houlton JJ, Seiden AM. The utility of magnetic resonance imaging in the diagnostic evaluation of idiopathic olfactory loss. Laryngoscope. 2014 Feb;124(2):365-8.
http://www.ncbi.nlm.nih.gov/pubmed/23775878?tool=bestpractice.com
Less common causes include exposure to toxic chemicals, radiation, or medications (e.g., chemotherapeutic drugs, zinc gluconate nasal spray); prior neurosurgical or craniofacial surgery; neurodegenerative disease; autoimmune disease; and intracranial neoplasms. Rarely, patients will present with a loss of smell that appears to be congenital or related to advancing age. Unfortunately, in many cases, the precise etiology of olfactory loss remains unknown.
Postviral upper respiratory infection
Most people will experience a temporary loss of smell during an acute viral upper respiratory infection (URI). However, in relatively rare cases, the loss will persist after resolution of all other cold and flu symptoms. It appears to be a sensory loss, as biopsy studies have demonstrated degenerative changes in the olfactory neuronal receptors or neuroepithelium in the olfactory cleft.[19]Jafek BW, Hartman L, Eller PM, et al. Postviral olfactory dysfunction. Am J Rhinol. 1990 May;4(3):91-100. These patients may be anosmic or hyposmic, and many may have associated dysosmia. It seems to occur more commonly in an older age group and affects twice as many women as men. A viral-induced loss does not fluctuate, but as many as 66% of patients may experience some spontaneous recovery over a period of several years.[28]Duncan HJ, Seiden AM. Long-term follow-up of olfactory loss secondary to head trauma and upper respiratory tract infection. Arch Otolaryngol Head Neck Surg. 1995 Oct;121(10):1183-7.
http://www.ncbi.nlm.nih.gov/pubmed/7546588?tool=bestpractice.com
A retrospective study looking at a large number of patients found that the incidence of recovery was inversely related to age at onset, with 38.7% of patients overall demonstrating clinically significant improvement.[29]Cavazzana A, Larsson M, Münch M, et al. Postinfectious olfactory loss: a retrospective study on 791 patients. Laryngoscope. 2018 Jan;128(1):10-5.
http://www.ncbi.nlm.nih.gov/pubmed/28556265?tool=bestpractice.com
The prevalence of olfactory loss associated with early COVID-19 variants (between 48% and 86%) was reported to be higher than that attributable to other viral infections.[10]Saniasiaya J, Islam MA, Abdullah B. Prevalence of olfactory dysfunction in coronavirus disease 2019 (COVID-19): a meta-analysis of 27,492 patients. Laryngoscope. 2021 Apr;131(4):865-78.
https://pmc.ncbi.nlm.nih.gov/articles/PMC7753439
http://www.ncbi.nlm.nih.gov/pubmed/33219539?tool=bestpractice.com
[11]Rocke J, Hopkins C, Philpott C, et al. Is loss of sense of smell a diagnostic marker in COVID-19: a systematic review and meta-analysis. Clin Otolaryngol. 2020 Nov;45(6):914-22.
https://pmc.ncbi.nlm.nih.gov/articles/PMC7436734
http://www.ncbi.nlm.nih.gov/pubmed/32741085?tool=bestpractice.com
[12]Lechien JR, Chiesa-Estomba CM, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. 2020 Aug;277(8):2251-61.
https://pmc.ncbi.nlm.nih.gov/articles/PMC7134551
http://www.ncbi.nlm.nih.gov/pubmed/32253535?tool=bestpractice.com
[30]Liu ZY, Vaira LA, Boscolo-Rizzo P, et al. Post-viral olfactory loss and parosmia. BMJ Med. 2023 Jul 20;2(1):e000382.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10568123
http://www.ncbi.nlm.nih.gov/pubmed/37841969?tool=bestpractice.com
[31]Addison AB, Wong B, Ahmed T, et al. Clinical Olfactory Working Group consensus statement on the treatment of postinfectious olfactory dysfunction. J Allergy Clin Immunol. 2021 May;147(5):1704-19.
https://www.jacionline.org/article/S0091-6749(21)00004-X/fulltext#secsectitle0070
http://www.ncbi.nlm.nih.gov/pubmed/33453291?tool=bestpractice.com
However, later COVID-19 variants (e.g., Omicron) appear to cause less olfactory dysfunction than the earlier variants.[14]von Bartheld CS, Wang L. Prevalence of olfactory dysfunction with the omicron variant of SARS-CoV-2: a systematic review and meta-analysis. Cells. 2023 Jan 28;12(3).
https://www.mdpi.com/2073-4409/12/3/430
http://www.ncbi.nlm.nih.gov/pubmed/36766771?tool=bestpractice.com
[32]Butowt R, Bilińska K, von Bartheld C. Why does the omicron variant largely spare olfactory function? Implications for the pathogenesis of anosmia in coronavirus disease 2019. J Infect Dis. 2022 Oct 17;226(8):1304-8.
https://academic.oup.com/jid/article/226/8/1304/6573859
http://www.ncbi.nlm.nih.gov/pubmed/35467743?tool=bestpractice.com
Complete anosmia has been commonly reported in COVID-19 patients, with significant (if not complete) recovery within a matter of weeks to months.[7]Hannum ME, Ramirez VA, Lipson SJ, et al. Objective sensory testing methods reveal a higher prevalence of olfactory loss in COVID-19-positive patients compared to subjective methods: a systematic review and meta-analysis. Chem Senses. 2020 Dec 5;45(9):865-74.
https://academic.oup.com/chemse/article/45/9/865/5912953
http://www.ncbi.nlm.nih.gov/pubmed/33245136?tool=bestpractice.com
[31]Addison AB, Wong B, Ahmed T, et al. Clinical Olfactory Working Group consensus statement on the treatment of postinfectious olfactory dysfunction. J Allergy Clin Immunol. 2021 May;147(5):1704-19.
https://www.jacionline.org/article/S0091-6749(21)00004-X/fulltext#secsectitle0070
http://www.ncbi.nlm.nih.gov/pubmed/33453291?tool=bestpractice.com
Patients may report spontaneous onset of dysosmia, which may present several months after COVID-19 symptom onset.[33]Lerner DK, Garvey KL, Arrighi-Allisan AE, et al. Clinical features of parosmia associated with COVID-19 infection. Laryngoscope. 2022 Mar;132(3):633-9.
https://onlinelibrary.wiley.com/doi/10.1002/lary.29982
http://www.ncbi.nlm.nih.gov/pubmed/34870334?tool=bestpractice.com
The clinical course may be explained by COVID-19 infecting supporting (sustentacular) cells of the olfactory neuroepithelium, rather than olfactory neuronal receptors.[34]Wei G, Gu J, Gu Z, et al. Olfactory dysfunction in patients with coronavirus disease 2019: A Review. Front Neurol. 2021;12:783249.
https://www.frontiersin.org/articles/10.3389/fneur.2021.783249/full
http://www.ncbi.nlm.nih.gov/pubmed/35115994?tool=bestpractice.com
Long-term prognosis in these patients is still being assessed.[35]Tan HQM, Pendolino AL, Andrews PJ, et al. Prevalence of olfactory dysfunction and quality of life in hospitalised patients 1 year after SARS-CoV-2 infection: a cohort study. BMJ Open. 2022 Jan 25;12(1):e054598.
https://bmjopen.bmj.com/content/12/1/e054598
http://www.ncbi.nlm.nih.gov/pubmed/35078845?tool=bestpractice.com
Head injury
Overall, approximately 5%-17% of patients with a head injury will have an associated olfactory loss; incidence increases with the severity of the injury and length of posttraumatic amnesia.[36]Howell J, Costanzo RM, Reiter ER. Head trauma and olfactory function. World J Otorhinolaryngol Head Neck Surg. 2018 Mar;4(1):39-45.
https://onlinelibrary.wiley.com/doi/10.1016/j.wjorl.2018.02.001
http://www.ncbi.nlm.nih.gov/pubmed/30035260?tool=bestpractice.com
[37]Collet S, Grulois V, Bertrand B, et al. Post-traumatic olfactory dysfunction: a cohort study and update. B-ENT. 2009;5 Suppl 13:97-107.
http://www.ncbi.nlm.nih.gov/pubmed/20084810?tool=bestpractice.com
[38]Temmel AF, Quint C, Schickinger-Fischer B, et al. Characteristics of olfactory disorders in relation to major causes of olfactory loss. Arch Otolaryngol Head Neck Surg. 2002 Jun;128(6):635-41.
https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/482893
http://www.ncbi.nlm.nih.gov/pubmed/12049556?tool=bestpractice.com
Posttraumatic olfactory impairment more commonly follows a frontal or occipital blow and is related to coup-contrecoup forces that cause a shearing of the olfactory filaments as they pass through the cribriform plate. These patients tend to be anosmic, and are generally between the ages of 20 and 50 years and male (consistent with the group more at risk for head trauma). In other cases, it may be due to a concussive injury resulting from a frontal or occipital blow, and patients may experience some recovery of function, typically within the first year following the injury. The reported incidence of anosmia following traumatic brain injury varies markedly with severity of injury (4% to 60%).[39]Singh R, Humphries T, Mason S, et al. The incidence of anosmia after traumatic brain injury: the SHEFBIT cohort. Brain Inj. 2018;32(9):1122-8.
https://www.tandfonline.com/doi/full/10.1080/02699052.2018.1483028
http://www.ncbi.nlm.nih.gov/pubmed/29874472?tool=bestpractice.com
[40]Haxel BR, Grant L, Mackay-Sim A. Olfactory dysfunction after head injury. J Head Trauma Rehabil. 2008 Nov-Dec;23(6):407-13.
http://www.ncbi.nlm.nih.gov/pubmed/19033834?tool=bestpractice.com
[41]Doty RL, Yousem DM, Pham LT, et al. Olfactory dysfunction in patients with head trauma. Arch Neurol. 1997 Sep;54(9):1131-40.
http://www.ncbi.nlm.nih.gov/pubmed/9311357?tool=bestpractice.com
Chronic nasal or sinus disease
Chronic nasal and sinus pathologies that cause an olfactory loss generally do so by obstructing the nasal vault, thereby preventing access of odorants to the olfactory receptors. This causes a conductive loss rather than a sensorineural loss, although some evidence suggests there may also be inflammatory changes within the olfactory neuroepithelium.[42]Kern RC. Chronic sinusitis and anosmia: pathologic changes in the olfactory mucosa. Laryngoscope. 2000 Jul;110(7):1071-7.
http://www.ncbi.nlm.nih.gov/pubmed/10892672?tool=bestpractice.com
[43]Konstantinidis I, Witt M, Kaidoglou K, et al. Olfactory mucosa in nasal polyposis: implications for FESS outcome. Rhinology. 2010 Mar;48(1):47-53.
http://www.ncbi.nlm.nih.gov/pubmed/20502735?tool=bestpractice.com
[44]Yee KK, Pribitkin EA, Cowart BJ, et al. Neuropathology of the olfactory mucosa in chronic rhinosinusitis. Am J Rhinol Allergy. 2010 Mar-Apr;24(2):110-20.
http://www.ncbi.nlm.nih.gov/pubmed/20021743?tool=bestpractice.com
Such obstruction may be due to frank nasal polyps but may also occur from secondary edema due to localized pathology within the ethmoid sinuses without polyps. One literature review found the prevalence of olfactory dysfunction in patients with chronic rhinosinusitis approached 70%, depending on the testing method used.[45]Kohli P, Naik AN, Harruff EE, et al. The prevalence of olfactory dysfunction in chronic rhinosinusitis. Laryngoscope. 2017;127:309-20.
http://www.ncbi.nlm.nih.gov/pubmed/27873345?tool=bestpractice.com
However, patients may not complain of nasal obstruction or other nasal symptoms, but may simply present with a loss of smell.[17]Seiden AM, Duncan HJ. The diagnosis of a conductive olfactory loss. Laryngoscope. 2001 Jan;111(1):9-14.
http://www.ncbi.nlm.nih.gov/pubmed/11192906?tool=bestpractice.com
This can make the diagnosis difficult, especially when trying to distinguish from a viral etiology. The distinction is important, because chronic rhinosinusitis can be treated effectively to restore the sense of smell.[21]Kohli P, Naik AN, Farhood Z, et al. Olfactory outcomes after endoscopic sinus surgery for chronic rhinosinusitis: a meta-analysis. Otolaryngol Head Neck Surg. 2016 Dec;155(6):936-48.
http://www.ncbi.nlm.nih.gov/pubmed/27576679?tool=bestpractice.com
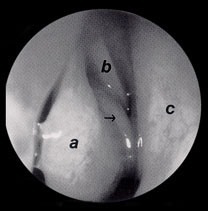
[Figure caption and citation for the preceding image starts]: Examination of the right nasal cavity using rigid nasal endoscopy. A polyp can be seen protruding from the superior meatus (arrow), while the middle meatus is clear. a = middle turbinate, b = superior turbinate, c = septumFrom the collection of Dr Allen M. Seiden [Citation ends].
Toxic exposure
Most cases occur in the workplace. But increased exposure to ambient air pollutants may be associated with olfactory dysfunction.[46]Ajmani GS, Suh HH, Pinto JM. Effects of ambient air pollution exposure on olfaction: a review. Environ Health Perspect. 2016 Nov;124(11):1683-93.
https://ehp.niehs.nih.gov/doi/10.1289/EHP136
http://www.ncbi.nlm.nih.gov/pubmed/27285588?tool=bestpractice.com
Exposure to a variety of toxic industrial and environmental agents has been associated with a loss of smell, although many of the reports in the literature are anecdotal.[47]Amoore JE. Effects of chemical exposure on olfaction in humans. In: Barrow CS, ed. Toxicology of the nasal passages. Washington. DC: Hemisphere Publishing; 1986;263-73.[48]Upadhyay UD, Holbrook EH. Olfactory loss as a result of toxic exposure. Otolaryngol Clin N Amer. 2004 Dec;37(6):1185-207.
http://www.ncbi.nlm.nih.gov/pubmed/15563910?tool=bestpractice.com
Such reports often involve sudden excessive exposure, rather than low-grade exposure over many years. Common toxic exposures include phosphorus fire, chlorine gas, metal dusts, solvents, acid fumes, oil vapors, and some household cleaners. Although its incidence is probably underestimated, toxic exposure accounts for approximately 5% of olfactory disorders.[48]Upadhyay UD, Holbrook EH. Olfactory loss as a result of toxic exposure. Otolaryngol Clin N Amer. 2004 Dec;37(6):1185-207.
http://www.ncbi.nlm.nih.gov/pubmed/15563910?tool=bestpractice.com
Several medications (e.g., amphetamines, estrogen, naphazoline, phenothiazines, prolonged use of nasal decongestants) may affect sense of smell. Olfactory loss following the use of an over-the-counter (OTC) zinc gluconate nasal spray (for the common cold) has been described.[49]Jafek BW, Linschoten MR, Murrow BW. Anosmia after intranasal zinc gluconate use. Am J Rhinol. 2004 May-Jun;18(3):137-41.
http://www.ncbi.nlm.nih.gov/pubmed/15283486?tool=bestpractice.com
The olfactory loss is thought to occur following exposure of the olfactory epithelium to the zinc cation.[50]Alexander TH, Davidson TM. Intranasal zinc and anosmia: the zinc-induced anosmia syndrome. Laryngoscope. 2006 Feb;116(2):217-20.
http://www.ncbi.nlm.nih.gov/pubmed/16467707?tool=bestpractice.com
Chemotherapeutic agents can produce loss of both smell and taste, and radiation therapy to the head and neck will cause a transient loss of both senses.[51]Doty RL, Bromley SM. Effects of drugs on olfaction and taste. Otolaryngol Clin North Am. 2004 Dec;37(6):1229-54.
http://www.ncbi.nlm.nih.gov/pubmed/15563912?tool=bestpractice.com
[52]Comeau TB, Epstein JB, Migas C. Taste and smell dysfunction in patients receiving chemotherapy: a review of current knowledge. Support Care Cancer. 2001 Nov;9(8):575-80.
http://www.ncbi.nlm.nih.gov/pubmed/11762967?tool=bestpractice.com
[53]Ophir D, Guterman A, Gross-Isseroff R. Changes in smell acuity induced by radiation exposure of the olfactory mucosa. Arch Otolaryngol Head Neck Surg. 1988 Aug;114(8):853-5.
http://www.ncbi.nlm.nih.gov/pubmed/3390326?tool=bestpractice.com
Postsurgery
Olfactory loss commonly occurs following neurosurgical procedures on the anterior cranial fossa through an anterior craniotomy approach, as well as following certain craniofacial procedures. This is expected and, therefore, these patients rarely present for further olfactory testing.
Olfactory loss may occur following endoscopic sinus surgery, due to direct injury to the olfactory cleft or scarring that obstructs the cleft. However, this is very uncommon, occurring in probably less than 2% of cases.[54]Hosemann W, Gode U, Wigand ME. Indications, technique, and results of endonasal endoscopic ethmoidectomy. Acta Otorhinolaryngol Belg. 1993;47(1):73-83.
http://www.ncbi.nlm.nih.gov/pubmed/8470554?tool=bestpractice.com
Most instances of persisting olfactory loss following sinus surgery are due to chronic inflammatory sinus disease.
Neurodegenerative diseases
Olfactory loss has been noted to be an early symptom of several neurodegenerative disorders, notably Alzheimer disease and Parkinson disease, although whether the loss reflects a true deficit or dementia is unclear.[55]Kovacs T. Mechanisms of olfactory dysfunction in aging and neurodegenerative disorders. Ageing Res Rev. 2004 Apr;3(2):215-32.
http://www.ncbi.nlm.nih.gov/pubmed/15177056?tool=bestpractice.com
Studies have found that faster olfactory decline in dementia-free older adults may predict higher incidence of subsequent cognitive impairment or dementia.[56]Dintica CS, Marseglia A, Rizzuto D, et al. Impaired olfaction is associated with cognitive decline and neurodegeneration in the brain. Neurology. 2019 Feb 12;92(7):e700-9.
https://n.neurology.org/content/92/7/e700
http://www.ncbi.nlm.nih.gov/pubmed/30651382?tool=bestpractice.com
In Alzheimer disease, neurofibrillary tangles and plaques appear to involve areas of the brain associated with olfaction, including the olfactory bulbs. Patients with Alzheimer disease and olfactory loss may often be unaware of their smell deficit and therefore not seek medical attention.[57]Devanand DP, Michaels-Marston KS, Liu X, et al. Olfactory deficits in patients with mild cognitive impairment predict Alzheimer's disease at follow-up. Am J Psychiatry. 2000 Sep;157(9):1399-405.
http://www.ncbi.nlm.nih.gov/pubmed/10964854?tool=bestpractice.com
In patients with Parkinson disease, impaired odor identification is associated with more rapid neurologic degeneration, particularly gait disturbance.[58]Wilson RS, Arnold SE, Buchman AS, et al. Odor identification and progression of parkinsonian signs in older persons. Exp Aging Res. 2008 Jul-Sep;34(3):173-87.
http://www.ncbi.nlm.nih.gov/pubmed/18568978?tool=bestpractice.com
Studies in people with Parkinson disease suggest that olfactory impairment is due at least in part to central nervous system decline.[59]Iannilli E, Stephan L, Hummel T, et al. Olfactory impairment in Parkinson's disease is a consequence of central nervous system decline. J Neurol. 2017 Jun;264(6):1236-46.
http://www.ncbi.nlm.nih.gov/pubmed/28550478?tool=bestpractice.com
Autoimmune diseases
Granulomatosis with polyangiitis (formerly known as Wegener granulomatosis) and sarcoidosis may manifest in the nose and will often cause an inflammatory obstruction of the olfactory cleft (although sarcoidosis may involve neural structures as well). Sinus disease may be the first manifestation of granulomatosis with polyangiitis, with later development of pulmonary and renal symptoms.[60]Gottschlich S, Ambrosch P, Kramkowski D, et al. Head and neck manifestations of Wegener's granulomatosis. Rhinology. 2006 Dec;44(4):227-33.
http://www.ncbi.nlm.nih.gov/pubmed/17216737?tool=bestpractice.com
Sjogren disease has been associated with olfactory loss, possibly related to very dry nasal mucosa or lymphocytic infiltration and destruction of exocrine glands.[61]Xu X, Geng L, Chen C, et al. Olfactory impairment in patients with primary Sjogren's syndrome and its correlation with organ involvement and immunological abnormalities. Arthritis Res Ther. 2021 Sep 29;23(1):250.
https://arthritis-research.biomedcentral.com/articles/10.1186/s13075-021-02624-6
http://www.ncbi.nlm.nih.gov/pubmed/34587995?tool=bestpractice.com
Most of these patients will probably have other symptoms in addition to olfactory dysfunction.
Sinonasal malignancies
Sinonasal tumors, both benign and malignant, can cause an obstructive olfactory loss, but these patients more often present due to other nasal symptoms, such as nasal obstruction or epistaxis.[16]Deems DA, Doty RL, Settle RG, et al. Smell and taste disorders, a study of 750 patients from the University of Pennsylvania Smell and Taste Center. Arch Otolaryngol Head Neck Surg. 1991;117:519-528.
http://www.ncbi.nlm.nih.gov/pubmed/2021470?tool=bestpractice.com
[17]Seiden AM, Duncan HJ. The diagnosis of a conductive olfactory loss. Laryngoscope. 2001 Jan;111(1):9-14.
http://www.ncbi.nlm.nih.gov/pubmed/11192906?tool=bestpractice.com
[62]Goodspeed RB, Gent JF, Catalanotto FA. Chemosensory dysfunction. Clinical evaluation results from a taste and smell clinic. Postgrad Med. 1987 Jan;81(1):251-7.
http://www.ncbi.nlm.nih.gov/pubmed/3809040?tool=bestpractice.com
Esthesioneuroblastoma, an uncommon malignant neoplasm believed to arise from the olfactory neuroepithelium, can cause anosmia. These patients typically present with other nasal symptoms.
A tumor of the anterior cranial fossa, such as an olfactory groove meningioma, can cause olfactory loss. However, patients generally present with headache, cognitive deficits, or vision loss, or develop other focal neurologic signs that cause them to seek medical attention.
Genetic syndromes
Congenital anosmia accounts for approximately 3% of cases.[17]Seiden AM, Duncan HJ. The diagnosis of a conductive olfactory loss. Laryngoscope. 2001 Jan;111(1):9-14.
http://www.ncbi.nlm.nih.gov/pubmed/11192906?tool=bestpractice.com
Although several well-described congenital syndromes, such as Turner syndrome and Kallmann syndrome, have been associated with olfactory loss, in most patients the loss of smell is an isolated finding. Patients will describe having no recollection of ever being able to smell.[63]John H, Schmid C. Kallmann's syndrome: clues to clinical diagnosis. Int J Impot Res. 2000 Apr;12(2):121-3.
http://www.ncbi.nlm.nih.gov/pubmed/11052640?tool=bestpractice.com
An MRI scan may demonstrate hypoplasia or aplasia of the olfactory bulb or tract; or, rarely, a frontal lobe encephalocele; or it may be normal.[64]Hamilton BE, Weissman JL. Imaging of chemosensory loss. Otolaryngol Clin N Amer. 2004 Dec;37(6):1255-80.
http://www.ncbi.nlm.nih.gov/pubmed/15563913?tool=bestpractice.com
Aging
Olfactory loss may occur with advancing age, but usually does not become significant until after the seventh decade. Even then, it tends to occur gradually along with diminution of the other senses, so that patients typically accept this limitation and rarely present for evaluation. It is important, however, not to attribute an olfactory loss to age when an older patient presents for evaluation.
Chemosensory test results must be compared with age-matched controls.[65]Doty RL, Shaman P, Dann M. Development of the University of Pennsylvania Smell Identification Test: a standardized microencapsulated test of olfactory function. Physiol Behav. 1984 Mar;32(3):489-502.
http://www.ncbi.nlm.nih.gov/pubmed/6463130?tool=bestpractice.com