Tests
1st tests to order
erythrocyte sedimentation rate (ESR)
Test
The ESR is only a rough estimate of systemic inflammation, however, and there are many reasons for false-positive elevations.
Result
elevated
C-reactive protein (CRP)
Test
CRP is a nonspecific marker of inflammation.
Result
elevated
antineutrophil cytoplasmic autoantibodies (ANCA)
Test
The presence of ANCA is strongly correlated with certain forms of vasculitis (i.e., granulomatosis with polyangiitis, microscopic polyangiitis, and eosinophilic granulomatosis with polyangiitis), but it would be impossible to establish a diagnosis of vasculitis based on the blood test alone.
In general, a cytoplasmic ANCA (c-ANCA) is associated with antibodies against proteinase-3 (PR3-ANCA), and is characteristic of granulomatosis with polyangiitis. A perinuclear ANCA (p-ANCA) is associated with antibodies against myeloperoxidase (MPO-ANCA), and is characteristic of microscopic polyangiitis or eosinophilic granulomatosis with polyangiitis.
Result
positive
assessment for glomerulonephritis
Test
Glomerulonephritis associated with small-vessel vasculitis may lead to renal dysfunction.
Assessment for glomerulonephritis involves tests such as urinalysis, microscopy of urine sediment, and estimated glomerular filtration rate (eGFR). See Glomerulonephritis for the full diagnostic work-up.
Result
may indicate presence of glomerulonephritis
biopsy of affected tissue
Test
Biopsy is the best test for establishing the diagnosis but is not always feasible due to site of affected tissue and may be misleading due to sampling error or immunosuppressive therapy.
Choose as noninvasive a site as possible, but with the greatest likelihood of a positive result.
Include subcutaneous fat during biopsy of a skin lesion to increase the probability of sampling a medium-sized blood vessel.
The unifying feature of systemic vasculitis is the presence of immune-mediated blood vessel wall injury. Fibrinoid necrosis of the vessel wall with karyorrhexis (fragmentation of the nucleus and the breakup of the chromatin into unstructured granules) and red blood cell extravasation are pathognomonic for this disorder.[7] Note that a perivascular inflammatory cell infiltrate is not diagnostic of vasculitis and may be seen in other inflammatory conditions.
Direct immunofluorescence should be performed whenever possible, as the pattern of immunoglobulin deposition may provide additional clues to the underlying etiology. IgM and C3 deposition are consistent with a mixed-essential cryoglobulinemia. IgA deposition is seen in IgA vasculitis. The presence of a pauci-immune vasculitis with minimal immunoreactants on immunofluorescence is consistent with an ANCA-associated vasculitis such as granulomatosis with polyangiitis.[Figure caption and citation for the preceding image starts]: Biopsy specimen showing florid transmural inflammation of a small arteryFrom the collection of Loic Guillevin, MD, Hopital Cochin, Paris, France [Citation ends]. [Figure caption and citation for the preceding image starts]: Photomicrograph of the aorta from a patient with Takayasu arteritis demonstrating marked thickening of the intimal layer and inflammatory infiltrates in the media and laminar necrosisFrom the collection of Dylan Miller, MD, Mayo Clinic [Citation ends].
[Figure caption and citation for the preceding image starts]: Photomicrograph of the aorta from a patient with Takayasu arteritis demonstrating marked thickening of the intimal layer and inflammatory infiltrates in the media and laminar necrosisFrom the collection of Dylan Miller, MD, Mayo Clinic [Citation ends].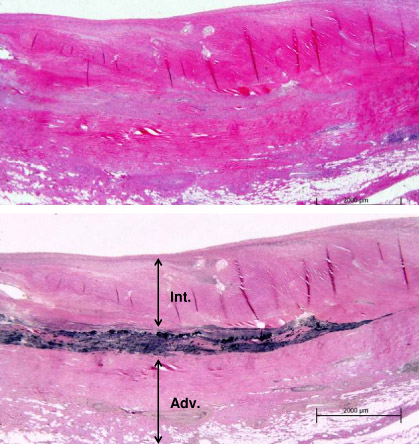
Result
vessel wall necrosis, fibrinoid necrosis, karyorrhexis (fragmentation of the nucleus and the break up of the chromatin into unstructured granules), and red blood cell extravasation
Tests to consider
conventional angiography or magnetic resonance angiography (MRA)
Test
Angiography can be extremely helpful to diagnose medium- and large-vessel vasculitis.
Beading, aneurysm, and smooth, tapering vessel stenosis are consistent with medium- or large-vessel vasculitis.
Angiography can be conventional (CT) or MRA.
Conventional angiography is the best test for diagnosing large-vessel vasculitis but is invasive and the optimal choice of method depends on local facilities and expertise as well as the anatomic site in question.
Angiography generally does not have a role in the evaluation of a small-vessel vasculitis.
Result
beading, aneurysm, or smooth, tapering vessel stenosis
positron emission tomography (PET) scan
Test
The utility of PET scanning has not been well established, although it may be useful to help establish the diagnosis of the large vessel vasculitides, such as giant cell arteritis or Takayasu arteritis.[8]
Result
may demonstrate changes associated with vasculitis
Use of this content is subject to our disclaimer