Urgent considerations
See Differentials for more details
Patients suspected of having any one of the following immediately sight-threatening conditions should be referred urgently for a same-day assessment by an ophthalmologist.[1]
Angle-closure glaucoma
This is a vision-threatening condition. Symptoms suggestive of angle-closure glaucoma include:
Pain in the affected eye
Blurred vision
Halos around lights seen from one eye
Headache
Associated nausea or vomiting.
The cornea can appear hazy if corneal oedema is present, and the pupil may be fixed and mid-dilated. If angle-closure glaucoma is suspected, then immediate referral for an ophthalmological opinion and treatment should be sought.[9] Delay in the diagnosis and referral of angle-closure glaucoma has been shown to be detrimental to the final outcome.[10]
Immediate treatment consists of carbonic anhydrase inhibitors, such as acetazolamide or methazolamide, to decrease aqueous humour formation. [Figure caption and citation for the preceding image starts]: Angle-closure glaucoma: central corneal oedema with an oval-shaped mid-dilated pupil.Private collection - courtesy of Mr Hugh Harris [Citation ends].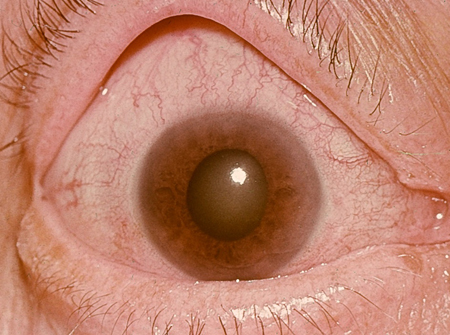
Neonatal conjunctivitis
Neonatal conjunctivitis (ophthalmia neonatorum) is usually a mild illness if appropriately treated. However, untreated infection (e.g., with gonococcus, chlamydia, pseudomonas, or herpes) can lead to sight-threatening complications and potentially serious systemic infection.[11][12][13] Complications of neonatal conjunctivitis due to chlamydia include superficial corneal vascularisation, conjunctival scarring, and pneumonia. Complications due to gonorrhoeal infections include corneal scarring, ulceration, panophthalmitis, perforation of the globe, and permanent visual impairment.[11][12] Patients with suspected neonatal conjunctivitis should be referred immediately to an ophthalmologist.[13][Figure caption and citation for the preceding image starts]: A newborn with gonococcal ophthalmia neonatorum caused by a maternally transmitted gonococcal infectionUS Centers for Disease Control and Prevention/ J. Pledger [Citation ends]. Infants less than 1 month old should be evaluated by a paediatrician and may require systemic antibiotics, in addition to topical antibiotic treatment.
Infants less than 1 month old should be evaluated by a paediatrician and may require systemic antibiotics, in addition to topical antibiotic treatment.
Trauma: chemical injury
Chemical injuries, especially from alkali-based solutions, are potentially extremely serious and can lead to long-term ocular surface problems. Immediate irrigation with water or 0.9% saline solution to remove the reservoir of chemicals from the eye should be attempted before any other procedures.[14] The amount of irrigation required is dependent on the pH of the tear film. After the pH has normalised, referral for further ophthalmological management is advised.[15]
Corneal ulcer
Bacterial, viral, or fungal corneal ulcers are vision-threatening conditions that need to be referred to an ophthalmologist urgently to ensure appropriate treatment to limit corneal scarring. Corneal ulcer can lead to perforation of the eye.[Figure caption and citation for the preceding image starts]: Corneal ulcer seen with fluorescein stainPrivate collection - courtesy of Mr Hugh Harris [Citation ends]. [Figure caption and citation for the preceding image starts]: Dendritic ulcer seen with fluorescein stainPrivate collection - courtesy of Mr Hugh Harris [Citation ends].
[Figure caption and citation for the preceding image starts]: Dendritic ulcer seen with fluorescein stainPrivate collection - courtesy of Mr Hugh Harris [Citation ends]. [Figure caption and citation for the preceding image starts]: Penetrating corneal injury with iris prolapsePrivate collection - courtesy of Mr Hugh Harris [Citation ends].
[Figure caption and citation for the preceding image starts]: Penetrating corneal injury with iris prolapsePrivate collection - courtesy of Mr Hugh Harris [Citation ends].
Contact lens-related red eye
This is potentially a vision-threatening condition and needs to be referred to an ophthalmologist to ensure appropriate treatment to limit corneal scarring.[16] The patient should be advised to cease use of their contact lenses and take the contact lenses to the local eye hospital where they are seen.
Corneal foreign body
High-velocity foreign bodies may penetrate the globe. Any history of a high-velocity injury (e.g., resulting from the use of a hammer) should be referred for appropriate and immediate imaging.
Penetrating and non-penetrating corneal foreign bodies are potentially vision-threatening conditions that require referral to an ophthalmologist to ensure appropriate treatment.
[Figure caption and citation for the preceding image starts]: Corneal foreign bodyPrivate collection - courtesy of Mr Hugh Harris [Citation ends].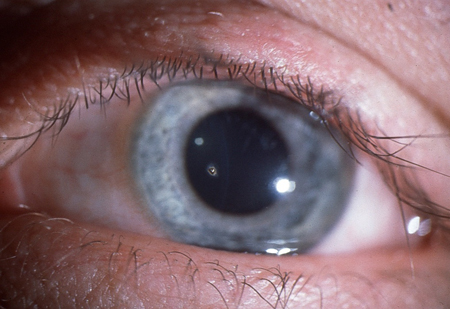
Penetrating ocular trauma
Very gentle initial examination is required to prevent possible expulsion of intra-ocular contents. Prompt specialist treatment is required to reduce the risk of sight- and eye-threatening complications.
Scleritis
Scleritis is potentially a vision-threatening condition. Certain forms of scleritis can lead to perforation of the globe and reduced visual acuity.[17] If global perforation is suspected, the eye should be shielded and palpation should be avoided. It should be evaluated further by an ophthalmologist. Scleritis is commonly associated with connective tissue disorders including rheumatoid arthritis, granulomatosis with polyangiitis (formerly known as Wegener’s granulomatosis), systemic lupus erythematosus, and relapsing polychondritis.[Figure caption and citation for the preceding image starts]: ScleritisPrivate collection - courtesy of Mr Hugh Harris [Citation ends]. [Figure caption and citation for the preceding image starts]: Penetrating corneal injury with iris prolapsePrivate collection - courtesy of Mr Hugh Harris [Citation ends].
[Figure caption and citation for the preceding image starts]: Penetrating corneal injury with iris prolapsePrivate collection - courtesy of Mr Hugh Harris [Citation ends].
Use of this content is subject to our disclaimer