Although plantar fasciitis is considered a self-limiting condition, it may take up to 18 months for pain resolution, thereby presenting a challenge for clinicians. Approximately 80% of patients improve within 12 months with nonoperative therapy.[35]Trojian T, Tucker AK. Plantar fasciitis. Am Fam Physician. 2019 Jun 15;99(12):744-50.
https://www.aafp.org/pubs/afp/issues/2019/0615/p744.html
http://www.ncbi.nlm.nih.gov/pubmed/31194492?tool=bestpractice.com
The American College of Foot and Ankle Surgeons recommends categorizing patients by duration of symptoms in order to allow selection of treatments that will have the greatest effect within each stage of plantar fasciitis. They define the 3 phases of plantar fasciitis as follows:[3]Schneider HP, Baca JM, Carpenter BB, et al. American College of Foot and Ankle Surgeons clinical consensus statement: diagnosis and treatment of adult acquired infracalcaneal heel pain. J Foot Ankle Surg. 2018 Mar-Apr;57(2):370-81.
https://www.jfas.org/article/S1067-2516(17)30619-1/abstract
http://www.ncbi.nlm.nih.gov/pubmed/29284574?tool=bestpractice.com
Acute: symptoms present for up to 6 weeks
Subacute: symptoms present for 6 to 12 weeks
Chronic: symptoms present for >3 months
A subdivision of chronic is refractory/recalcitrant. Refractory plantar fasciitis is best defined as chronic plantar fasciitis that has not improved with appropriate intervention for >6 months and is much more difficult to successfully treat.
Treatment goals
The goal of treatment is complete pain relief. This often requires many months of therapy, with reports ranging from 4 months to 18 months of conservative treatment to achieve this goal.[36]Donley BG, Moore T, Sferra J, et al. The efficacy of oral nonsteroidal anti-inflammatory medication (NSAID) in the treatment of plantar fasciitis: a randomized, prospective, placebo-controlled study. Foot Ankle Int. 2007;28:20-23.
http://www.ncbi.nlm.nih.gov/pubmed/17257533?tool=bestpractice.com
Treatment targets the anatomical, biomechanical, and environmental factors that may lead to the initiation of the cause of foot pain and disability.[3]Schneider HP, Baca JM, Carpenter BB, et al. American College of Foot and Ankle Surgeons clinical consensus statement: diagnosis and treatment of adult acquired infracalcaneal heel pain. J Foot Ankle Surg. 2018 Mar-Apr;57(2):370-81.
https://www.jfas.org/article/S1067-2516(17)30619-1/abstract
http://www.ncbi.nlm.nih.gov/pubmed/29284574?tool=bestpractice.com
[9]Koc TA Jr, Bise CG, Neville C, et al. Heel pain - plantar fasciitis: revision 2023. J Orthop Sports Phys Ther. 2023 Dec;53(12):CPG1-39.
https://www.jospt.org/doi/10.2519/jospt.2023.0303
http://www.ncbi.nlm.nih.gov/pubmed/38037331?tool=bestpractice.com
[37]Roos E, Angstrom M, Soderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int. 2006;27:606-611.
http://www.ncbi.nlm.nih.gov/pubmed/16919213?tool=bestpractice.com
Combination therapy is the general rule, aimed at addressing pain and inflammation, reducing tissue stress, and restoring muscle strength and flexibility.[9]Koc TA Jr, Bise CG, Neville C, et al. Heel pain - plantar fasciitis: revision 2023. J Orthop Sports Phys Ther. 2023 Dec;53(12):CPG1-39.
https://www.jospt.org/doi/10.2519/jospt.2023.0303
http://www.ncbi.nlm.nih.gov/pubmed/38037331?tool=bestpractice.com
[38]Crosby W, Humble RN. Rehabilitation of plantar fasciitis. Clin Podiatr Med Surg. 2001;18:225-231.
http://www.ncbi.nlm.nih.gov/pubmed/11417152?tool=bestpractice.com
Controlled randomized studies typically compare combination therapies rather than relying on a single treatment to provide complete long-term resolution. Studies also vary in their means of measurement of a successful outcome, frequently relying more on patients' subjective reports than on one objective measurement tool. Nonetheless, the outcome for individuals with acute plantar fasciitis has been studied and is usually favorable.
Initial treatment
First-line therapy is nonoperative and includes various combinations of rest, weight reduction methods, foot orthotics, mechanical support, and stretching of the tendoachilles and plantar fascia. Most patients will be able to implement these strategies themselves. Corticosteroid injections or nonsteroidal anti-inflammatory drugs (NSAIDs) for short-term pain relief and cast immobilization are sometimes used. For the majority of patients, conservative therapies prove to be beneficial in relieving heel pain.
Only persistent, significantly painful heels that interfere with weight-bearing activity and that fail to respond to nonsurgical therapy after about 6 to 12 months are considered for extracorporeal shockwave therapy (ESWT) or surgical intervention.
Rest, self-care advice, and management of precipitating factors
Rest or modification of exercise activity (e.g., avoidance of running, dancing, jumping, prolonged standing/walking, or walking barefoot on hard, concrete floors) is typically recommended. One study cited rest as the therapy that worked best for 25% of patients treated for plantar fasciitis.[39]Wolgin M, Cook C, Graham C, et al. Conservative treatment of plantar heel pain: long-term follow-up. Foot Ankle Int. 1994;15:97-102.
http://www.ncbi.nlm.nih.gov/pubmed/7951946?tool=bestpractice.com
Patients should be advised to wear shoes with good arch support and cushioned heels (such as laced sports shoes). Patients in all stages of plantar fasciitis are advised to avoid nonsupportive shoes such as flip-flops and ballet slippers.[3]Schneider HP, Baca JM, Carpenter BB, et al. American College of Foot and Ankle Surgeons clinical consensus statement: diagnosis and treatment of adult acquired infracalcaneal heel pain. J Foot Ankle Surg. 2018 Mar-Apr;57(2):370-81.
https://www.jfas.org/article/S1067-2516(17)30619-1/abstract
http://www.ncbi.nlm.nih.gov/pubmed/29284574?tool=bestpractice.com
Weight reduction is recommended in people with overweight or obesity. Education and counseling on exercise strategies to gain or maintain optimal lean body mass should be provided. Referral to a dietitian may be considered.[9]Koc TA Jr, Bise CG, Neville C, et al. Heel pain - plantar fasciitis: revision 2023. J Orthop Sports Phys Ther. 2023 Dec;53(12):CPG1-39.
https://www.jospt.org/doi/10.2519/jospt.2023.0303
http://www.ncbi.nlm.nih.gov/pubmed/38037331?tool=bestpractice.com
Elevated BMI is not only a risk factor for plantar fasciitis but also a predictor of the extent of functional loss as reported by patients.[16]Riddle DL, Schappert SM. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int. 2004;25:303-310.
http://www.ncbi.nlm.nih.gov/pubmed/15134610?tool=bestpractice.com
[17]van Leeuwen KD, Rogers J, Winzenberg T, et al. Higher body mass index is associated with plantar fasciopathy/'plantar fasciitis': systematic review and meta-analysis of various clinical and imaging risk factors. Br J Sports Med. 2016;50:972-981.
http://www.ncbi.nlm.nih.gov/pubmed/26644427?tool=bestpractice.com
However, no studies have evaluated the effect of weight loss on occurrence of symptoms.[18]Irving DB, Cook JL, Young MA, et al. Obesity and pronated foot type may increase the risk of chronic plantar heel pain: a matched case-control study. BMC Musculoskelet Disord. 2007;8:41.
http://www.biomedcentral.com/1471-2474/8/41
http://www.ncbi.nlm.nih.gov/pubmed/17506905?tool=bestpractice.com
Stretching
Tight hamstrings and equinus are common in patients with plantar fasciitis and treatment of equinus is important for all stages of the condition.[3]Schneider HP, Baca JM, Carpenter BB, et al. American College of Foot and Ankle Surgeons clinical consensus statement: diagnosis and treatment of adult acquired infracalcaneal heel pain. J Foot Ankle Surg. 2018 Mar-Apr;57(2):370-81.
https://www.jfas.org/article/S1067-2516(17)30619-1/abstract
http://www.ncbi.nlm.nih.gov/pubmed/29284574?tool=bestpractice.com
Stretching, aimed at the tendoachilles and the plantar fascia, is recommended 3 times daily with 10 repetitions of each stretch.[40]DiGiovanni BF, Nawoczenski DA, Lintal ME, et al. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain: a prospective, randomized study. J Bone Joint Surg Am. 2003;85:1270-7.
http://www.ncbi.nlm.nih.gov/pubmed/12851352?tool=bestpractice.com
Patients may be referred to a physical therapist or podiatrist for help with technique, although formal physical therapy has not been shown to be more effective than home stretching exercises.[41]Kaiser PB, Keyser C, Crawford AM, et al. A prospective randomized controlled trial comparing physical therapy with independent home stretching for plantar fasciitis. J Am Acad Orthop Surg. 2022 Jul 15;30(14):682-9.
https://journals.lww.com/jaaos/abstract/2022/07150/a_prospective_randomized_controlled_trial.7.aspx
http://www.ncbi.nlm.nih.gov/pubmed/35797682?tool=bestpractice.com
A study found nonweight-bearing stretching exercises, specific to the plantar fascia, to be superior to the standard weight-bearing achilles tendon-stretching exercises in patients with recalcitrant pain.[42]DiGiovanni BF, Nawoczenski DA, Malay DP, et al. Plantar fascia-specific stretching exercises improves outcomes in patients with chronic plantar fasciitis: a prospective clinical trial with two-year follow up. J Bone Joint Surg Am. 2006;88:1775-81.
http://www.ncbi.nlm.nih.gov/pubmed/16882901?tool=bestpractice.com
Recommendations for stretching are based on the hypothesis that nocturnal contracture of the gastrocnemius-soleus complex contributes to the irritation of the plantar fascia and persistence of symptoms.[43]Barrett S, O'Malley R. Plantar fasciitis and other causes of heel pain. Am Fam Physician. 1999;59:2200-2206.
http://www.ncbi.nlm.nih.gov/pubmed/10221305?tool=bestpractice.com
[44]Powell MW, Post WR, Keener JK. Effective treatment of chronic plantar fasciitis with dorsiflexion night splints: a crossover prospective randomized study. Foot Ankle Int. 1998;19:10-18.
http://www.ncbi.nlm.nih.gov/pubmed/9462907?tool=bestpractice.com
The main pain-relieving benefits of stretching appear to occur within the first 2 weeks to 4 months. Orthoses may be used to increase the benefits of stretching.[9]Koc TA Jr, Bise CG, Neville C, et al. Heel pain - plantar fasciitis: revision 2023. J Orthop Sports Phys Ther. 2023 Dec;53(12):CPG1-39.
https://www.jospt.org/doi/10.2519/jospt.2023.0303
http://www.ncbi.nlm.nih.gov/pubmed/38037331?tool=bestpractice.com
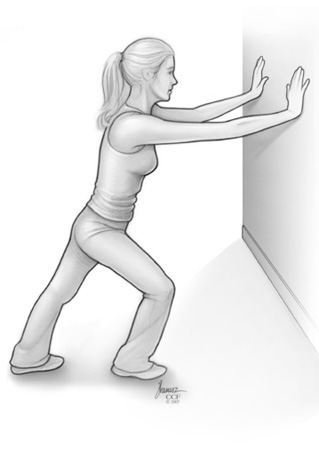
[Figure caption and citation for the preceding image starts]: Calf stretchFrom the collection of Alex Koleszar, Cleveland Clinic; used with permission [Citation ends].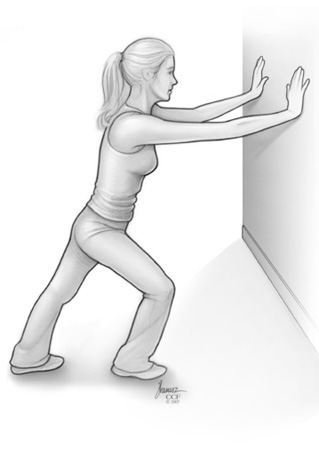 [Figure caption and citation for the preceding image starts]: Achilles stretchFrom the collection of Alex Koleszar, Cleveland Clinic; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Achilles stretchFrom the collection of Alex Koleszar, Cleveland Clinic; used with permission [Citation ends].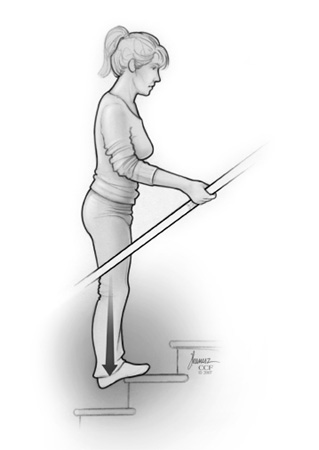 [Figure caption and citation for the preceding image starts]: Plantar stretchFrom the collection of Alex Koleszar, Cleveland Clinic; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Plantar stretchFrom the collection of Alex Koleszar, Cleveland Clinic; used with permission [Citation ends].
Low-Dye taping or strapping
Low-Dye (antipronation) taping is frequently used as a first-line short-term treatment for plantar fasciitis. It alters the mechanical function of the foot, supporting the medial longitudinal arch and decreasing stress on the plantar fascia, which leads to relief of morning pain and stiffness. The first strip of tape, used as an anchor, is applied plantarly and transversely, with no tension, just proximal to the metatarsal head. A second longitudinal strip is applied around the sides of the foot, just proximal to the first and fifth metatarsal heads. Then lateral to medial straps are placed plantarly on the heel and arch.[45]Dye RW. A strapping. J Natl Assoc. Chiropodists. 1939;29:11. It is typically applied for a period of 3 to 5 days.[46]Hyland MR, Webber-Gaffney A, Cohen L, et al. Randomized controlled trial of calcaneal taping, sham taping, and plantar fascia stretching for the short-term management of plantar heel pain. J Orthop Sports Phys Ther. 2006;36:364-371.
http://www.ncbi.nlm.nih.gov/pubmed/16776486?tool=bestpractice.com
[47]Radford JA, Landorf KB, Buchbinder R, et al. Effectiveness of low-Dye taping for the short-term treatment of plantar heel pain: a randomized trial. BMC Musculoskelet Disord. 2006;7:64.
http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=16895612
http://www.ncbi.nlm.nih.gov/pubmed/16895612?tool=bestpractice.com
Low-Dye taping is effective in the short-term (up to 6 weeks) and used as a precursor to arch supports.[9]Koc TA Jr, Bise CG, Neville C, et al. Heel pain - plantar fasciitis: revision 2023. J Orthop Sports Phys Ther. 2023 Dec;53(12):CPG1-39.
https://www.jospt.org/doi/10.2519/jospt.2023.0303
http://www.ncbi.nlm.nih.gov/pubmed/38037331?tool=bestpractice.com
One systematic review found that the addition of taping on stretching exercises has a surplus value.[48]van de Water AT, Speksnijder CM. Efficacy of taping for the treatment of plantar fasciosis: a systematic review of controlled trials. J Am Podiatr Med Assoc. 2010;100:41-51.
http://www.ncbi.nlm.nih.gov/pubmed/20093544?tool=bestpractice.com
Strapping with elastic therapeutic tape is an alternative treatment; it is applied to the gastrocnemius and plantar fascia for short-term (1-6 weeks) pain reduction.[9]Koc TA Jr, Bise CG, Neville C, et al. Heel pain - plantar fasciitis: revision 2023. J Orthop Sports Phys Ther. 2023 Dec;53(12):CPG1-39.
https://www.jospt.org/doi/10.2519/jospt.2023.0303
http://www.ncbi.nlm.nih.gov/pubmed/38037331?tool=bestpractice.com
Foot orthotics
Insoles, prefabricated devices, custom-made orthotics, and heel cushions are all frequently used for treating plantar fasciitis. Meta-analyses suggest they have little to no effect as a stand-alone treatment to improve pain and function in the short-term (<3 months).[9]Koc TA Jr, Bise CG, Neville C, et al. Heel pain - plantar fasciitis: revision 2023. J Orthop Sports Phys Ther. 2023 Dec;53(12):CPG1-39.
https://www.jospt.org/doi/10.2519/jospt.2023.0303
http://www.ncbi.nlm.nih.gov/pubmed/38037331?tool=bestpractice.com
[49]Guimarães JS, Arcanjo FL, Leporace G, et al. Effects of therapeutic interventions on pain due to plantar fasciitis: a systematic review and meta-analysis. Clin Rehabil. 2023 Jun;37(6):727-46.
https://journals.sagepub.com/doi/10.1177/02692155221143865
http://www.ncbi.nlm.nih.gov/pubmed/36571559?tool=bestpractice.com
However, orthoses may be beneficial when combined with other treatments, especially in patients who respond positively to antipronation taping techniques.[9]Koc TA Jr, Bise CG, Neville C, et al. Heel pain - plantar fasciitis: revision 2023. J Orthop Sports Phys Ther. 2023 Dec;53(12):CPG1-39.
https://www.jospt.org/doi/10.2519/jospt.2023.0303
http://www.ncbi.nlm.nih.gov/pubmed/38037331?tool=bestpractice.com
There is evidence that at 12 months, no significant difference exists among patient outcomes with prefabricated versus custom orthoses.[49]Guimarães JS, Arcanjo FL, Leporace G, et al. Effects of therapeutic interventions on pain due to plantar fasciitis: a systematic review and meta-analysis. Clin Rehabil. 2023 Jun;37(6):727-46.
https://journals.sagepub.com/doi/10.1177/02692155221143865
http://www.ncbi.nlm.nih.gov/pubmed/36571559?tool=bestpractice.com
[50]Hawke FB, Burns J, Radford JA, et al. Custom-made foot orthoses for the treatment of foot pain. Cochrane Database Syst Rev. 2008;(3):CD006801.
http://www.ncbi.nlm.nih.gov/pubmed/18646168?tool=bestpractice.com
Some institutions include orthotic dispensing within a physical therapy or podiatry department.
Night splints
Night splints, used for a 1- to 3-month period, have been shown to be effective adjuncts to treatment for those with both acute and recalcitrant pain, particularly those who consistently have pain with the first step in the morning.[9]Koc TA Jr, Bise CG, Neville C, et al. Heel pain - plantar fasciitis: revision 2023. J Orthop Sports Phys Ther. 2023 Dec;53(12):CPG1-39.
https://www.jospt.org/doi/10.2519/jospt.2023.0303
http://www.ncbi.nlm.nih.gov/pubmed/38037331?tool=bestpractice.com
[44]Powell MW, Post WR, Keener JK. Effective treatment of chronic plantar fasciitis with dorsiflexion night splints: a crossover prospective randomized study. Foot Ankle Int. 1998;19:10-18.
http://www.ncbi.nlm.nih.gov/pubmed/9462907?tool=bestpractice.com
[51]Wapner KL, Sharkey PF. The use of night splints for treatment of recalcitrant plantar fasciitis. Foot Ankle. 1991;12:135-137.
http://www.ncbi.nlm.nih.gov/pubmed/1791004?tool=bestpractice.com
[52]Probe PA, Baca M, Adams R, et al. Night splint treatment for plantar fasciitis: a prospective randomized study. Clin Orthop Rel Res. 1999;368:190-195.
http://www.ncbi.nlm.nih.gov/pubmed/10613168?tool=bestpractice.com
Efficacy may be limited, however, as many patients remove them to sleep due to interference with sleep comfort.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Oral NSAIDs are commonly prescribed for pain and inflammation in the short term. Large randomized controlled trials are lacking. One small randomized trial found a trend toward improved pain relief and reduced disability, but no significant difference, with NSAID therapy compared with placebo and conservative treatment with night splints, visco-elastic heel cups, and stretching.[36]Donley BG, Moore T, Sferra J, et al. The efficacy of oral nonsteroidal anti-inflammatory medication (NSAID) in the treatment of plantar fasciitis: a randomized, prospective, placebo-controlled study. Foot Ankle Int. 2007;28:20-23.
http://www.ncbi.nlm.nih.gov/pubmed/17257533?tool=bestpractice.com
NSAIDs are typically used in conjunction with other therapies and are considered most effective when treating the initial stage of plantar fasciitis. The American College of Foot and Ankle Surgeons does not recommend the routine use of NSAIDs in treating plantar fasciitis due to lack of supporting data.[3]Schneider HP, Baca JM, Carpenter BB, et al. American College of Foot and Ankle Surgeons clinical consensus statement: diagnosis and treatment of adult acquired infracalcaneal heel pain. J Foot Ankle Surg. 2018 Mar-Apr;57(2):370-81.
https://www.jfas.org/article/S1067-2516(17)30619-1/abstract
http://www.ncbi.nlm.nih.gov/pubmed/29284574?tool=bestpractice.com
Corticosteroid injections
Corticosteroid injections are used in the short term for acute pain management of plantar fasciitis. They are considered if conservative treatment leads to inadequate relief of pain, or if pain is especially high on initial presentation. They have been shown to be efficacious in relieving pain; however, most studies report only short-term (up to 6 weeks), and not sustained, benefits.[53]Tsai WC, Hsu CC, Chen CP, et al. Plantar fasciitis treated with local steroid injection: comparison between sonographic and palpation guidance. J Clin Ultrasound. 2006;34:12-16.
http://www.ncbi.nlm.nih.gov/pubmed/16353228?tool=bestpractice.com
[54]Porter MD, Shadbolt B. Intralesional corticosteroid injection versus extracorporeal shock wave therapy for plantar fasciopathy. Clin J Sports Med. 2005;15:119-124.
http://www.ncbi.nlm.nih.gov/pubmed/15867552?tool=bestpractice.com
[55]David JA, Sankarapandian V, Christopher PR, et al. Injected corticosteroids for treating plantar heel pain in adults. Cochrane Database Syst Rev. 2017 Jun 11;6:CD009348.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6481652
http://www.ncbi.nlm.nih.gov/pubmed/28602048?tool=bestpractice.com
[  ]
For adults with plantar heel pain, how do locally injected corticosteroids compare with extracorporeal shock wave therapy (ESWT)?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.2997/fullShow me the answer One study, however, found that the significant reduction in thickness of plantar fascia seen at 1 month following corticosteroid injection persisted on re-scanning at 6 months.[56]Genc H, Saracoglu M, Nacir B, et al. Long-term ultrasonographic follow-up of plantar fasciitis patients treated with steroid injection. Joint Bone Spine. 2005;72:61-65.
http://www.ncbi.nlm.nih.gov/pubmed/15681250?tool=bestpractice.com
A Cochrane review pooled data from 8 trials and found only a modest short-term (<1 month) benefit of glucocorticoid injections compared with placebo.[55]David JA, Sankarapandian V, Christopher PR, et al. Injected corticosteroids for treating plantar heel pain in adults. Cochrane Database Syst Rev. 2017 Jun 11;6:CD009348.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6481652
http://www.ncbi.nlm.nih.gov/pubmed/28602048?tool=bestpractice.com
Another systematic review found that corticosteroid injection was more effective than some comparators (autologous blood injection, foot orthoses, and physical therapy) for the reduction of pain and the improvement of function in people with plantar heel pain in the short term. However, it was no more effective than placebo injection for reducing pain in the short and medium term.[57]Whittaker GA, Munteanu SE, Menz HB, et al. Corticosteroid injection for plantar heel pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019 Aug 17;20(1):378.
https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-019-2749-z
http://www.ncbi.nlm.nih.gov/pubmed/31421688?tool=bestpractice.com
]
For adults with plantar heel pain, how do locally injected corticosteroids compare with extracorporeal shock wave therapy (ESWT)?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.2997/fullShow me the answer One study, however, found that the significant reduction in thickness of plantar fascia seen at 1 month following corticosteroid injection persisted on re-scanning at 6 months.[56]Genc H, Saracoglu M, Nacir B, et al. Long-term ultrasonographic follow-up of plantar fasciitis patients treated with steroid injection. Joint Bone Spine. 2005;72:61-65.
http://www.ncbi.nlm.nih.gov/pubmed/15681250?tool=bestpractice.com
A Cochrane review pooled data from 8 trials and found only a modest short-term (<1 month) benefit of glucocorticoid injections compared with placebo.[55]David JA, Sankarapandian V, Christopher PR, et al. Injected corticosteroids for treating plantar heel pain in adults. Cochrane Database Syst Rev. 2017 Jun 11;6:CD009348.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6481652
http://www.ncbi.nlm.nih.gov/pubmed/28602048?tool=bestpractice.com
Another systematic review found that corticosteroid injection was more effective than some comparators (autologous blood injection, foot orthoses, and physical therapy) for the reduction of pain and the improvement of function in people with plantar heel pain in the short term. However, it was no more effective than placebo injection for reducing pain in the short and medium term.[57]Whittaker GA, Munteanu SE, Menz HB, et al. Corticosteroid injection for plantar heel pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019 Aug 17;20(1):378.
https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-019-2749-z
http://www.ncbi.nlm.nih.gov/pubmed/31421688?tool=bestpractice.com
Injections are administered using a plantar medial approach, typically in combination with local anesthetic to work as an immediate analgesic and anti-inflammatory agent. Lidocaine and bupivacaine are used in combination to achieve a faster onset and longer relief. Ultrasound guidance has been found to be associated with superior results and a lower risk of recurrence of heel pain compared to palpation-guided injection.[3]Schneider HP, Baca JM, Carpenter BB, et al. American College of Foot and Ankle Surgeons clinical consensus statement: diagnosis and treatment of adult acquired infracalcaneal heel pain. J Foot Ankle Surg. 2018 Mar-Apr;57(2):370-81.
https://www.jfas.org/article/S1067-2516(17)30619-1/abstract
http://www.ncbi.nlm.nih.gov/pubmed/29284574?tool=bestpractice.com
[8]Rhim HC, Kwon J, Park J, et al. A systematic review of systematic reviews on the epidemiology, evaluation, and treatment of plantar fasciitis. Life (Basel). 2021 Nov 24;11(12).
https://www.mdpi.com/2075-1729/11/12/1287
http://www.ncbi.nlm.nih.gov/pubmed/34947818?tool=bestpractice.com
Complications are uncommon, but include infection, subcutaneous fat atrophy, skin pigmentation changes, fascial rupture, peripheral nerve injury, and muscle damage.[58]Sellman JR. Plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int. 1994;15:376-381.
http://www.ncbi.nlm.nih.gov/pubmed/7951973?tool=bestpractice.com
[59]Ahstrom JP Jr. Spontaneous rupture of the plantar fascia. Am J Sports Med. 1988;16:306-307.
http://www.ncbi.nlm.nih.gov/pubmed/2898217?tool=bestpractice.com
Injection therapy can be very painful and this is the most commonly reported adverse event.[60]Mann RA, Baxter DE, Lutter LD. Running symposium. Foot Ankle. 1981;1:190-224.
http://www.ncbi.nlm.nih.gov/pubmed/7262751?tool=bestpractice.com
Post-injection pain can last for several days. If the initial treatment was beneficial but symptoms return, the treatment may be repeated once with a minimum of 6 weeks between injections.
Other physical therapies
Icing: this may be the most underreported adjunct to management. Used for 20 minutes at a time, this is a local pain reducer with virtually no adverse systemic effects.
Phonophoresis: a technique by which therapeutic ultrasound is used to introduce ketoprofen gel through intact skin into the subcutaneous tissues. Limited evidence suggests that it can reduce pain short-term in patients with plantar fasciitis.[9]Koc TA Jr, Bise CG, Neville C, et al. Heel pain - plantar fasciitis: revision 2023. J Orthop Sports Phys Ther. 2023 Dec;53(12):CPG1-39.
https://www.jospt.org/doi/10.2519/jospt.2023.0303
http://www.ncbi.nlm.nih.gov/pubmed/38037331?tool=bestpractice.com
Deep tissue massage with myofascial release[3]Schneider HP, Baca JM, Carpenter BB, et al. American College of Foot and Ankle Surgeons clinical consensus statement: diagnosis and treatment of adult acquired infracalcaneal heel pain. J Foot Ankle Surg. 2018 Mar-Apr;57(2):370-81.
https://www.jfas.org/article/S1067-2516(17)30619-1/abstract
http://www.ncbi.nlm.nih.gov/pubmed/29284574?tool=bestpractice.com
Soft tissue mobilization: mobilization of gastrocnemius and soleus myofascia, specifically targeting trigger points and areas of soft tissue restriction, may help to reduce pain and improve function.[3]Schneider HP, Baca JM, Carpenter BB, et al. American College of Foot and Ankle Surgeons clinical consensus statement: diagnosis and treatment of adult acquired infracalcaneal heel pain. J Foot Ankle Surg. 2018 Mar-Apr;57(2):370-81.
https://www.jfas.org/article/S1067-2516(17)30619-1/abstract
http://www.ncbi.nlm.nih.gov/pubmed/29284574?tool=bestpractice.com
[9]Koc TA Jr, Bise CG, Neville C, et al. Heel pain - plantar fasciitis: revision 2023. J Orthop Sports Phys Ther. 2023 Dec;53(12):CPG1-39.
https://www.jospt.org/doi/10.2519/jospt.2023.0303
http://www.ncbi.nlm.nih.gov/pubmed/38037331?tool=bestpractice.com
[61]Piper S, Shearer HM, Côté P, et al. The effectiveness of soft-tissue therapy for the management of musculoskeletal disorders and injuries of the upper and lower extremities: systematic review by the Ontario Protocol for Traffic Injury management (OPTIMa) collaboration. Man Ther. 2016;21:18-34.
http://www.mskscienceandpractice.com/article/S1356-689X(15)00174-5/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/26386912?tool=bestpractice.com
Manual therapy: joint mobilization to improve any identified restrictions in joint mobility of the lower extremity, with an emphasis on improving talocrural dorsiflexion, may provide symptomatic relief and improve function.[9]Koc TA Jr, Bise CG, Neville C, et al. Heel pain - plantar fasciitis: revision 2023. J Orthop Sports Phys Ther. 2023 Dec;53(12):CPG1-39.
https://www.jospt.org/doi/10.2519/jospt.2023.0303
http://www.ncbi.nlm.nih.gov/pubmed/38037331?tool=bestpractice.com
Therapeutic exercise: resistance training for the musculature of the foot and ankle. The combination of manual therapy, patient education, stretching, resistance training, and neurodynamic interventions can improve pain and function.[9]Koc TA Jr, Bise CG, Neville C, et al. Heel pain - plantar fasciitis: revision 2023. J Orthop Sports Phys Ther. 2023 Dec;53(12):CPG1-39.
https://www.jospt.org/doi/10.2519/jospt.2023.0303
http://www.ncbi.nlm.nih.gov/pubmed/38037331?tool=bestpractice.com
Low-level laser therapy: multiple systematic reviews suggest that laser therapy can be used to reduce pain and activity limitations short-term.[62]Wang W, Jiang W, Tang C, et al. Clinical efficacy of low-level laser therapy in plantar fasciitis: A systematic review and meta-analysis. Medicine (Baltimore). 2019 Jan;98(3):e14088.
https://www.doi.org/10.1097/MD.0000000000014088
http://www.ncbi.nlm.nih.gov/pubmed/30653125?tool=bestpractice.com
[63]Guimarães JS, Arcanjo FL, Leporace G, et al. Effect of low-level laser therapy on pain and disability in patients with plantar fasciitis: A systematic review and meta-analysis. Musculoskelet Sci Pract. 2022 Feb;57:102478.
https://www.sciencedirect.com/science/article/abs/pii/S2468781221001624?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/34847470?tool=bestpractice.com
[64]Naterstad IF, Joensen J, Bjordal JM, et al. Efficacy of low-level laser therapy in patients with lower extremity tendinopathy or plantar fasciitis: systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2022 Sep 28;12(9):e059479.
https://www.doi.org/10.1136/bmjopen-2021-059479
http://www.ncbi.nlm.nih.gov/pubmed/36171024?tool=bestpractice.com
Dry needling: use of a thin filiform needle to stimulate underlying myofascial trigger points in the gastrocnemius, soles, and plantar muscles of the foot to improve pain and function.[9]Koc TA Jr, Bise CG, Neville C, et al. Heel pain - plantar fasciitis: revision 2023. J Orthop Sports Phys Ther. 2023 Dec;53(12):CPG1-39.
https://www.jospt.org/doi/10.2519/jospt.2023.0303
http://www.ncbi.nlm.nih.gov/pubmed/38037331?tool=bestpractice.com
One meta-analysis found low-quality evidence that dry needling is effective for short-term pain relief.[49]Guimarães JS, Arcanjo FL, Leporace G, et al. Effects of therapeutic interventions on pain due to plantar fasciitis: a systematic review and meta-analysis. Clin Rehabil. 2023 Jun;37(6):727-46.
https://journals.sagepub.com/doi/10.1177/02692155221143865
http://www.ncbi.nlm.nih.gov/pubmed/36571559?tool=bestpractice.com
Iontophoresis: the application of an electrical current to promote transdermal delivery of dexamethasone 0.4% or acetic acid 5%. Due to limited evidence, iontophoresis is considered a second-line physical therapy option, with manual therapy, stretching, and foot orthoses preferred.[9]Koc TA Jr, Bise CG, Neville C, et al. Heel pain - plantar fasciitis: revision 2023. J Orthop Sports Phys Ther. 2023 Dec;53(12):CPG1-39.
https://www.jospt.org/doi/10.2519/jospt.2023.0303
http://www.ncbi.nlm.nih.gov/pubmed/38037331?tool=bestpractice.com
Cast immobilization
Cast immobilization can be used to eradicate morning pain and stiffness, allow rest with weight-bearing, and provide short-term and long-term pain relief in people with extreme pain presentation or with unresponsive heel pain. The painful foot is placed in an anatomically correct position for the duration of healing. Immobilization can be difficult to tolerate, particularly for those with degenerative arthritis or obesity, and activities of daily living may be adversely affected.
Second- and third-line therapy
Only people with persistent, significant pain that interferes with weight-bearing activity and that fails to respond to nonsurgical therapy after about 6 to 12 months are considered for extracorporeal shock wave therapy (ESWT) or surgical intervention.
Extracorporeal shock wave therapy (ESWT)
The outcome for the 10% of patients who fail to respond to conservative care after 12 months is not well understood. ESWT has evolved as a noninvasive approach for recalcitrant plantar fasciitis pain and is a recommended second-line treatment.[3]Schneider HP, Baca JM, Carpenter BB, et al. American College of Foot and Ankle Surgeons clinical consensus statement: diagnosis and treatment of adult acquired infracalcaneal heel pain. J Foot Ankle Surg. 2018 Mar-Apr;57(2):370-81.
https://www.jfas.org/article/S1067-2516(17)30619-1/abstract
http://www.ncbi.nlm.nih.gov/pubmed/29284574?tool=bestpractice.com
[65]Rompe JD, Furia J, Weil L, et al. Shock wave therapy for chronic plantar fasciopathy. Br Med Bull. 2007;81-82:183-208.
http://bmb.oxfordjournals.org/cgi/content/full/81-82/1/183?view=long&pmid=17456546
http://www.ncbi.nlm.nih.gov/pubmed/17456546?tool=bestpractice.com
It is proposed that ESWT creates local tissue injury that causes selective dysfunction of unmyelinated sensory nerves, neovascularisation, and increased amounts of tissue growth factors within the locally injured structures.[65]Rompe JD, Furia J, Weil L, et al. Shock wave therapy for chronic plantar fasciopathy. Br Med Bull. 2007;81-82:183-208.
http://bmb.oxfordjournals.org/cgi/content/full/81-82/1/183?view=long&pmid=17456546
http://www.ncbi.nlm.nih.gov/pubmed/17456546?tool=bestpractice.com
Two techniques have been described: a high-energy single-treatment approach with local anesthetic pre-procedure, and a series of three low-energy treatments. A therapeutic response in the plantar fascia is expected by 12 weeks. One study found that low-intensity treatment was more effective for pain relief and improved function versus high-intensity treatment.[66]Yin MC, Ye J, Yao M, et al. Is extracorporeal shock wave therapy clinical efficacy for relief of chronic, recalcitrant plantar fasciitis? A systematic review and meta-analysis of randomized placebo or active-treatment controlled trials. Arch Phys Med Rehabil. 2014;95:1585-1593.
http://www.ncbi.nlm.nih.gov/pubmed/24662810?tool=bestpractice.com
No serious adverse events have been described. Multiple systematic reviews have examined the benefit of ESWT, and overall it appears to provide better longer-term outcomes over corticosteroid injections and most other interventions studied.[8]Rhim HC, Kwon J, Park J, et al. A systematic review of systematic reviews on the epidemiology, evaluation, and treatment of plantar fasciitis. Life (Basel). 2021 Nov 24;11(12).
https://www.mdpi.com/2075-1729/11/12/1287
http://www.ncbi.nlm.nih.gov/pubmed/34947818?tool=bestpractice.com
A general observation across studies is that approximately 70% of patients with chronic or subacute plantar fasciitis who undergo ESWT experience meaningful improvement in their heel pain at 12 weeks.[3]Schneider HP, Baca JM, Carpenter BB, et al. American College of Foot and Ankle Surgeons clinical consensus statement: diagnosis and treatment of adult acquired infracalcaneal heel pain. J Foot Ankle Surg. 2018 Mar-Apr;57(2):370-81.
https://www.jfas.org/article/S1067-2516(17)30619-1/abstract
http://www.ncbi.nlm.nih.gov/pubmed/29284574?tool=bestpractice.com
Surgery
In patients with recalcitrant pain, surgery has been shown to be generally effective and is considered as a third-line option.[1]Williams SK, Brage M. Heel pain - plantar fasciitis and Achilles enthesopathy. Clin Sports Med. 2004;23:123-144.
http://www.ncbi.nlm.nih.gov/pubmed/15062587?tool=bestpractice.com
Various surgical techniques exist (e.g., partial or complete plantar fascia release with or without calcaneal spur resection, excision of abnormal tissue, and nerve decompression). Favorable outcomes have been reported in more than 75% of patients, but recovery time is often slow. Persistent pain may occur in up to one quarter of patients up to two or more years post surgery. Complications include swelling, fracture, nerve damage, and arch flattening.[4]Buchbinder R. Plantar fasciitis. N Engl J Med. 2004;350:2159-66.
http://www.ncbi.nlm.nih.gov/pubmed/15152061?tool=bestpractice.com
[67]Ogden JA, Cross GL, Williams SS. Bilateral chronic proximal plantar fasciopathy: treatment with electrohydraulic orthotripsy. Foot Ankle Int. 2004;25:298-302.
http://www.ncbi.nlm.nih.gov/pubmed/15134609?tool=bestpractice.com
[68]Sammarco GJ, Helfrey RB. Surgical treatment of recalcitrant plantar fasciitis. Foot Ankle Int. 1996;17:520-526.
http://www.ncbi.nlm.nih.gov/pubmed/8886777?tool=bestpractice.com
A frequently used surgical approach, partial plantar fascia release with nerve release, has resulted in mixed outcomes, with some reports demonstrating about a 50% success rate. The recommendation is to release <50% of the plantar fascia rather than 100% in order to prevent lateral column instability.[69]Brugh AM, Fallat AM, Savoy-Moore RT. Lateral column symptomatology following plantar fascia release: a prospective study. J Foot Ankle Surg. 2002;41:365-371.
http://www.ncbi.nlm.nih.gov/pubmed/12500787?tool=bestpractice.com
Nerve decompression may be helpful for people with neuritic pain associated with recalcitrant heel pain. An endoscopically released plantar fascia approach is another technique, with potential for quicker return to normal function. However, it is associated with specific risks, including nerve damage and insufficient or overzealous release of the plantar fascia without open visualization of the anatomy.
Weight has not been a factor in the success of surgical outcomes. Overweight individuals may experience the same success as others if surgical intervention is elected. Patients who have had symptoms for more than 2 years, who then go on to surgical intervention, have less favorable results after surgery.
 [Figure caption and citation for the preceding image starts]: Achilles stretchFrom the collection of Alex Koleszar, Cleveland Clinic; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Achilles stretchFrom the collection of Alex Koleszar, Cleveland Clinic; used with permission [Citation ends].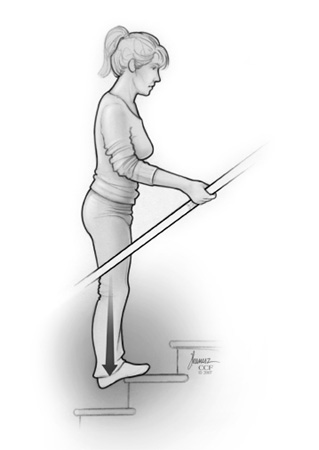 [Figure caption and citation for the preceding image starts]: Plantar stretchFrom the collection of Alex Koleszar, Cleveland Clinic; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Plantar stretchFrom the collection of Alex Koleszar, Cleveland Clinic; used with permission [Citation ends].
 ]
One study, however, found that the significant reduction in thickness of plantar fascia seen at 1 month following corticosteroid injection persisted on re-scanning at 6 months.[56] A Cochrane review pooled data from 8 trials and found only a modest short-term (<1 month) benefit of glucocorticoid injections compared with placebo.[55] Another systematic review found that corticosteroid injection was more effective than some comparators (autologous blood injection, foot orthoses, and physical therapy) for the reduction of pain and the improvement of function in people with plantar heel pain in the short term. However, it was no more effective than placebo injection for reducing pain in the short and medium term.[57]
]
One study, however, found that the significant reduction in thickness of plantar fascia seen at 1 month following corticosteroid injection persisted on re-scanning at 6 months.[56] A Cochrane review pooled data from 8 trials and found only a modest short-term (<1 month) benefit of glucocorticoid injections compared with placebo.[55] Another systematic review found that corticosteroid injection was more effective than some comparators (autologous blood injection, foot orthoses, and physical therapy) for the reduction of pain and the improvement of function in people with plantar heel pain in the short term. However, it was no more effective than placebo injection for reducing pain in the short and medium term.[57]