Approach
History, together with a physical and neurologic exam, are typically suggestive of an intracranial mass lesion. In the setting of trauma, intracranial hematomas are typically high on the list of differential diagnoses.[34] Noncontrast computed tomography (CT) scans are imperative when assessing a patient with a moderate or high risk for intracranial injury.[35]
Acute subdural hematoma (SDH) classically manifests with acute neurologic decline including alteration in consciousness, contralateral weakness, and signs of brainstem herniation. Chronic SDH manifests with symptoms that range from acute neurologic deficit to slow cognitive decline. Because of brain atrophy over time, older patients with chronic SDH are often less symptomatic than younger patients, who are more susceptible to the mass effect from an intracranial hematoma.[36]
[Figure caption and citation for the preceding image starts]: CT scan of the brain of an 80-year-old man with a gait disorder and a progressive cognitive impairment dating back about 6 months, showing a bilateral chronic subdural hematoma up to the convexityAdapted from BMJ Case Rep. 2009;2009:bcr06.2008.0130 [Citation ends]. [Figure caption and citation for the preceding image starts]: CT scans of the brain of an 80-year-old man with a gait disorder and a progressive cognitive impairment dating back about 6 months, showing a bilateral chronic subdural hematoma up to the convexityAdapted from BMJ Case Rep. 2009;2009:bcr06.2008.0130 [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scans of the brain of an 80-year-old man with a gait disorder and a progressive cognitive impairment dating back about 6 months, showing a bilateral chronic subdural hematoma up to the convexityAdapted from BMJ Case Rep. 2009;2009:bcr06.2008.0130 [Citation ends].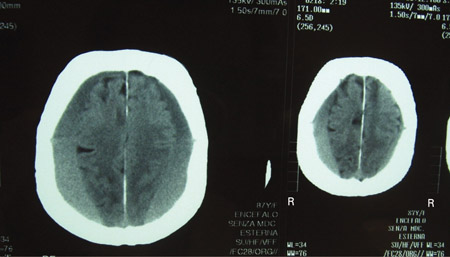
History
Key features in the history include recent history of trauma, loss of consciousness or period of decreased alertness, potential seizure activity, loss of bowel and bladder continence, headache, weakness or sensory changes, or changes in cognition, speech, or vision.[3] Enquiry about recent use of antiplatelets, antithrombotics, or anticoagulants is imperative.[12] A history of liver or renal disease is important when evaluating coagulation and platelet function.
Physical exam
Physical signs of trauma should be sought on the head and neck. Scalp and face abrasions, lacerations, avulsions, or ecchymosis are important to note. Periorbital or retroauricular ecchymosis, as well as otorrhea or rhinorrhea, may indicate occult basilar skull fracture. It is also important to always evaluate the cervical spine for tenderness, deformity, ecchymosis, or step-off in all patients with suspected head injury. Cervical spine immobilization should always be maintained as a protective measure, until potential injury is excluded.
Neurologic exam
Calculation of the admission Glasgow Coma Scale (GCS) score, in the absence of sedation and paralysis, is important for prognosis and management.[37] In addition, pupil size, symmetry, and reactivity should be noted. If the patient is able to follow commands, the presence of a pronator drift (indicating early hemiparesis) should be noted. If the patient cannot follow commands, the response to stimulation in all four extremities is noted.
The total GCS score is the sum of points from eye opening, verbal response, and motor response scores (from 3 to 15 points total):
Eye opening: spontaneous (4 points), to verbal command (3 points), to painful stimulation (2 points), none (1 point)
Motor response: obeys verbal commands (6 points), localizes to painful stimulus (5 points), flexion withdrawal to painful stimulus (4 points), decorticate response to painful stimulus (3 points), decerebrate (extensor) response to painful stimulus (2 points), none (1 point)
Verbal response: oriented conversation (5 points), disorientated conversation (4 points), inappropriate words (3 points), incomprehensible sounds (2 points), none (1 point).
CT of the brain
This is critical in the evaluation of head trauma.[35] Bone windowing can help to identify fractures and intracranial air. Brain windowing aids in the identification of hematomas and brain swelling. Subdural fluid collections are usually crescentic in shape and can cross suture lines.[38] Acute hematomas are hyperdense, subacute hematomas are usually hyperdense or isodense, and chronic hematomas are usually hypodense.[39] However, SDHs that are isodense relative to the brain parenchyma can be hyperacute; for example, in a profoundly anemic patient or in a patient with an arachnoid tear and a mixture of hemorrhage and cerebrospinal fluid (CSF).[38] The presence of midline shift, the patency of the basal cisterns, and the effacement of sulcal-gyral patterns underlying the hematoma are noted. Other intracranial hematomas, such as epidural hematomas or cerebral contusions, may be identified. Cerebral swelling may be manifested as the loss of gray-white matter distinction or gyral integrity. SDHs that have a hypodense "swirl" inside them signify potential hyperacute hematoma with active bleeding.[40][41]
Assessment criteria to guide imaging include the American College of Radiology Appropriateness Criteria® and the Canadian CT Head Rule.[42][35]
American College of Radiology Appropriateness Criteria®[35]
Patients identified as having moderate or high risk for intracranial injury should undergo early postinjury noncontrast CT for evidence of intracerebral hematoma, midline shift, or increased intracranial pressure.
The Canadian CT Head Rule is a clinical decision rule derived and validated in adults with minor head injuries. It states that a CT of the head is required in patients with minor head injuries only if they have any of the following: [ Canadian CT Head Rule Opens in new window ] [42]
Glasgow coma score <15 at 2 hours after injury
Suspected open or depressed skull fracture
Any sign of a basal skull fracture
Two or more episodes of vomiting after the injury
Age 65 years or over
Amnesia of the period before the injury of 30 minutes or longer
Dangerous mechanism of injury (pedestrian hit by a vehicle, ejection from a vehicle, fall from ≥3 feet or down ≥5 stairs).
MRI of the brain
While CT is considered the first-line imaging modality for suspected intracranial injury, magnetic resonance imaging (MRI) is useful when there are persistent neurologic deficits that remain unexplained after CT, especially in the subacute or chronic phase or in the absence of trauma history.[35] MRI may identify differential diagnoses (e.g., lymphoma, metastasis, sarcoma, infection). Many other pathologies involving the leptomeninges or subdural space can mimic the appearance of SDHs on CT. One review found the most common pathologies mimicking SDH to be lymphoma (29%), metastasis (21%), sarcoma (15%), infection (8%), and autoimmune disorders (8%).[43] In nearly 80% of these cases, there was no history of trauma and most presented with a history of progressive headache. With this in mind, additional imaging such as MRI may be considered in patients presenting with an atraumatic history, progressive headache, and possible SDH on CT. In addition, MRI may identify incidental hematomas in patients being evaluated for neurologic complaints. Typically, acute hematomas are isointense on T1-weighted images and hypointense on T2-weighted images. Subacute hematomas are usually hyperintense on T1-weighted images and either hypointense or hyperintense on T2-weighted images (dependent on age of hematoma). Chronic SDHs are hypointense on both T1- and T2-weighted images.
When SDH is identified by CT in children with intentional brain injury, subsequent MRI will disclose additional abnormalities in approximately 25% of those imaged.[44] MRI may be indicated as a follow-up study when there are persistent neurologic deficits that remain unexplained after a head CT.[35]
Plain skull x-ray
X-ray is neither sensitive nor specific for intracranial hematomas.[35] May be useful for identifying skull fractures or the presence of intracranial shrapnel.
Special diagnostic situations
Bilateral SDHs are common, comprising up to 24% of observed chronic SDHs.[3][45] They can present with mixed patterns: bilateral acute or chronic SDHs or a combination, with acute on one side and chronic on the other. When equal in size, the increase in pressure associated with each subdural is equal, so there is minimal or no midline shift.[3] Diagnostically this can be challenging, especially when both hematomas are subacute in age and isodense on CT.[3] As the brain parenchyma is compressed bilaterally, the direction of the mass effect trends away from lateral shifts (i.e., subfalcine herniation) and toward downward shifts and central herniation, a potentially fatal complication if not diagnosed and corrected in a timely fashion.[3]
An epidural hematoma may be present on the contralateral side to SDH. Although rare, this is a potentially life-threatening situation, and a small epidural hematoma contralateral to an acute SDH can rapidly expand when the compressive force of the SDH is relieved by surgical evacuation.[46][47] Initial recognition is therefore important. Most epidural hematomas are associated with skull fractures coursing through the foramen spinosum, where the middle meningeal artery is injured.[38]
Use of this content is subject to our disclaimer