History and exam
Key diagnostic factors
common
family history of NF1
Parent and/or offspring affected. All first-degree relatives should be examined for signs of NF1.
pain, any location
Usually due to peripheral nerve neurofibromas.
neurologic deficits: gross motor delay, general incoordination, school performance problems
Occur in about 60% of NF1 patients.[17] Such patients may have particular problems with expressive and receptive prosody, including speech.
compromised vision
Optic gliomas are found in 15% of the NF1 population; one third of these lesions are symptomatic.[18]
compromised social interactions
Very large numbers of cutaneous neurofibromas and very large diffuse plexiform neurofibromas may cause serious cosmetic compromise, especially those located in and around the head and neck.
Apart from cosmetic and esthetic considerations, some patients may have impoverished or otherwise compromised social interactions.[19][20]
skin: café au lait spots, axillary freckling, cutaneous juvenile xanthogranulomas, neurofibromas
Cutaneous juvenile xanthogranulomas are transient in childhood, and three types of neurofibromas occur: cutaneous, subcutaneous, and diffuse plexiform.
Early-onset subcutaneous neurofibromas are harbingers of paraspinal nodular plexiform neurofibromas, serious morbidity, and early death.
Early and enlarging cutaneous neurofibromas demonstrate buttonholing (i.e., pushing deeper into the dermis when pressed) and may be pruritic.[Figure caption and citation for the preceding image starts]: Café au lait spots on the back of a young boyFrom the personal collection of Dr Vincent M. Riccardi; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Cutaneous neurofibromas in a patient with NF1From the personal collection of Dr D. Gareth Evans; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Cutaneous neurofibromas in a patient with NF1From the personal collection of Dr D. Gareth Evans; used with permission [Citation ends].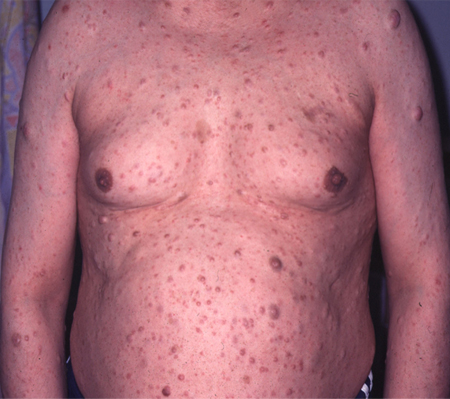 [Figure caption and citation for the preceding image starts]: Left anterior chest diffuse plexiform neurofibroma with overlying hyperpigmentationFrom the personal collection of Dr Vincent M. Riccardi; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Left anterior chest diffuse plexiform neurofibroma with overlying hyperpigmentationFrom the personal collection of Dr Vincent M. Riccardi; used with permission [Citation ends].
head and neck: unilateral diffuse plexiform neurofibroma divisions of the trigeminal nerve
A unilateral diffuse plexiform neurofibroma involving any or all of the three divisions of the trigeminal nerve occurs in 3% to 5% of patients with NF1.[17][21]
Early on, it is often misdiagnosed (e.g., as mumps).
It stops at the midline and is not prone to malignant peripheral nerve sheath tumor (MPNST) transformation as are other diffuse plexiform neurofibromas.
Subcutaneous and nodular plexiform neurofibromas may be readily visible and palpable in both the anterior and posterior triangles of the neck (as well as in the supraclavicular fossae).
ophthalmologic: visual compromise, optic disk pallor, iris Lisch nodules
Performing a physical exam to identify visual compromise and optic disk pallor is important for making decisions about brain and optic nerve neuroimaging.[22]
Slit-lamp documentation of iris Lisch nodules can confirm the diagnosis of NF1. [Figure caption and citation for the preceding image starts]: Multiple Lisch nodules (pale yellow) on a blue irisFrom the personal collection of Dr Richard A. Lewis; used with permission [Citation ends].
central nervous system: signs of hydrocephalus, brain tumors, and/or cerebellar abnormalities
There may also be historical data.
Seizures of all types can be part of the NF1 diagnosis.
peripheral nervous system: palpable mass about neck, brachial plexuses, groin, Hunter canal, or the popliteal fossae
The peripheral nerves - primarily their sensory and autonomic elements - are primary targets of the NF1 mutation, from their origins in the dorsal root ganglia to intermediate and small nerves in the distal extremities.
Palpation around the neck, brachial plexuses, groin, Hunter canal, and popliteal fossae may be especially revealing.
These tumors feel like a hard rubber eraser and they are tender.
skeletal: tibial dysplasia or pseudarthrosis, sphenoid wing dysplasia, pectus excavatum or carinatum, genu valgum or varum, ankle valgus, pes planus
Tibial dysplasia or pseudarthrosis (actually also involving the adjacent fibula) is a hallmark lesion of infants and toddlers with NF1 (about 0.5%).[17]
Other skeletal lesions include sphenoid wing dysplasia (unilateral), pectus excavatum or carinatum, genu valgum or varum, ankle valgus, and pes planus.
gastrointestinal: severe constipation, obstipation, abdominal pain, gastrointestinal bleeding
Hyperganglionosis of the colon may lead to severe constipation or obstipation in both children and adults with NF1.
Gastrointestinal stromal tumors may cause abdominal pain and bleeding.
Carcinoid tumors tend to occur in the duodenum and cause facial flushing, diarrhea, right sided cardiac lesions, facial telangiectasia, and bronchoconstriction. The diagnosis is confirmed by increased urinary levels of the serotonin metabolite 5-hydroxyindoleacetic acid.
vascular: neurologic problems, abdominal pain (and/or hemorrhage)
Vascular abnormalities of the cerebral and gastrointestinal circulations may manifest as neurologic problems and abdominal pain (and/or hemorrhage), respectively.
autism spectrum disorder
21% to 40% of children with NF1 demonstrate an autism spectrum disorder based on diagnostic testing.[23]
uncommon
vascular: hypertension
Vascular abnormalities of the renal circulation may be manifest as hypertension.
Hypertension may be present if a pheochromocytoma develops. Most patients with pheochromocytoma present with continuously or paroxysmally increased blood pressure, or with episodic signs of flushing or palpitations. Although rare, a pheochromocytoma may also be recognized in an acute setting, in which patients present with an acute abdomen or collapse. About 15% of patients are asymptomatic, and the diagnosis is made coincidentally.[13]
Risk factors
strong
parent with NF1
NF1 is an autosomal-dominant genetic disorder with virtually 100% penetrance. There is a 50% risk for each pregnancy if one of the parents has NF1.
Use of this content is subject to our disclaimer