Approach
Diagnosis is based on defined clinical criteria, developed by the International Study Group for Behcet disease in 1990: patients virtually always have recurrent oral ulcers plus two other clinical manifestations (i.e., recurrent genital ulcers, skin lesions, eye lesions, or positive pathergy test).[16] Additional clinical manifestations may involve various organ systems, including the eye, gastrointestinal, vascular, pulmonary, and central nervous system (CNS).
A full history should be taken with particular attention to family history of the condition.
Laboratory testing and imaging are not useful in making the diagnosis of Behcet syndrome but do play a role in ruling out alternative diagnoses, or evaluating for complications of Behcet syndrome, such as vascular and CNS disorders.
Clinical manifestations
Oral and genital ulcers [Figure caption and citation for the preceding image starts]: Mouth and genital ulcersFrom the collection of Yusuf Yazici, MD [Citation ends].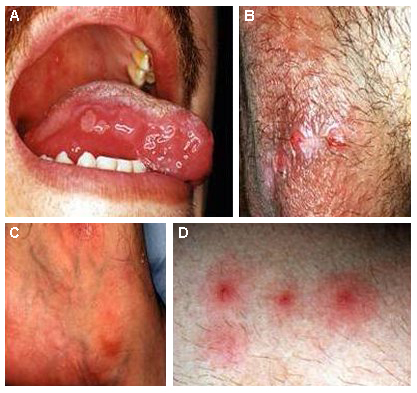
Many report recurrent oral ulcers; aphthous ulcers are the most common type seen.
Genital ulcerations can be painful and are usually on the scrotum or the labia. Large ulcers may scar, especially those on the scrotum.
Skin lesions may be papulopustular or nodular.
Acneiform lesions are similar to acne vulgaris, but may arise in atypical locations, for example, the arms and legs.
Erythema nodosum lesions are seen in about one-half of patients; unlike in other conditions, Behcet-associated lesions may ulcerate.
Superficial thrombophlebitis may be mistaken for erythema nodosum.
Pathergy reaction [Figure caption and citation for the preceding image starts]: PathergyFrom the collection of Yusuf Yazici, MD [Citation ends].
Elicited by performing a skin prick using a sterile needle and waiting 48 hours to see whether a papule or pustule forms.
Frequency of pathergy positivity is >60% in Turkey but <10% in the US.[10]
Eye involvement [Figure caption and citation for the preceding image starts]: HypopyonFrom the collection of Yusuf Yazici, MD [Citation ends].
Approximately one-half of patients have eye involvement with uveitis.[7]
More severe in men.[7]
Hypopyon, the precipitation of inflammatory cells in the anterior chamber of the eye, is seen in 20% of patients with eye involvement and is a marker for severe inflammation.[7] Hypopyon is virtually pathognomonic.[3]
Gastrointestinal involvement
Most common in eastern Asia; up to one third can have gastrointestinal involvement.[3]
Diarrhea, cramping abdominal pain, and mucosal ulcerations.
Major vessel involvement [Figure caption and citation for the preceding image starts]: Pulmonary aneurysmFrom the collection of Yusuf Yazici, MD [Citation ends].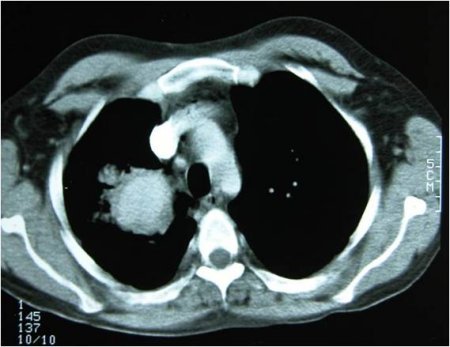
Rare. Possibilities include thrombophlebitis, deep vein thrombosis, cerebral venous thrombosis, and aneurysm formation.
Aneurysm formation can be life-threatening, especially in the pulmonary vasculature, when hemoptysis would be the presenting symptom.[17]
Parenchymal CNS involvement
Features of parenchymal involvement include memory impairment, mental status changes, hemiparesis, dizziness, loss of balance, seizures, cranial nerve palsies, or coma. There may be meningeal inflammation, with signs and symptoms of meningoencephalitis, including headache, confusion, and fever.[4][5]
Parenchymal disease in Behcet syndrome typically causes distinct white matter changes, commonly involving the midbrain, brainstem, and basal ganglia.[18]
Vascular CNS involvement
Cerebral venous thrombosis is the most common feature of vascular CNS involvement, and is marked by benign intracranial hypertension. Cerebral venous thrombosis is usually an extension of general vascular involvement in Behcet syndrome.[19]
Arterial stenosis, thrombosis, and aneurysm formation are less common manifestations of neurovascular Behcet syndrome.[2][6]
Nonerosive arthritis
Knees are most commonly involved; small joints can also be involved, but typically larger joints are targeted.
Laboratory tests
There are no tests specific for the syndrome itself. Laboratory testing may be useful in ruling out competing differential diagnoses.
Rheumatoid factor, antinuclear antibodies, and antineutrophil cytoplasmic antibodies are usually negative in Behcet syndrome.
Erythrocyte sedimentation rate and C-reactive protein may be mildly elevated, but these findings are nonspecific and therefore not diagnostically useful.
HLA-B51 may be positive. HLA-B51 is the most strongly associated known genetic factor for Behcet syndrome.[20] This association varies with ethnicity, although it is also seen in a healthy population. Positive HLA-B51 is more common in patients with Behcet syndrome, especially around the Mediterranean and in eastern Asian populations.[21] It may be an indicator of severity but this is still not well established.
In patients with gastrointestinal involvement, anti-Saccharomyces cerevisiae antibodies may be elevated but further studies are needed.[22]
In patients with suspected CNS involvement, cerebrospinal fluid (CSF) analysis is used to exclude infection as a cause of the patient's symptoms. In Behcet syndrome, the CSF may be hypercellular, with a predominance of lymphocytes, and, less frequently, polymorphonuclear cells or pleocytosis.[5]
Central nervous system imaging
Any neurologic symptoms should be evaluated promptly with magnetic resonance imaging (MRI), including magnetic resonance angiography of the brain.
MRI findings of the brain can be similar to those in multiple sclerosis, or there may be distinct white matter changes involving the midbrain, brainstem, and basal ganglia.[18]
Gastrointestinal endoscopy
Colonoscopy and/or upper gastrointestinal endoscopy may be required in those with gastrointestinal symptoms to rule out alternative diagnoses, such as Crohn disease or ulcerative colitis.
Behcet features on colonoscopy are usually distinct, single, deep ulcers. However, at times it may be difficult to differentiate from Crohn disease.
Lung imaging
Hemoptysis may be the only presenting symptom of pulmonary aneurysm in Behcet syndrome.
High-resolution chest computed tomography (CT) is recommended. CT angiography and invasive angiography are alternative studies if high-resolution chest CT does not confirm the diagnosis. High-resolution CT or CT angiography, chosen depending on the availability and local expertise, is used to screen for pulmonary aneurysm in patients with thrombophlebitis or other aneurysms (e.g., in the vena cava, hepatic veins).
Ophthalmologic evaluation
Symptoms of eye involvement may include eye pain, blurry vision, light sensitivity, eye redness, or tearing; however, posterior uveitis can present with minimal symptoms.
Consultation with an ophthalmology specialist is indicated for any visual changes or eye symptoms to evaluate for eye involvement, such as uveitis.
Use of this content is subject to our disclaimer