Tests
1st tests to order
transvaginal ultrasound
Test
Should be offered to all patients with suspected endometriosis.[1][36][49] The transvaginal ultrasound is used to: identify ovarian endometriomas and deep endometriosis (including that involving the bowel, bladder or ureter); identify or rule out alternative pathologies; guide management and enable referral to an appropriate service.[36] Note that a normal ultrasound scan does not exclude endometriosis and referral may still be appropriate.[36]
Confirmatory for endometriomas but criteria are less well-defined for peritoneal fibrosis. [Figure caption and citation for the preceding image starts]: Ultrasound of ovarian endometriomaFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].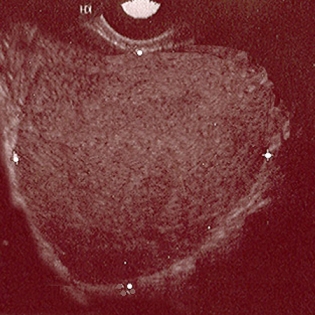
Sensitivity and specificity for detecting endometriomas is 93% and 96%, respectively.[39]
[  ]
]
Sensitivity is 58%, and specificity 96%, for detecting vaginal endometriosis. Sensitivity is 53% to 65%, and specificity 92% to 93% for detecting uterosacral ligament disease.[40][43]
Sensitivity 49%, and specificity 98% for detecting rectovaginal septal disease.[40]
Sensitivity is 89%, and specificity 97%, for rectosigmoid deep endometriosis.[44]
Sensitivity is 55%, and specificity 99%, for bladder deep endometriosis.[41]
Sensitivity is 31%, and specificity 98%, for parametrial deep endometriosis.[42]
Ultrasound exam is limited by retroverted uterus.
A negative uterine "sliding sign" predicts deep infiltrating endometriosis in the rectum.[45]
If a transvaginal ultrasound is unsuitable or declined by the patient, NICE recommends that a transabdominal ultrasound of the pelvis should be considered.[36]
Result
may show ovarian endometrioma (homogeneous, low-level echoes) or evidence of deep pelvic endometriosis such as uterosacral ligament involvement (hypoechoic linear thickening) or parametrium, bladder, or rectovaginal septum involvement
Tests to consider
rectal endoscopic ultrasound
Test
Designed to assess for uterosacral, rectovaginal and intestinal endometriosis. Rectal endoscopic ultrasound may be considered in women with suspected deep pelvic endometriosis or involvement of the colon/rectum, as this may help plan surgical resection.[39]
There is a growing body of literature demonstrating improved detection of deep pelvic disease with endoscopically guided endorectal ultrasound.
Sensitivity and specificity are at least 90% in most studies, but like transvaginal ultrasound, the available data are difficult to interpret.[52]
Result
hypoechoic nodule or mass
3D ultrasonography
Test
Less invasive than hysterosalpingography, hysteroscopy or laparoscopy and more cost-effective than MRI as a test to confirm mullerian anomalies.
Few comparative studies are available; limited to specialized centers.
Result
3-dimensional image of the endometrial cavity (varies based on type of anomaly)
hysterosalpingography
Test
Useful for women thought to have a mullerian anomaly (such as unicornuate uterus or uterine didelphys [double uterus]) which accounts for a small percentage of women with endometriosis.
A useful adjunct for women with subfertility.
Also evaluates tubal diameter and patency.
Result
contrast will delineate the endometrial cavity from surrounding/internal filling defects (varies based on type of mullerian anomaly)
MRI pelvis
Test
Useful for imaging the entire abdomen and pelvis. Ovarian disease can be easily seen. MRI can detect extra-pelvic and rectovaginal implants. MRI may be used to diagnose and assess the extent of deep endometriosis.[17][36][Figure caption and citation for the preceding image starts]: MRI - fibrotic nodules involving the uterosacral ligaments and rectal wallBazot M, et al. Radiology. 2004 Aug;232(2):379-89; used with permission [Citation ends].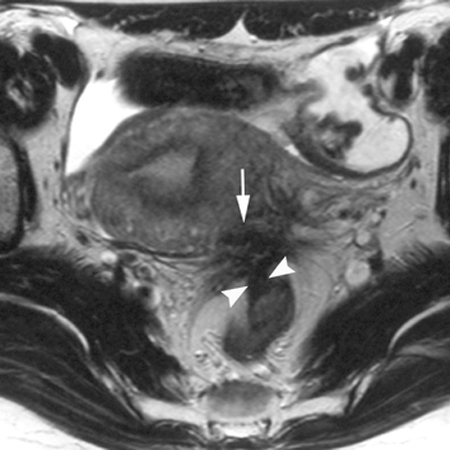
Sensitivity and specificity for deep pelvic disease is approximately 90%, but is consistently lower for uterosacral ligament and higher for gastrointestinal disease.[53]
NICE advises that pelvic MRI scans should be planned and interpreted by a professional with specialist expertise in gynecologic imaging.[36]
Result
hypointense, irregular thickening or mass of uterosacral ligament; replacement of fat tissue plane between uterus and rectum/sigmoid with tissue mass
diagnostic laparoscopy
Test
Direct visualization of implants at time of surgery and histopathology do not always correlate since there is no standardized method used by all pathologists and atypical lesions may be difficult to assess without biopsy. [Figure caption and citation for the preceding image starts]: Laparoscopic image of ovarian endometriomaFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].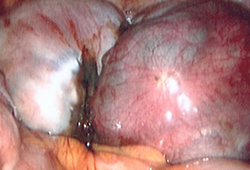 [Figure caption and citation for the preceding image starts]: Laparoscopic image of endometriotic noduleFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Laparoscopic image of endometriotic noduleFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Laparoscopic image of peritoneal windowFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Laparoscopic image of peritoneal windowFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].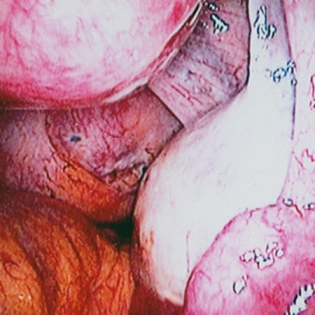 [Figure caption and citation for the preceding image starts]: Laparoscopic image of retroverted uterusFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Laparoscopic image of retroverted uterusFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].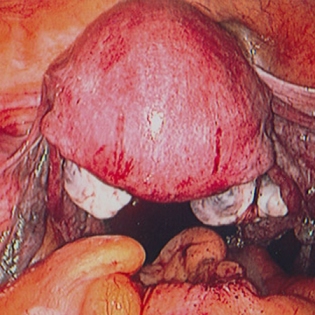
Surgical experience may increase the sensitivity to 97%.[54]
Diagnostic laparoscopy may be considered for suspected endometriosis even if other investigations (e.g., imaging) have been normal.[36]
Result
direct visualization with biopsy-confirmed endometrial glands or stroma outside of the uterine cavity. Early stage (minimal to mild) is marked by superficial peritoneal implants which appear vesicle-like (clear or red). Moderate disease is typically characterized by multiple superficial or deep lesions with a variable degree of adhesions. Advanced disease is typified by multiple implants (deep and fibrotic), parametrial or retroperitoneal extension, ovarian endometrioma, an obliterated cul-de-sac and pelvic adhesions.
Use of this content is subject to our disclaimer