Criteria
The gold standard for diagnosis of endometriosis is histologic verification of endometrial glands and stroma from surgically excised tissue specimens. However, surgical confirmation of disease is not required to initiate medical management. The use of preoperative imaging is associated with decreased morbidity and mortality and can aid patient decision making, surgical planning, and management.[49]
Revised American Society for Reproductive Medicine score[50]
The classification of endometriosis is typically based on visual inspection during laparoscopy. A cumulative score yields 4 stages (I to IV, or minimal to severe) and is based on:
The appearance, size and depth of peritoneal and ovarian implants
The presence, extent and type of lesions (red, red-pink and clear, white, peritoneal defects and black)
Presence, extent and type of pelvic adhesions (ovaries and tubes) and the degree of cul-de-sac obliteration.
Stage I (minimal): total score 1 to 5
Small, superficial peritoneal or adnexal implants (<1 to 3 cm); filmy adhesions.
Stage II (mild): total score 6 to 15
Larger lesions (>3 cm), some deeply infiltrating.
Stage III (moderate): total score 16 to 40
Larger lesions, more of which are infiltrative, partial cul-de-sac obliteration; dense adhesions involving adnexa.
Stage IV (severe): total score >40
Deep ovarian lesions (endometrioma) with dense adnexal adhesions; cul-de-sac obliteration.
This method of classification was designed to predict fertility outcomes, but has been criticized for its poor predictive power. Its utility for general practice should be limited to complete and reproducible operative documentation. Rather than computing a score after each case, a thorough dictation with specific implant/adhesion characteristics should be described.[Figure caption and citation for the preceding image starts]: Laparoscopic image of ovarian endometriomaFrom the collection of Dr Jonathon Solnik; used with permission [Citation ends].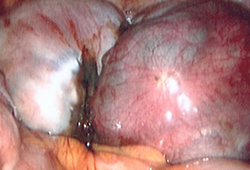
Use of this content is subject to our disclaimer