Approach
Clinical evaluation
The diagnosis of opioid overdose is primarily based on history and physical examination. History of opioid use or misuse is a key factor. This history is often unavailable from the patient and must be obtained from family or bystanders. Drug paraphernalia found with the patient may lead to a suspicion of opioid overdose. Other risk factors include recent abstinence from opioid use in chronic users and a history of chronic pain.[10][11] Opioid overdose should be considered in any patient with respiratory or cardiac arrest.[25][26]
Physical exam
A physical exam may reveal central nervous system depression, respiratory depression, and miosis, as well as decreased gastrointestinal motility and a relative bradycardia. A respiratory rate of 12 breaths/minute or less alone, or in combination with miosis or circumstantial evidence of opioid misuse, is highly sensitive in predicting the diagnosis in the prehospital setting.[27] Other clues are fresh needle marks or old track marks on the arms and legs.
Response to naloxone
A dramatic clinical response to naloxone in a patient who also fits the clinical or physical picture is diagnostic. The patient will immediately awaken and become responsive. In any patient who presents with altered mental status with bradypnea and miosis, a trial of naloxone should be considered. If there is no response, then another diagnosis should be sought. Higher doses of naloxone may be required before a response is seen in patients who have taken overdoses of opioids such as buprenorphine, fentanyl, or propoxyphene.
Electrocardiogram (ECG)
In patients with significant respiratory compromise, a 12-lead ECG should be performed to look for evidence of myocardial ischemia. QRS prolongation should be looked for in patients with propoxyphene overdose.
Imaging
Noncardiogenic pulmonary edema is a recognized complication of opioid overdose and is manifested by hypoxemia, pulmonary rales, and occasionally frothy pink sputum. A chest x-ray should be considered in all patients and may show signs of acute respiratory distress syndrome, including perihilar, basilar, or diffuse alveolar infiltrates.[Figure caption and citation for the preceding image starts]: Chest x-ray of acute respiratory distress syndrome in opioid overdoseFrom the collection of Dr Dean Olsen; used with permission [Citation ends].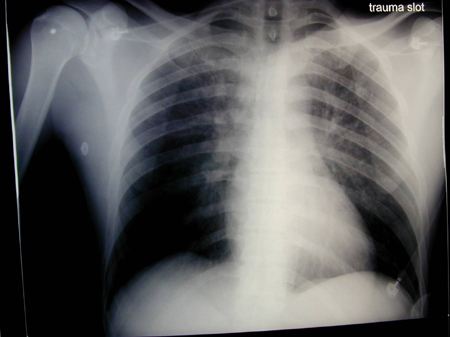
In suspected "body packers," imaging should be performed; in both symptomatic and asymptomatic patients abdominal x-ray may show evidence of packets throughout the gastrointestinal tract.[Figure caption and citation for the preceding image starts]: Abdominal x-ray showing multiple drug-filled packetsFrom the collection of Dr Dean Olsen; used with permission [Citation ends]. Occasionally, false-negative radiographic results occur, and patients with high suspicion of internal drug packets but negative abdominal x-rays should have an abdominal computed tomography scan.[28][29]
Occasionally, false-negative radiographic results occur, and patients with high suspicion of internal drug packets but negative abdominal x-rays should have an abdominal computed tomography scan.[28][29]
Urine testing
There are currently no laboratory tests available that can give a timely result to confirm or exclude the diagnosis. Although urine toxicology screens, which are available in most labs, can test for opioids, most are immunoassays that are specific for morphine and may not detect synthetic opioids. Because heroin and codeine are metabolized to morphine, these will also be detected. These tests are not available in a helpful time frame because of the need for rapid intervention, which cannot be withheld while awaiting laboratory results. In addition, as opioids are chemically detectable in the urine several days after use, a positive test result, even on point of care testing, does not confirm recent overdose.
In "body packers" with an initial negative urine screen for opioids, repeated tests may be useful in identifying or excluding leakage from ingested packages.
Gas chromatography/mass spectrometry
Gas chromatography and mass spectrometry are the most sensitive and specific tests to detect opioids in the serum, but are not clinically useful due to the high cost and long turnaround time. These are most commonly used for forensic cases or workplace testing. They are never used for overdose or clinical practice.
Use of this content is subject to our disclaimer