Tests
1st tests to order
urinalysis and microscopy
Test
Indicated in all patients with suspected granulomatosis with polyangiitis (GPA) disease.[22] Earliest indicators of renal involvement, detectable prior to elevated serum creatinine.
Result
may show hematuria, proteinuria; dysmorphic red blood cells, RBC casts
CT chest
Test
Chest imaging is indicated in all patients with suspected disease, as lung involvement is asymptomatic in one third of patients.[22] [Figure caption and citation for the preceding image starts]: Cavitary lung nodules in granulomatosis with polyangiitis (formerly known as Wegener granulomatosis)From the collection of Dr Eamonn Molloy, used with permission [Citation ends].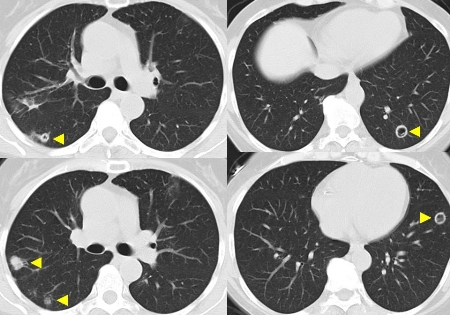
Chest CT is preferred to chest x-ray because of its greater sensitivity for detecting lung involvement.[33]
Result
lung nodules (which may cavitate); infiltrates
antineutrophil cytoplasmic antibody (ANCA)
Test
Antigen-specific immunoassay for proteinase 3 (PR3)-ANCAs and myeloperoxidase (MPO)-ANCAs is the preferred first screening method for ANCA-associated vasculitides.[28]
If immunoassay results are negative or equivocal, and a strong suspicion of GPA persists, indirect immunofluorescence may be performed.[28]
A positive ANCA test in the setting of typical symptoms is generally sufficient for diagnosis.
A negative ANCA test does not rule out GPA.[28] Between 9% and 16% of patients with GPA have a negative ANCA immunoassay.[30][31]
A positive ANCA may also be seen in other settings, such as infections (e.g., infective endocarditis, mycobacterial and parasitic infections), other systemic inflammatory disorders, gastrointestinal disorders (e.g., inflammatory bowel disease, autoimmune hepatitis), malignancy, and drug exposures (e.g., cocaine, propylthiouracil, minocycline). These conditions should be considered in the differential diagnosis and, in cases where doubt exists, histologic confirmation of the diagnosis should be sought.[28]
Result
positive proteinase 3 (PR3)-ANCA on antigen-specific immunoassay; cANCA (cytoplasmic pattern) on immunofluorescence testing
CBC and differential
Test
Anemia may be related to a number of factors, such as disease activity, renal insufficiency, and pulmonary hemorrhage.
Thrombocytopenia or leukopenia in patients not previously treated with myelotoxic immunosuppressive therapy should prompt consideration of alternative diagnoses such as systemic lupus erythematosus or thrombotic thrombocytopenic purpura.
Result
anemia
serum creatinine
Test
A normal result does not rule out glomerulonephritis. Serum creatinine may also be elevated due to other factors such as intercurrent sepsis, medication effects, or, rarely, obstructive uropathy due to granulomatosis with polyangiitis (GPA) (formerly known as Wegener granulomatosis). Levels may change rapidly in the acute phase of GPA, so frequent monitoring is advised.
Result
elevated
C-reactive protein
Test
Nonspecific marker of inflammation.
Result
elevated
erythrocyte sedimentation rate (ESR)
Test
An elevated ESR is a typical finding, but it is nonspecific. ESR may be normal, especially in less severe disease presentations. ESR may be influenced by many other factors such as anemia, renal failure, intercurrent infection, and malignancy.
Result
elevated
liver function tests
Test
Typically normal or near-normal; abnormalities suggest an alternative diagnosis such as cancer or infection. Serum albumin may be low due to proteinuria and/or inflammation.[22]
Result
normal or low albumin
serum calcium
Test
Typically normal or near-normal; abnormalities suggest an alternative diagnosis such as cancer or infection.[22]
Result
normal
Tests to consider
tissue biopsy
Test
Biopsy may be indicated to support the diagnosis, depending on the presence of other clinical, laboratory, and imaging criteria.[21] Biopsies of the affected organs are recommended for patients with negative antineutrophil cytoplasmic antibody (ANCA) test results.[28]
Yield from upper respiratory and transbronchial biopsies is low (<10%), so these techniques cannot be relied upon to rule out GPA. Open lung biopsy has a higher yield.
Renal biopsy can be helpful in confirming the presence of glomerulonephritis and excluding other potential renal diagnoses. The lesions in GPA are indistinguishable from those of microscopic polyangiitis and renal-limited pauci-immune glomerulonephritis. However, in the context of the overall signs, symptoms, and laboratory results, it can provide useful supporting evidence for the diagnosis of GPA.
Skin biopsy shows leukocytoclastic vasculitis, which, although nonspecific for GPA, provides useful evidence of a vasculitic process.
Result
granulomatous inflammation, necrosis and vasculitis; minimal/absent immune deposits on immunofluorescence, and electron microscopy
pulmonary function testing
Test
An elevated diffusion capacity is suggestive for pulmonary hemorrhage (which may present as infiltrates without hemoptysis).
An abnormal, box-like, flow-volume loop is suggestive of subglottic airway stenosis.
Result
elevated diffusion capacity; abnormal box-like flow volume loop
bronchoscopy
Test
Can be helpful for detection of subclinical pulmonary hemorrhage. Microbiologic studies of bronchoalveolar lavage ± transbronchial biopsy specimens important to exclude infection, especially in patients treated with immunosuppressive agents.
Transbronchial biopsies have a low yield (<10%) for diagnosis, but may help identify competing diagnoses such as infection and malignancy.
Result
hemorrhage; hemosiderosis; detection of infectious agents
electromyography/nerve conduction studies
Test
Indicated only for patients with compatible neurologic symptoms and signs.
Result
peripheral sensorimotor polyneuropathy; mononeuritis multiplex
upper airway endoscopy
Test
Direct visualization of upper airway lesions also facilitates local management, e.g., with dilatation and corticosteroid injection of subglottic stenosis, debridement of extensive nasal crusting, or obtaining specimens for microbiologic testing.
Result
subglottic stenosis; nasal crusting/inflammation/septal perforation/sinusitis
CT sinuses
Test
Mucosal thickening is frequently seen, but is nonspecific. Pan-sinusitis may be seen. Bony reactive changes may be seen with chronic disease. Perforation of a bony structure other than the lamina papyracea implies an alternative diagnosis such as infection or malignancy.
Result
sinusitis; mucocele
Use of this content is subject to our disclaimer