Approach
The most common presentation of HL is persistent cervical and/or supraclavicular lymphadenopathy in a young adult.
HL mainly occurs in early (age 20-34 years) or late adulthood (over 55 years).[6][7][8]
Signs and symptoms
Most patients present with a several-month history of persistent lymphadenopathy, which has often been treated empirically with antibiotics. The cervical chain is the most commonly involved site.
Systemic symptoms, referred to as B symptoms, occur in up to 30% of patients and include unexplained recurrent fevers (≥100.4°F [≥38°C]), drenching night sweats necessitating change of bedclothes, and/or unexplained weight loss of >10% of baseline weight in the preceding 6 months.[4][5] These symptoms are typically associated with advanced disease (stage III to IV), and are more common in older patients (ages >60 years).[33]
Other systemic symptoms include localized or generalized pruritus and alcohol-induced pain at involved sites. Symptoms from enlarged lymph nodes, such as shortness of breath, cough, chest pain, abdominal pain, or superior vena cava syndrome, may occur but are less common.
Clinical assessment
Clinical examination should focus on the lymphatic system, including the cervical, supraclavicular, axillary, and inguinal lymph node chains. Documentation of size, mobility, and tenderness of palpable lymph nodes should be performed.
The abdomen should be examined for hepatomegaly or splenomegaly. The oropharynx should be evaluated for tonsillar enlargement.
A dental evaluation should be carried out because radiation therapy can cause xerostomia and increased caries.
Laboratory evaluation
Complete blood count with differential, comprehensive metabolic panel (including alkaline phosphatase, lactate dehydrogenase, liver enzymes, and albumin), and an erythrocyte sedimentation rate are required as part of the diagnostic workup.
Baseline thyroid function tests are required, particularly in patients receiving radiation therapy to the neck. Radiation therapy to the neck can increase the risk of developing thyroid dysfunction.
Screening for HIV and hepatitis B and C should be carried out as infection with these viruses may complicate treatment for HL.
Pathology
Pathologic confirmation via biopsy is the only acceptable method of diagnosing HL and is essential before treatment can commence. An excisional biopsy of an enlarged lymph node is recommended.[5][33] Under certain circumstances a core biopsy can be adequate. A fine-needle aspiration biopsy is never suitable for diagnosing HL.
HL is characterized by the identification of Hodgkin cells with an appropriate background cellular milieu. The Hodgkin cell can be a characteristic Reed-Sternberg cell or one of its variants, such as the lacunar cell in the nodular sclerosis subtype. For nodular lymphocyte-predominant HL, the characteristic cell is the lymphocytic and histiocytic (L&H) cell, also referred to as a popcorn cell.
Immunohistochemical studies, which are routinely obtained as part of the pathologic assessment, are invaluable in differentiating HL from other lymphomas as well as nonhematologic processes.[Figure caption and citation for the preceding image starts]: A diagnostic Reed-Sternberg cell is seen in the center of the imageFrom the personal collection of CR Kelsey [Citation ends].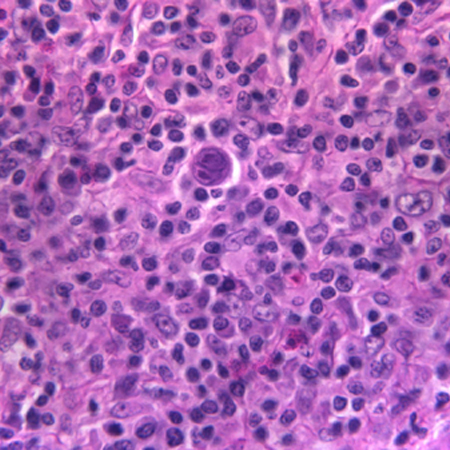
Imaging and staging
Positron emission tomography/computed tomography (PET/CT) imaging (where available) should be carried out at diagnosis to evaluate the extent of disease (i.e., stage), and throughout treatment to monitor treatment response and guide management.[34][35]
A pre-treatment PET/CT is recommended to facilitate interpretation of post-treatment PET/CT scans.[36][37]
Patients adequately staged with PET/CT do not require a bone marrow biopsy to evaluate bone involvement.[38] However, a bone marrow biopsy may be required if PET/CT is unavailable, or if a patient has a negative PET/CT and unexplained thrombocytopenia or neutropenia.[5][33]
A gallium scan, supplemented with contrast-enhanced CT of the neck, chest, abdomen, and pelvis, can be used if PET/CT is unavailable.
A chest x-ray at diagnosis is helpful to evaluate for bulky mediastinal adenopathy.[Figure caption and citation for the preceding image starts]: CXR of patient presenting with dyspnea, showing widened mediastinum and tracheal displacementFrom the personal collection of CR Kelsey [Citation ends]. [Figure caption and citation for the preceding image starts]: CT scan of patient with nodular sclerosis Hodgkin lymphoma, showing an 11-cm anterior mediastinal massFrom the personal collection of CR Kelsey [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan of patient with nodular sclerosis Hodgkin lymphoma, showing an 11-cm anterior mediastinal massFrom the personal collection of CR Kelsey [Citation ends]. [Figure caption and citation for the preceding image starts]: PET scan (axial) showing fluorodeoxyglucose (FDG)-avid mass in the anterior mediastinumFrom the personal collection of CR Kelsey [Citation ends].
[Figure caption and citation for the preceding image starts]: PET scan (axial) showing fluorodeoxyglucose (FDG)-avid mass in the anterior mediastinumFrom the personal collection of CR Kelsey [Citation ends].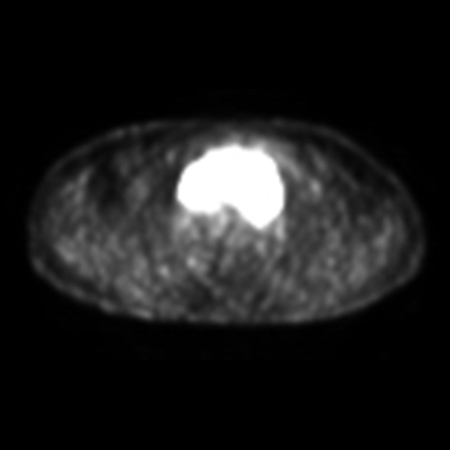 [Figure caption and citation for the preceding image starts]: PET scan (coronal) showing fluorodeoxyglucose (FDG)-avid mass in the superior mediastinumFrom the personal collection of CR Kelsey [Citation ends].
[Figure caption and citation for the preceding image starts]: PET scan (coronal) showing fluorodeoxyglucose (FDG)-avid mass in the superior mediastinumFrom the personal collection of CR Kelsey [Citation ends].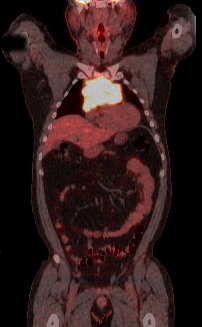
Physiologic evaluation
Baseline pulmonary function tests are important in patients receiving mediastinal radiation therapy and/or chemotherapy with potential for pulmonary toxicity (e.g., bleomycin).
A baseline cardiac evaluation (echocardiogram or multigated acquisition scan) is required in those patients receiving potentially cardiotoxic chemotherapy agents (e.g., anthracyclines).
Use of this content is subject to our disclaimer