The treatment of ileus focuses on supportive care and correction of any underlying or predisposing conditions.
General management in all patients
All patients with ileus are made nothing by mouth (NPO) and require intravenous hydration. The initial choice of intravenous solution will depend on the baseline hydration state of the patient and the presence of comorbidities. A significantly hypovolemic patient may benefit from a bolus of several liters of normal saline. Following this initial hydration, the maintenance intravenous solution should be physiologic and provide some glucose. Fluids should be administered at a maintenance rate according to body weight. This rate should be tailored to the patient's urine output and hemodynamics.
Once ileus begins to resolve, as seen by passage of flatus and resolution of abdominal distention and nausea, the patient can be started on a liquid diet and advanced as tolerated.
Postoperative ileus
Attempts to prevent postoperative ileus should begin in the perioperative setting, including appropriate intra-operative fluid management and avoidance of opioid analgesia. Enhanced recovery after surgery (ERAS) pathways are increasingly utilized in an attempt to expedite recovery of intestinal function and shorten hospital length of stay.[3]Wattchow D, Heitmann P, Smolilo D, et al. Postoperative ileus- an ongoing conundrum. Neurogastroenterol Motil. 2021 May;33(5):e14046.
http://www.ncbi.nlm.nih.gov/pubmed/33252179?tool=bestpractice.com
[28]Gustafsson UO, Scott MJ, Hubner M, et al. Guidelines for perioperative care in elective colorectal surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations: 2018. World J Surg. 2019 Mar;43(3):659-95.
https://link.springer.com/article/10.1007/s00268-018-4844-y
http://www.ncbi.nlm.nih.gov/pubmed/30426190?tool=bestpractice.com
[32]Hedrick TL, McEvoy MD, Mythen MMG, et al. American Society for Enhanced Recovery and Perioperative Quality Initiative joint consensus statement on postoperative gastrointestinal dysfunction within an enhanced recovery pathway for elective colorectal surgery. Anesth Analg. 2018 Jun;126(6):1896-907.
https://journals.lww.com/anesthesia-analgesia/fulltext/2018/06000/american_society_for_enhanced_recovery_and.20.aspx
http://www.ncbi.nlm.nih.gov/pubmed/29293183?tool=bestpractice.com
The mainstays of ERAS pathways include minimally invasive surgery, avoiding opioids, multimodal pain control, early ambulation, and early intake of oral fluids and solids.[3]Wattchow D, Heitmann P, Smolilo D, et al. Postoperative ileus- an ongoing conundrum. Neurogastroenterol Motil. 2021 May;33(5):e14046.
http://www.ncbi.nlm.nih.gov/pubmed/33252179?tool=bestpractice.com
[28]Gustafsson UO, Scott MJ, Hubner M, et al. Guidelines for perioperative care in elective colorectal surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations: 2018. World J Surg. 2019 Mar;43(3):659-95.
https://link.springer.com/article/10.1007/s00268-018-4844-y
http://www.ncbi.nlm.nih.gov/pubmed/30426190?tool=bestpractice.com
[31]Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg. 2017 Mar 1;152(3):292-8.
http://www.ncbi.nlm.nih.gov/pubmed/28097305?tool=bestpractice.com
[32]Hedrick TL, McEvoy MD, Mythen MMG, et al. American Society for Enhanced Recovery and Perioperative Quality Initiative joint consensus statement on postoperative gastrointestinal dysfunction within an enhanced recovery pathway for elective colorectal surgery. Anesth Analg. 2018 Jun;126(6):1896-907.
https://journals.lww.com/anesthesia-analgesia/fulltext/2018/06000/american_society_for_enhanced_recovery_and.20.aspx
http://www.ncbi.nlm.nih.gov/pubmed/29293183?tool=bestpractice.com
In patients undergoing surgery and requiring opioid analgesia, decreasing the use of systemically administered opioid analgesics helps to prevent postoperative ileus.[28]Gustafsson UO, Scott MJ, Hubner M, et al. Guidelines for perioperative care in elective colorectal surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations: 2018. World J Surg. 2019 Mar;43(3):659-95.
https://link.springer.com/article/10.1007/s00268-018-4844-y
http://www.ncbi.nlm.nih.gov/pubmed/30426190?tool=bestpractice.com
Patient-controlled analgesia pumps are beneficial as they reduce the overall amount of opioid given compared with round-the-clock analgesic dosing administered by a nurse.[33]Chan KC, Cheng YJ, Huang GT, et al. The effect of IVPCA morphine on post-hysterectomy bowel function. Acta Anaesthesiol Sin. 2002 Jun;40(2):61-4.
http://www.ncbi.nlm.nih.gov/pubmed/12194392?tool=bestpractice.com
Useful adjuncts for pain management include nonsteroidal anti-inflammatory drugs (NSAIDs) such as ketorolac, other nonopioid analgesics such as acetaminophen, and local anesthetics administered via epidural.[3]Wattchow D, Heitmann P, Smolilo D, et al. Postoperative ileus- an ongoing conundrum. Neurogastroenterol Motil. 2021 May;33(5):e14046.
http://www.ncbi.nlm.nih.gov/pubmed/33252179?tool=bestpractice.com
[34]Senagore AJ, Delaney CP, Mekhail N, et al. Randomized clinical trial comparing epidural anaesthesia and patient-controlled analgesia after laparoscopic segmental colectomy. Br J Surg. 2003 Oct;90(10):1195-9.
http://www.ncbi.nlm.nih.gov/pubmed/14515286?tool=bestpractice.com
[35]Marret E, Remy C, Bonnet F. Meta-analysis of epidural analgesia versus parenteral opioid analgesia after colorectal surgery. Br J Surg. 2007 Jun;94(6):665-73.
https://onlinelibrary.wiley.com/doi/full/10.1002/bjs.5825
http://www.ncbi.nlm.nih.gov/pubmed/17514701?tool=bestpractice.com
[36]Gendall KA, Kennedy RR, Watson AJ, et al. The effect of epidural analgesia on postoperative outcome after colorectal surgery. Colorectal Dis. 2007 Sep;9(7):584-98;discussion 598-600.
http://www.ncbi.nlm.nih.gov/pubmed/17506795?tool=bestpractice.com
[37]Carli F, Trudel JL, Belliveau P. The effect of intraoperative thoracic epidural anesthesia and postoperative analgesia on bowel function after colorectal surgery: a prospective, randomized trial. Dis Colon Rectum. 2001 Aug;44(8):1083-9.
http://www.ncbi.nlm.nih.gov/pubmed/11535845?tool=bestpractice.com
[38]Schlachta CM, Burpee SE, Fernandez C, et al. Optimizing recovery after laparoscopic colon surgery (ORAL-CS): effect of intravenous ketorolac on length of hospital stay. Surg Endosc. 2007 Dec;21(12):2212-9.
http://www.ncbi.nlm.nih.gov/pubmed/17440782?tool=bestpractice.com
[39]Chen JY, Wu GJ, Mok MS, et al. Effect of adding ketorolac to intravenous morphine patient-controlled analgesia on bowel function in colorectal surgery patients: a prospective, randomized, double-blind study. Acta Anaesthesiol Scand. 2005 Apr;49(4):546-51.
http://www.ncbi.nlm.nih.gov/pubmed/15777304?tool=bestpractice.com
[40]McNicol ED, Ferguson MC, Schumann R. Single-dose intravenous ketorolac for acute postoperative pain in adults. Cochrane Database Syst Rev. 2021 May 17;5(5):CD013263.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD013263.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/33998669?tool=bestpractice.com
[41]Bell S, Rennie T, Marwick CA, et al. Effects of peri-operative nonsteroidal anti-inflammatory drugs on post-operative kidney function for adults with normal kidney function. Cochrane Database Syst Rev. 2018 Nov 29;11(11):CD011274.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011274.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/30488949?tool=bestpractice.com
[42]Chen JY, Ko TL, Wen YR, et al. Opioid-sparing effects of ketorolac and its correlation with the recovery of postoperative bowel function in colorectal surgery patients: a prospective randomized double-blinded study. Clin J Pain. 2009 Jul-Aug;25(6):485-9.
http://www.ncbi.nlm.nih.gov/pubmed/19542795?tool=bestpractice.com
[53]Guay J, Nishimori M, Kopp SL. Epidural local anesthetics versus opioid-based analgesic regimens for postoperative gastrointestinal paralysis, vomiting, and pain after abdominal surgery: a Cochrane review. Anesth Analg. 2016 Dec;123(6):1591-602.
https://journals.lww.com/anesthesia-analgesia/fulltext/2016/12000/epidural_local_anesthetics_versus_opioid_based.33.aspx
http://www.ncbi.nlm.nih.gov/pubmed/27870743?tool=bestpractice.com
[85]Blank JJ, Berger NG, Dux JP, et al. The impact of intravenous acetaminophen on pain after abdominal surgery: a meta-analysis. J Surg Res. 2018 Jul;227:234-45.
http://www.ncbi.nlm.nih.gov/pubmed/29804858?tool=bestpractice.com
[86]Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016 Feb;17(2):131-57.
https://www.doi.org/10.1016/j.jpain.2015.12.008
http://www.ncbi.nlm.nih.gov/pubmed/26827847?tool=bestpractice.com
Several randomized controlled trials and meta-analyses have shown decreased duration of postoperative ileus in patients given chewing gum after surgery.[60]Yeh YC, Klinger EV, Reddy P. Pharmacologic options to prevent postoperative ileus. Ann Pharmacother. 2009 Sep;43(9):1474-85.
http://www.ncbi.nlm.nih.gov/pubmed/19602600?tool=bestpractice.com
[68]Vasquez W, Hernandez AV, Garcia-Sabrido JL, et al. Is gum chewing useful for ileus after elective colorectal surgery? A systematic review and meta-analysis of randomized clinical trials. J Gastrointest Surg. 2009 Apr;13(4):649-56.
http://www.ncbi.nlm.nih.gov/pubmed/19050983?tool=bestpractice.com
[69]Purkayastha S, Tilney HS, Darzi AW, et al. Meta-analysis of randomized studies evaluating chewing gum to enhance postoperative recovery following colectomy. Arch Surg. 2008 Aug;143(8):788-93.
http://archsurg.ama-assn.org/cgi/reprint/143/8/788
http://www.ncbi.nlm.nih.gov/pubmed/18711040?tool=bestpractice.com
[70]Noble EJH, Harris R, Hosie KB, et al. Gum chewing reduces postoperative ileus? A systematic review and meta-analysis. Int J Surg. 2009 Apr;7(2):100-5.
https://www.sciencedirect.com/science/article/pii/S1743919109000089?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/19261555?tool=bestpractice.com
[71]Fitzgerald JE, Ahmed I. Systematic review and meta-analysis of chewing-gum therapy in the reduction of postoperative paralytic ileus following gastrointestinal surgery. World J Surg. 2009 Dec;33(12):2557-66.
http://www.ncbi.nlm.nih.gov/pubmed/19763686?tool=bestpractice.com
[72]Short V, Herbert G, Perry R, et al. Chewing gum for postoperative recovery of gastrointestinal function. Cochrane Database Syst Rev. 2015 Feb 20;(2):CD006506.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD006506.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/25914904?tool=bestpractice.com
[73]van den Heijkant TC, Costes LM, van der Lee DG, et al. Randomized clinical trial of the effect of gum chewing on postoperative ileus and inflammation in colorectal surgery. Br J Surg. 2015 Feb;102(3):202-11.
http://www.ncbi.nlm.nih.gov/pubmed/25524125?tool=bestpractice.com
[74]Zhu YP, Wang WJ, Zhang SL, et al. Effects of gum chewing on postoperative bowel motility after caesarean section: a meta-analysis of randomised controlled trials. BJOG. 2014 Jun;121(7):787-92.
http://onlinelibrary.wiley.com/doi/10.1111/1471-0528.12662/full
http://www.ncbi.nlm.nih.gov/pubmed/24629205?tool=bestpractice.com
[75]Andersson T, Bjerså K, Falk K, et al. Effects of chewing gum against postoperative ileus after pancreaticoduodenectomy - a randomized controlled trial. BMC Res Notes. 2015 Feb 10;8:37.
http://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-015-0996-0
http://www.ncbi.nlm.nih.gov/pubmed/25886536?tool=bestpractice.com
It is a safe and easy modality that can be utilized in most patients; however, it is not routinely recommended because the quality of evidence is very low.[28]Gustafsson UO, Scott MJ, Hubner M, et al. Guidelines for perioperative care in elective colorectal surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations: 2018. World J Surg. 2019 Mar;43(3):659-95.
https://link.springer.com/article/10.1007/s00268-018-4844-y
http://www.ncbi.nlm.nih.gov/pubmed/30426190?tool=bestpractice.com
[76]Pereira Gomes Morais E, Riera R, Porfírio GJ, et al. Chewing gum for enhancing early recovery of bowel function after caesarean section. Cochrane Database Syst Rev. 2016 Oct 17;10(10):CD011562.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011562.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/27747876?tool=bestpractice.com
Patients with significant abdominal distention and repeated vomiting should have a nasogastric (NG) tube placed.[3]Wattchow D, Heitmann P, Smolilo D, et al. Postoperative ileus- an ongoing conundrum. Neurogastroenterol Motil. 2021 May;33(5):e14046.
http://www.ncbi.nlm.nih.gov/pubmed/33252179?tool=bestpractice.com
[32]Hedrick TL, McEvoy MD, Mythen MMG, et al. American Society for Enhanced Recovery and Perioperative Quality Initiative joint consensus statement on postoperative gastrointestinal dysfunction within an enhanced recovery pathway for elective colorectal surgery. Anesth Analg. 2018 Jun;126(6):1896-907.
https://journals.lww.com/anesthesia-analgesia/fulltext/2018/06000/american_society_for_enhanced_recovery_and.20.aspx
http://www.ncbi.nlm.nih.gov/pubmed/29293183?tool=bestpractice.com
Gastric output should be measured and lost volume should be replaced with an intravenous physiologic saline solution. The decision to remove the NG tube is based on measured gastric output over time and clinical resolution of ileus. The patient is assessed for absence of abdominal distention and cramping, decreasing NG tube output, and passage of flatus and stool with a view to removal of the NG tube. The NG tube may require reinsertion if the patient again displays evidence of ongoing ileus with abdominal distention and vomiting. Studies have shown that routine NG decompression is unnecessary and may be detrimental.[87]Nelson R, Edwards S, Tse B. Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev. 2007 Jul 18;(3):CD004929.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004929.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/17636780?tool=bestpractice.com
Therefore, routine NG decompression is reserved for selective use.[87]Nelson R, Edwards S, Tse B. Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev. 2007 Jul 18;(3):CD004929.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004929.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/17636780?tool=bestpractice.com
Often, orogastric decompression is performed intra-operatively, but the tube is removed at the completion of surgery.[28]Gustafsson UO, Scott MJ, Hubner M, et al. Guidelines for perioperative care in elective colorectal surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations: 2018. World J Surg. 2019 Mar;43(3):659-95.
https://link.springer.com/article/10.1007/s00268-018-4844-y
http://www.ncbi.nlm.nih.gov/pubmed/30426190?tool=bestpractice.com
Patients with prolonged postoperative ileus (ileus on or after day 4 postsurgery without prior resolution of postoperative ileus) may not have any oral intake for several weeks. Parenteral nutrition is recommended for patients who do not have any oral intake for more than 7 days.[3]Wattchow D, Heitmann P, Smolilo D, et al. Postoperative ileus- an ongoing conundrum. Neurogastroenterol Motil. 2021 May;33(5):e14046.
http://www.ncbi.nlm.nih.gov/pubmed/33252179?tool=bestpractice.com
[78]Gero D, Gié O, Hübner M, et al. Postoperative ileus: in search of an international consensus on definition, diagnosis, and treatment. Langenbecks Arch Surg. 2017 Feb;402(1):149-58.
http://www.ncbi.nlm.nih.gov/pubmed/27488952?tool=bestpractice.com
It is beneficial in patients who are on bowel rest for more than 14 days or who have underlying malnutrition.[88]Sandstrom R, Drott C, Hyltander A, et al. The effect of postoperative intravenous feeding (TPN) on outcome following major surgery evaluated in a randomized study. Ann Surg. 1993 Feb;217(2):185-95.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1242758
http://www.ncbi.nlm.nih.gov/pubmed/8439216?tool=bestpractice.com
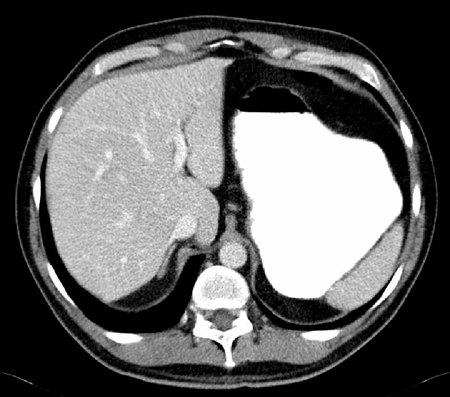
Electrolytes should be checked daily to identify electrolyte abnormalities associated with postoperative intravenous feeding and the NPO state. The benefits of starting parenteral nutrition earlier than 7 days are fewer than the risks associated with parenteral nutrition and central venous access. In most patients, the postoperative "starvation" state is not associated with increased morbidity or mortality. Insertion of a central venous line is associated with increased risk of iatrogenic injury to nearby vessels, pneumothorax, deep vein thrombosis, and central line-associated bacteremia. [Figure caption and citation for the preceding image starts]: CT scan showing significantly dilated stomachFrom the personal collection of Dr Paula I. Denoya [Citation ends].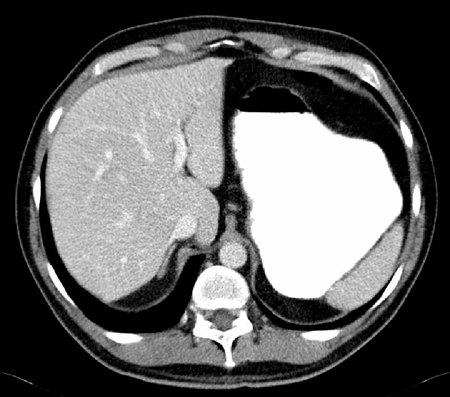 [Figure caption and citation for the preceding image starts]: Nasogastric tubeFrom the personal collection of Dr Paula I. Denoya [Citation ends].
[Figure caption and citation for the preceding image starts]: Nasogastric tubeFrom the personal collection of Dr Paula I. Denoya [Citation ends].
Management of underlying causes
Underlying conditions, such as sepsis, intra-abdominal infections, or other acute/systemic illnesses should be treated.
Some pharmacologic agents (e.g., opioids, anticholinergics) reduce gastrointestinal motility and can cause ileus, so these should be discontinued or reduced. Chronic opioid use contributes to ileus, but cessation or reduction of opioids should be managed carefully in these patients due to the risk of withdrawal symptoms.[89]Cunningham C, Edlund MJ, Fishman M, et al. The ASAM national practice guideline for the treatment of opioid use Disorder: 2020 focused update. J Addict Med. 2020 Mar/Apr;14(2s suppl 1):1-91.
https://journals.lww.com/journaladdictionmedicine/fulltext/2020/04001/the_asam_national_practice_guideline_for_the.1.aspx
http://www.ncbi.nlm.nih.gov/pubmed/32511106?tool=bestpractice.com
[90]Müller-Lissner S, Bassotti G, Coffin B, et al. Opioid-induced constipation and bowel dysfunction: a clinical Guideline. Pain Med. 2017 Oct 1;18(10):1837-63.
https://pmc.ncbi.nlm.nih.gov/articles/PMC5914368
http://www.ncbi.nlm.nih.gov/pubmed/28034973?tool=bestpractice.com
Electrolyte imbalance, particularly hypermagnesemia, has been associated with ileus.[82]Golzarian J, Scott HW Jr, Richards WO. Hypermagnesemia-induced paralytic ileus. Dig Dis Sci. 1994 May;39(5):1138-42.
http://www.ncbi.nlm.nih.gov/pubmed/8174429?tool=bestpractice.com
Electrolytes should be monitored and corrected as necessary.
Other evaluated therapies
In patients with acute small bowel obstruction as a result of adhesions, there is some evidence that water-soluble contrast agents (e.g., diatrizoate meglumine/diatrizoate sodium solution [Gastrografin®]) are an effective treatment, avoiding surgery, as well as correlating with a reduction in hospital stay.[3]Wattchow D, Heitmann P, Smolilo D, et al. Postoperative ileus- an ongoing conundrum. Neurogastroenterol Motil. 2021 May;33(5):e14046.
http://www.ncbi.nlm.nih.gov/pubmed/33252179?tool=bestpractice.com
[91]Ceresoli M, Coccolini F, Catena F, et al. Water-soluble contrast agent in adhesive small bowel obstruction: a systematic review and meta-analysis of diagnostic and therapeutic value. Am J Surg. 2016 Jun;211(6):1114-25.
http://www.ncbi.nlm.nih.gov/pubmed/26329902?tool=bestpractice.com
However, two small double-blind placebo-controlled trials of patients with prolonged postoperative ileus after elective colorectal surgery suggest that Gastrografin® is of limited clinical utility in these patients, and the therapeutic value of these treatments remains controversial and uncertain.[77]American College of Radiology. ACR appropriateness criteria: suspected small-bowel obstruction. 2019 [internet publication].
https://acsearch.acr.org/docs/69476/Narrative
[92]Biondo S, Miquel J, Espin-Basany E, et al. A double-blinded randomized clinical study on the therapeutic effect of gastrografin in prolonged postoperative ileus after elective colorectal surgery. World J Surg. 2016 Jan;40(1):206-14.
http://www.ncbi.nlm.nih.gov/pubmed/26446450?tool=bestpractice.com
[93]Vather R, Josephson R, Jaung R, et al. Gastrografin in prolonged postoperative ileus: a double-blinded randomized controlled trial. Ann Surg. 2015 Jul;262(1):23-30.
http://www.ncbi.nlm.nih.gov/pubmed/25575258?tool=bestpractice.com
Promotility agents have been used to treat ileus with limited success.[64]Traut U, Brügger L, Kunz R, et al. Systemic prokinetic pharmacologic treatment for postoperative adynamic ileus following abdominal surgery in adults. Cochrane Database Syst Rev. 2008 Jan 23:(1):CD004930.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD004930.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/18254064?tool=bestpractice.com
While metoclopramide is helpful in treating delayed gastric emptying, it has not proved useful in postoperative ileus when evaluated in randomized controlled trials.[94]Cheape JD, Wexner SD, James K, et al. Does metoclopramide reduce the length of ileus after colorectal surgery? A prospective randomized trial. Dis Colon Rectum. 1991 Jun;34(6):437-41.
http://www.ncbi.nlm.nih.gov/pubmed/2036922?tool=bestpractice.com
[95]Seta ML, Kale-Pradhan PB. Efficacy of metoclopramide in postoperative ileus after exploratory laparotomy. Pharmacotherapy. 2001 Oct;21(10):1181-6.
http://www.ncbi.nlm.nih.gov/pubmed/11601663?tool=bestpractice.com
Intravenous erythromycin has been found not to be beneficial for the treatment of postoperative ileus, and the evidence is insufficient to recommend the use of cholecystokinin-like drugs, cisapride, dopamine agonists, propranolol, or vasopressin.[64]Traut U, Brügger L, Kunz R, et al. Systemic prokinetic pharmacologic treatment for postoperative adynamic ileus following abdominal surgery in adults. Cochrane Database Syst Rev. 2008 Jan 23:(1):CD004930.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD004930.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/18254064?tool=bestpractice.com
[95]Seta ML, Kale-Pradhan PB. Efficacy of metoclopramide in postoperative ileus after exploratory laparotomy. Pharmacotherapy. 2001 Oct;21(10):1181-6.
http://www.ncbi.nlm.nih.gov/pubmed/11601663?tool=bestpractice.com
[96]Lightfoot AJ, Eno M, Kreder KJ, et al. Treatment of postoperative ileus after bowel surgery with low-dose intravenous erythromycin. Urology. 2007 Apr;69(4):611-5.
http://www.ncbi.nlm.nih.gov/pubmed/17445634?tool=bestpractice.com
 [Figure caption and citation for the preceding image starts]: Nasogastric tubeFrom the personal collection of Dr Paula I. Denoya [Citation ends].
[Figure caption and citation for the preceding image starts]: Nasogastric tubeFrom the personal collection of Dr Paula I. Denoya [Citation ends].
