Recommendations
Key Recommendations
Diagnosis is based on the presence of fracture on x-ray, and history is usually specific for a fall or trauma. Magnetic resonance imaging (MRI)/computed tomography (CT) should only be ordered if the index of suspicion of hip fracture is high (i.e., there is groin pain, pain with hip movement, or pain in the region of the groin/proximal femur), but plain x-ray is negative. Laboratory studies are not useful in the diagnosis of fractures. If a hip fracture is identified, referral to an orthopedic surgeon should be made.
History
Hip fractures occur most commonly in older people, and women may be at higher risk than men. The risk of hip fractures increases significantly with age. They occur more frequently in those older than 65 years of age, with the average age being approximately 83 years.[9][32] Osteoporosis is a strong risk factor; there is an almost 3-fold increase in the risk of proximal femoral fractures for both men and women for each decrease of 1 standard deviation below peak bone mass values.[23] A family history of osteoporosis/osteopenia should also be noted.
Patients most commonly have a history of a fall or trauma; it is rare for fractures to occur with no precipitating fall/trauma. High-energy trauma (e.g., motor vehicle accident) is more common in younger patients; however, these account for only 1% to 3% of hip fractures seen.[9][23]
Patients commonly complain of an inability to bear weight, pain in the affected leg/hip, and pain with range of motion of the hip.
Physical exam
Examination is usually nonspecific; however, the leg on the affected side may be shortened and externally rotated if the hip fracture is displaced. This is the only clinical finding indicating that the fracture is displaced. However, this finding may also be seen with other fractures of the femur as well as the pelvis or lower leg.
If the patient can tolerate passive range of motion, pain is elicited in the groin or proximal femur with internal or external rotation of the leg or flexion of the hip. Crepitus may also be felt in the region of the femoral neck with range of motion of the hip.
Radiography
Plain radiographs should be ordered in all patients with a history of a fall or trauma who present with acute hip pain.[51] An anteroposterior (AP) pelvic x-ray and AP and lateral views of the affected hip should be taken.[19][20][51] Radiography will demonstrate a fracture of the proximal femur. A true AP of the hip (an AP image taken with the leg in 15° of internal rotation) may also be helpful.[51] An x-ray of the femur can be ordered if distal extension of the fracture is suspected.
With intracapsular fracture patterns, disruption of the cortex as well as the primary compressive and tensile trabecular lines suggests displacement in the fracture. Increased angulation of varus or valgus on the AP image or increased anterior or posterior version as seen on the lateral radiograph also suggests displacement and can be compared with the other intact hip.
With extracapsular fracture patterns, stability of displaced fractures generally takes into account the extent of comminution and, more specifically, the comminution of the medial cortex. Simple 2-part intertrochanteric fracture patterns with no comminution of the medial calcar (cortex) are generally considered stable. Three- and 4-part intertrochanteric fractures with disruption of the posteromedial cortex or the reverse-obliquity fracture are considered unstable.[3][52][Figure caption and citation for the preceding image starts]: Initial anteroposterior radiograph showing a displaced left hip intracapsular fractureFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends]. [Figure caption and citation for the preceding image starts]: Unstable intertrochanteric fracture on x-rayFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends].
[Figure caption and citation for the preceding image starts]: Unstable intertrochanteric fracture on x-rayFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends].
Other investigations
At least 90% of proximal femoral fractures will be identified on radiographs.[51][53] If the index of suspicion for hip fracture is high and plain x-ray is negative, a CT scan or MRI (without contrast) should be ordered.[51] MRI has been shown to be more cost-effective for the patient, with a higher sensitivity for the detection of occult hip fractures, and is not contingent on time between injury and the study.[51][54][55][56] CT or technetium bone scan may be used if there is no access to an MRI; however, the bone scan may be falsely negative for up to 72 hours from the time of injury.[51] False positives may also arise with bone scan, related to osteoarthritis, soft-tissue injury, or any other process that may increase bone turnover.[51][Figure caption and citation for the preceding image starts]: MRI showing coronal imaging confirming an intracapsular fracture of the left hipFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends].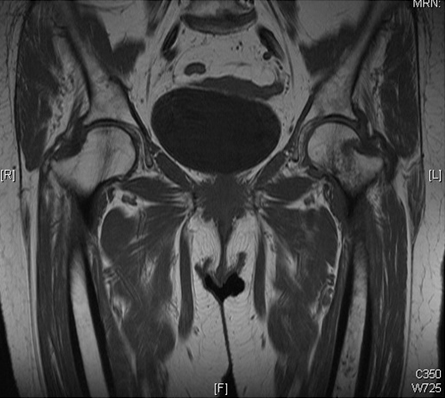 [Figure caption and citation for the preceding image starts]: Anteroposterior pelvic radiograph showing a possible intracapsular fracture of the left hipFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends].
[Figure caption and citation for the preceding image starts]: Anteroposterior pelvic radiograph showing a possible intracapsular fracture of the left hipFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends].
Use of this content is subject to our disclaimer