Approach
The goals of treatment are to:[6]
Provide immediate pain and inflammation relief
Provide eye protection to prevent corneal damage in patients unable to close their eye on the affected side
Minimize the severity of chronic facial palsy.
The majority of patients presenting with Ramsay Hunt syndrome will recover their facial movement at least partially with treatment. Patients typically see improvement in facial movement within a few weeks to months of symptom onset. However, changes in facial symmetry and function can continue for up to a year before a patient’s exam stabilizes. Recurrent Ramsay Hunt syndrome is exceedingly rare.[2]
Management of acute phase
Corticosteroids and antivirals
Give combination therapy with high-dose oral corticosteroids and high-dose antivirals early (i.e., <72 hours from symptom onset) to all patients with Ramsay Hunt syndrome.[1][26][27]
This recommendation is based on the efficacy of corticosteroid treatment shown in studies in patients with Bell's palsy, which is based on reduction of inflammatory edema.[1][26][27] Expert consensus guidelines consider that corticosteroids are still the best treatment option for viral inflammation of the facial nerve; however it is not clear how corticosteroids work on patients with Ramsay Hunt syndrome.[1] The recommendation to use antiviral treatment is based on its demonstrated efficacy in patients with herpes zoster. Antivirals are believed to reduce acute pain, improve herpes zoster lesions, and reduce the risk of postherpetic neuralgia.[28]
Data in patients with Ramsay Hunt syndrome are of low quality and have shown mixed efficacy overall.
One retrospective case review (n=128) of patients with Ramsay Hunt syndrome with complete facial paralysis (House-Brackmann scale VI) showed highest rates of recovery in patients receiving early administration of high-dose corticosteroid and antiviral treatment, compared with normal-dose corticosteroid and antiviral treatment, or with high-dose corticosteroid alone (71%, 60%, and 57%, respectively). However, the results were not statistically significant.[29]
One small study (n=91) evaluating a combination of corticosteroids plus antiviral treatment showed higher rates of good nerve excitability (a promising sign of nerve function) in patients with Ramsay Hunt syndrome receiving combination treatment than in those receiving corticosteroids alone (75% and 53%, respectively).[30]
One Cochrane review found one randomized controlled trial (n=15) comparing intravenous acyclovir and corticosteroids with corticosteroids alone in patients with Ramsay Hunt syndrome and found no statistically significant difference between the two groups.[31]
Despite the lack of randomized prospective studies, collective data from retrospective studies show that patients with Ramsay Hunt syndrome treated with corticosteroids and antivirals have better recovery rates than those receiving no medication.
General warnings and cautions concerning short-course corticosteroids should be followed. Temporary or permanent adverse effects can occur with high doses (e.g., blurry vision, weight gain, Cushingoid appearance, altered glucose metabolism, dyslipidemia, hypertension, cataracts, glaucoma, osteoporosis, diabetes). Monitor patients closely for adverse effects. Consider adding a proton-pump inhibitor for gastric protection when prescribing high-dose corticosteroids.
Assess kidney function in patients on high-dose antiviral therapy. Use caution in patients with renal impairment; a dose adjustment may be necessary.
Eye protection
Keratoconjunctivitis sicca (dry eye) is common and may lead to exposure keratopathy. For patients with facial paralysis and symptomatic eye irritation, give moisture-based therapy (e.g., preservative-free methylcellulose ophthalmic drops) and a lubricant eye ointment. Additionally, advise patients with eye irritation when waking up in the morning to tape the eye shut using non-irritant tape at night after ointment has been applied to prevent corneal damage.[32][33] Eye patches are contraindicated because the eye may easily open under the patch, leading to corneal abrasion.
Surgical decompression
The use of surgical decompression in patients with acute Ramsay Hunt syndrome and complete paralysis who do not show any signs of recovery after treatment is controversial. Neural decompression is rarely employed as there is significant potential morbidity with this procedure. There are limited data supporting surgery over optimal medical management and expectant management.[34][35]
Management of chronic phase
Facial reanimation
Many patients will develop chronic Ramsay Hunt syndrome, despite prompt treatment, with chronic facial paralysis manifested by facial asymmetry, facial tightness, and facial synkinesis (i.e., nonflaccid facial paralysis, postparalytic facial paralysis).[36] Long-term treatment for these patients is individualized and highly specialized. Refer the patient to a specialist in facial reanimation to discuss both surgical and nonsurgical options. Chronic facial paralysis can be a significant source of depression, anxiety, and social withdrawal for patients, and close monitoring is warranted.
Postherpetic neuralgia (defined as pain that persists for >3 months after the cutaneous herpes zoster lesions have resolved) is rare in patients with Ramsay Hunt syndrome. Refer affected patients to a pain specialist.
[Figure caption and citation for the preceding image starts]: Patient with acute Ramsay Hunt syndrome (A and C) that progressed to chronic Ramsay Hunt syndrome (B and D). Photos B and D were taken 14 months after symptom onset. Note the patient’s inability to close right eye (A) and significant smile asymmetry (C), which are both frequently seen in acute Ramsay Hunt syndrome. The patient recovered, but had some signs of aberrant facial nerve regeneration; specifically, note right ocular-oral synkinesis (B) and improved but persistent smile asymmetry (D) From the collection of Dr Matthew Miller; used with permission [Citation ends].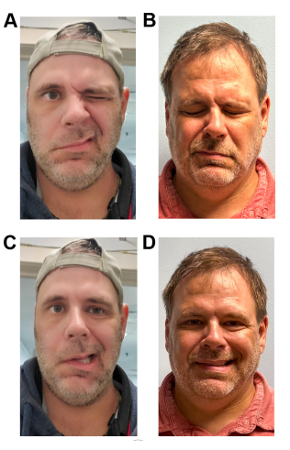
Use of this content is subject to our disclaimer