Postural orthostatic tachycardia syndrome (POTS) is a clinical syndrome characterized by symptoms of orthostatic intolerance and an increase in heart rate (without orthostatic hypotension) on standing, in the absence of other causes. It is also associated with comorbidities such as migraine headaches, irritable bowel syndrome, Ehlers-Danlos syndrome, chronic fatigue syndrome, and autoimmune diseases such as Hashimoto thyroiditis and celiac disease.
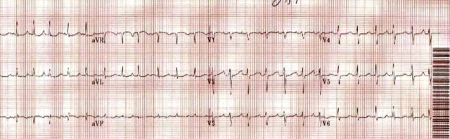
Initial investigations should include an ECG and blood tests to look for other causes of symptoms, such as anemia, hyperthyroidism, and adrenal insufficiency. Further investigation (e.g., Holter monitor, tilt-table test, echocardiogram) may be needed if the diagnosis is unclear, or other causes are suspected.
First-line management of POTS symptoms is avoidance of triggers (e.g., exposure to excessive heat, prolonged standing), and lifestyle modifications (e.g., increase in water and salt intake, use of compression garments). If symptoms of POTS persist, pharmacologic treatment should be started to target specific symptoms; a combination of medications is usually required.
There is a lack of evidence for effective treatments for POTS in children. However, it is reasonable to treat children with the same interventions that are recommended for adults, with a focus on promoting salt and fluid intake, physical counterpressure techniques, and reassurance to the patient and their families.
POTS is a chronic, multisystem disorder that is thought to be due to an autoimmune process. It is characterized by frequent symptoms of orthostatic intolerance that improve rapidly when the patient returns to a supine position, interfere with daily living activities, and have continued for at least 3 months, and an increase in heart rate by ≥30 bpm (or ≥40 bpm in patients ages 12 to 19 years) within 10 minutes of standing from a supine position or head-up tilt (without orthostatic hypotension) that is not due to other causes of sinus tachycardia.[1]Vernino S, Bourne KM, Stiles LE, et al. Postural orthostatic tachycardia syndrome (POTS): state of the science and clinical care from a 2019 National Institutes of Health expert consensus meeting - part 1. Auton Neurosci. 2021 Nov;235:102828.
https://www.doi.org/10.1016/j.autneu.2021.102828
http://www.ncbi.nlm.nih.gov/pubmed/34144933?tool=bestpractice.com
[2]Sheldon RS, Grubb BP 2nd, Olshansky B, et al. 2015 Heart Rhythm Society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm. 2015 Jun;12(6):e41-63.
https://www.doi.org/10.1016/j.hrthm.2015.03.029
http://www.ncbi.nlm.nih.gov/pubmed/25980576?tool=bestpractice.com
[3]Shen WK, Sheldon RS, Benditt DG, et al. 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2017 Aug 1;136(5):e25-e59.
https://www.doi.org/10.1161/CIR.0000000000000498
http://www.ncbi.nlm.nih.gov/pubmed/28280232?tool=bestpractice.com
[4]Raj SR, Guzman JC, Harvey P, et al. Canadian Cardiovascular Society position statement on postural orthostatic tachycardia syndrome (POTS) and related disorders of chronic orthostatic intolerance. Can J Cardiol. 2020 Mar;36(3):357-72.
https://www.doi.org/10.1016/j.cjca.2019.12.024
http://www.ncbi.nlm.nih.gov/pubmed/32145864?tool=bestpractice.com
However, it is undefined in patients ages <12 years, although they may present with similar symptoms.[1]Vernino S, Bourne KM, Stiles LE, et al. Postural orthostatic tachycardia syndrome (POTS): state of the science and clinical care from a 2019 National Institutes of Health expert consensus meeting - part 1. Auton Neurosci. 2021 Nov;235:102828.
https://www.doi.org/10.1016/j.autneu.2021.102828
http://www.ncbi.nlm.nih.gov/pubmed/34144933?tool=bestpractice.com