Approach
AML is a highly heterogeneous disease. The diagnosis of AML requires a multifaceted approach that includes medical history, clinical assessment, and pathologic assessment (including bone marrow and/or peripheral blood).
As AML and acute lymphoblastic leukemia (ALL) are often clinically indistinguishable, confirmation of a myeloid origin of the leukemic cells by immunophenotyping is essential. This may be done on peripheral blood before confirmation from the bone marrow.
History
In all patients, a complete medical history (including family history, if known) is important for diagnosis.
Risk of AML is increased in certain patient groups, including those with a prior history of hematologic disease; previous treatment with chemotherapy; genetic disorders (e.g., inherited chromosomal fragility disorders; bone marrow failure syndromes; chromosomal abnormalities [e.g., trisomy disorders]); age over 65 years; smokers; and prior exposure to radiation or benzene.
The clinical features in the recent history that suggest a diagnosis of AML are related to cytopenia, and include increased fatigue, dizziness, palpitations, fevers, infections, mucosal bleeding (from the gums or nose or menorrhagia in females), gingival enlargement, petechial rash, and bone pain. There may be a history of a skin rash or masses (e.g., skin chloromas). Pulmonary symptoms (e.g., dyspnea) and gastrointestinal symptoms (e.g., severe abdominal pain) due to leukemic infiltration or infection may be present. Neurologic symptoms (e.g., headache, confusion) due to meningeal leukemic infiltration may be present.
Physical examination
Findings may include pallor, ecchymoses, and petechiae. Features of extramedullary leukemic infiltration may be evident (e.g., hepatosplenomegaly, lymphadenopathy, skin and testicular masses). Dental abscess, nasopharyngeal infections, chest signs, or perianal infections may be apparent. Within the skin, leukemia cutis infiltration may be present, and the presence of cutaneous ulcers (e.g., Sweet syndrome or pyoderma gangrenosum) may indicate underlying malignancy. Rarely, an acute abdomen may occur.
Initial laboratory tests
All patients with suspected AML should have the following baseline tests:[23][38]
Complete blood count with differential
Peripheral blood smear
Comprehensive metabolic panel (serum electrolytes, renal and liver profiles, serum uric acid, and serum lactate dehydrogenase [LDH])
Coagulation panel (prothrombin time [PT], activated partial thromboplastin time [aPTT], fibrinogen, and D-dimers).
Laboratory findings
Most patients with AML (including those with acute promyelocytic leukemia [APL], a subtype of AML) have anemia, neutropenia, and/or thrombocytopenia, but blood count can vary greatly.
An elevated white blood cell (WBC) count >100,000/microliter (>100 × 10⁹/L; hyperleukocytosis) occurs in approximately 5% to 20% of patients with AML, predisposing them to complications such as tumor lysis syndrome (TLS), central nervous system (CNS) involvement, and leukostasis (symptomatic hyperleukocytosis; symptoms include respiratory distress and altered mental status).[3][4] These are medical emergencies and require immediate treatment. Despite the elevation in WBC count, many patients have severe neutropenia (<500 granulocytes/microliter [<0.5 × 10⁹ granulocytes/L]), thus placing them at high risk for serious infections.
In AML, the blood film may show myeloid blasts characterized by Auer rods or Phi bodies. In APL, the blood film will typically show hypergranular promyelocytes with bilobed nuclei and bundles of Auer rods (as well as myeloid blasts). A variant of APL is characterized by hypogranular promyelocytes (absence of Auer rods), but is less common.[Figure caption and citation for the preceding image starts]: Peripheral blood film of a patient with acute myeloid leukemia with maturation showing myeloid blasts with an Auer rodFrom the collection of Drs K. Raj and P. Mehta; used with patient consent [Citation ends].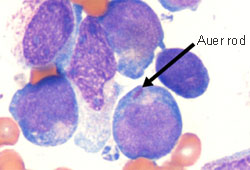 [Figure caption and citation for the preceding image starts]: Peripheral blood film of a patient with acute promyelocytic leukemia showing hypergranular promyelocytes with bilobed nuclei and bundles of Auer rodsFrom the collection of Drs K. Raj and P. Mehta; used with patient consent [Citation ends].
[Figure caption and citation for the preceding image starts]: Peripheral blood film of a patient with acute promyelocytic leukemia showing hypergranular promyelocytes with bilobed nuclei and bundles of Auer rodsFrom the collection of Drs K. Raj and P. Mehta; used with patient consent [Citation ends].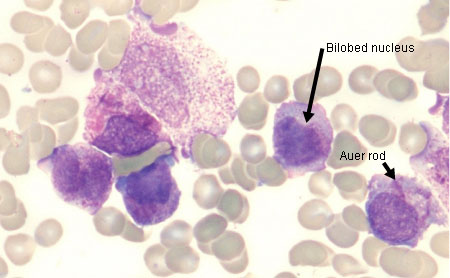 [Figure caption and citation for the preceding image starts]: Peripheral blood film of a patient with acute promyelocytic leukemia showing hypergranular promyelocytes, some with bundles of Auer rodsFrom the collection of Drs K. Raj and P. Mehta; used with patient consent [Citation ends].
[Figure caption and citation for the preceding image starts]: Peripheral blood film of a patient with acute promyelocytic leukemia showing hypergranular promyelocytes, some with bundles of Auer rodsFrom the collection of Drs K. Raj and P. Mehta; used with patient consent [Citation ends].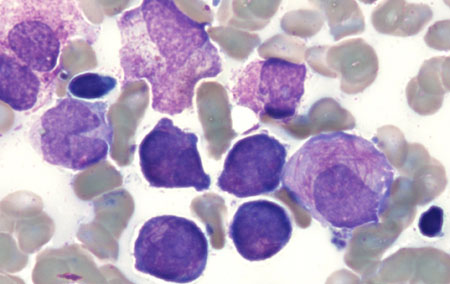
Hyperkalemia, hypocalcemia, hyperphosphatemia, hyperuricemia, and elevated serum LDH may occur due to TLS, particularly during treatment and if WBC count (tumor burden) is high. This can lead to cardiac arrhythmias, seizures, acute renal failure, and death, if untreated. TLS is an oncologic emergency.[51] See Tumor lysis syndrome.
Hypercalcemia may occur due to bony infiltration or ectopic release of a parathyroid hormone-like substance.
The coagulation tests PT and aPTT may be mildly prolonged with normal fibrinogen and D-dimer. If these tests are abnormal (prolonged PT and aPTT, decreased fibrinogen, and/or elevated D-dimer), disseminated intravascular coagulation (DIC) should be suspected and an urgent referral is warranted to commence treatment. Refer to the International Society on Thrombosis and Haemostasis (ISTH) scoring system for DIC.[52] DIC occurs most frequently in APL.
Bone marrow evaluation
The diagnostic workup includes bone marrow aspirate and trephine biopsy analyses. The following tests should be performed.[23][38]
Cytomorphology assessment: demonstrates bone marrow hypercellularity and infiltration by myeloid blasts (as well as hypergranular or hypogranular [less common] promyelocytes, in APL). Blast cells are negative for terminal deoxynucleotidyl transferase (TdT) and stain positive for myeloperoxidase.
Immunophenotyping (using flow cytometry on bone marrow aspirate): identifies cell surface and cytoplasmic markers of myeloid blasts (e.g., CD34, CD33) and establishes lineage.
Immunohistochemistry (using core biopsy specimen): may be used instead of flow cytometry for immunophenotyping if bone marrow aspirate is unavailable or of poor quality.
If bone marrow specimens are inadequate or unattainable, then peripheral blood can be used for pathologic assessment provided there are sufficient numbers of circulating blasts.
Genetic testing
Cytogenetic analysis (karyotyping and fluorescence in situ hybridization [FISH]) and molecular genetic testing should be performed to inform the diagnosis, prognosis, and treatment.[23][38]
In AML, the following genetic abnormalities should be investigated due to their association with specific prognoses and treatment targets: RUNX1::RUNX1T1; CBFB::MYH11; MLLT3::KMT2A (or other KMT2A rearrangements); DEK::NUP214; BCR::ABL1; KAT6A::CREBBP; c-KIT; NPM1; FLT3 (ITD and TKD); IDH1; IDH2; CEBPA (basic leucine zipper [bZIP] domain); -5 or del(5q); -7; -17/abn(17p); GATA2; MECOM(EVI1); ASXL1; BCOR; EZH2; RUNX1; SF3B1; SRSF2; STAG2; U2AF1; ZRSR2; and TP53.[23][38] See Criteria.
Next-generation sequencing panels and multiplex gene panels are recommended for mutational analysis.[23]
APL is characterized by the PML::RARA fusion gene caused by a t(15;17)(q22;q12) balanced chromosomal rearrangement.[23][37]
Definitive diagnosis and classification
AML can be diagnosed and classified according to the latest World Health Organization (WHO) classification (5th Edition, 2022) or the International Consensus Classification (ICC).[1][2] In both classifications, bone marrow evaluation, genetic testing, and predisposing factors (e.g., prior therapy; antecedent myeloid neoplasms; inherited genetic mutations or syndrome) are required to make a definitive AML diagnosis. However, the classifications differ in how specific subtypes of AML are categorized, and in the blast count threshold requirements for certain subtypes of AML.
The 5th edition of the WHO Classification of Haematolymphoid Tumours no longer requires a blast count threshold of ≥20% for the diagnosis of AML with defining genetic abnormalities (except for BCR::ABL1 fusion and CEBPA mutation).[1] In the ICC classification, however, a blast count of ≥10% is required for diagnosing AML with defining genetic abnormalities (except for BCR::ABL1 fusion where a blast count of ≥20% is required).[2]
See Classification section for further details.
Additional tests
Human leukocyte antigen (HLA) typing should be performed in all patients being considered for an allogeneic stem cell transplant.
CNS imaging (e.g., brain MRI or CT scan) should be carried out in patients presenting with neurologic signs or symptoms suggesting CNS involvement.[23][38] A diagnostic lumbar puncture should be carried out if CNS imaging does not identify CNS bleeding, meningeal disease, and a mass lesion, and neurologic signs and symptoms persist. A single dose of intrathecal chemotherapy (e.g., methotrexate or cytarabine) may be considered at the time of diagnostic lumbar puncture. Coagulopathy should be managed before lumbar puncture, particularly in patients with APL.
An FDG-PET/CT scan should be considered in patients with suspected extramedullary disease.[38]
Cardiac function assessment (echocardiogram or multigated acquisition scan) should be performed in patients:
with a history or symptoms of cardiac disease,
with prior exposure to cardiotoxic drugs or radiation therapy to the thorax, or
Findings may guide treatment.
Chest x-ray may be performed to identify pneumonia, mediastinal masses, pulmonary infiltrates, or cardiomegaly.
Use of this content is subject to our disclaimer