Approach
Presumptive diagnosis of squamous cell carcinoma (SCC) of the skin is usually based on a thorough history and clinical findings; however, skin biopsy confirms the diagnosis.[73]
Patients with SCC of the skin often present with multiple actinic keratoses (AK). These are skin-colored, yellowish, or erythematous, ill-defined, irregularly shaped, small, scaly macules or plaques localized to sun-exposed areas of the body that have the potential to progress into SCC. Vigilance and a low threshold for investigation are important in achieving early diagnosis and a successful outcome.
History
SCCs are most frequently observed in photoexposed skin, often in those >40 years of age, and frequently in the presence of actinic keratoses. Changes in shape or size, increased redness, induration, inflammation, or bleeding of any such lesion should prompt investigation of a potential SCC.
Although not diagnostic, AKs tend to be multiple whereas SCCs tend to be solitary. In immunocompromised patients, however, multiple SCCs are not uncommon. Men have a higher incidence than women, and those with Fitzpatrick skin type I and II (white) are at increased risk.[8][9][10]
Skin phototype and cumulative UV radiation exposure history (e.g., sun exposure, tanning beds, psoralen, and UV-A light therapy for psoriasis) should be noted.[38][39] Inquire about rarer risk factors, including exposure to ionizing radiation, arsenic, soot, or tar; human papillomavirus; immunosuppression; previous melanoma; and hereditary skin conditions.[4][22][46][47][50][53][54][55][56][57][58]
Because AKs and SCCs are on a spectrum, it is often difficult to clinically distinguish between the two. In general, SCCs tend to be symptomatic and are thicker, larger, more indurated than AKs.
The rate of transformation of actinic keratoses to invasive SCC is not completely clear, although estimates range from 0.025% to 16% per lesion per year.[51] However, the vast majority of SCCs arise within or close to actinic keratoses. There is evidence to suggest that patients with Olsen grade 3 actinic keratosis are at the highest risk of developing invasive SCC.[52]
Bowen disease (SCC in situ) may be misdiagnosed as dermatitis that fails to respond to treatment.
Patients commonly present with a new or enlarging lesion that they are concerned about, which may be tender or itchy, or a nonhealing wound originally caused by some trauma.
Physical exam
A thorough skin exam should be performed, including dermoscopy. Good lighting and possibly handheld lenses should be used. Recognition of different types of SCC is essential, as the therapy and follow-up will vary.
SCC in situ (Bowen disease)
In situ tumors (Bowen disease) present as thin, flesh-colored or erythematous plaques that often have scale or hemorrhagic crust.[Figure caption and citation for the preceding image starts]: Squamous cell in situ on nasal bridgeFrom the private collection of Dr Nwaneshiudu and Dr Soltani [Citation ends]. Most commonly detected on head and neck (84%) and extensor upper extremities (13%).[39] May be friable and bleed easily and are located mostly on sun-exposed skin.[Figure caption and citation for the preceding image starts]: Squamous cell carcinoma on the dorsal hand with evidence of extensive sun damageFrom the private collection of Dr Nwaneshiudu and Dr Soltani [Citation ends].
Most commonly detected on head and neck (84%) and extensor upper extremities (13%).[39] May be friable and bleed easily and are located mostly on sun-exposed skin.[Figure caption and citation for the preceding image starts]: Squamous cell carcinoma on the dorsal hand with evidence of extensive sun damageFrom the private collection of Dr Nwaneshiudu and Dr Soltani [Citation ends].
Invasive SCC
Invasive SCC may present as exophytic and sometimes ulcerated tumors. For example, verrucous carcinoma presents as exophytic, fungating, verrucous nodules, or plaques on skin or mucosa. Despite low mitotic activity and slow growth, verrucous carcinoma can infiltrate adjacent tissues in advanced stages but does not metastasize.
Keratoacanthoma presents as a rapidly growing, dome-shaped nodule with a central keratin-filled crater, occasionally they can act aggressively and invade surrounding tissue
Metastatic SCC
In metastatic disease, regional lymph nodes are involved in approximately 85% of cases, and approximately 15% of cases involve distant sites, including the lungs, liver, brain, skin, and bone. Lymphadenopathy, bone pain, or hepatomegaly may be seen with metastatic disease.
Marjolin ulcers present in an area of previously traumatized, chronically inflamed or scarred skin, or a nonhealing wound. Case series suggest that these ulcers are often found in an advanced state, with a propensity for lymph node metastasis and distant metastasis.[74]
Patients with perineural involvement may present with neurologic signs. Tumors with perineural involvement, when present on the face, can invade sinuses via a foramen.
Biopsy
To confirm the diagnosis, a biopsy must be performed.[73]
A shave biopsy, punch biopsy, incisional biopsy, or excisional biopsy may be used, depending on the size and location of the tumor. Histologic analysis of skin specimens routinely uses hematoxylin and eosin. The histologic appearance depends on the type of SCC but usually shows keratinocyte atypia. The biopsy specimen should include the underlying dermis to confirm or rule out invasion.
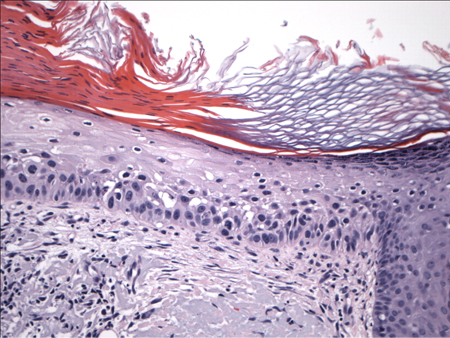
Actinic keratosis:
Displays atypical keratinocytes that appear to crowd the basal layer and lower levels of the epidermis, but do not extend to full thickness.[Figure caption and citation for the preceding image starts]: Biopsy showing histology of an actinic keratosis with keratinocyte atypia limited to the basal layerFrom the private collection of Dr Nwaneshiudu and Dr Soltani [Citation ends].
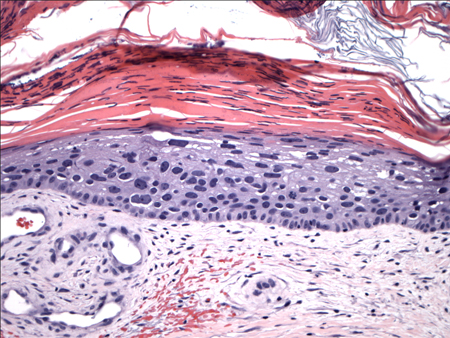
SCC in situ (Bowen disease):
Displays full-thickness atypia that is confined to the epidermis, with an intact basement membrane. The involvement of the entire thickness of the epidermis follows, and there is an absent granular layer, as well as parakeratosis.[Figure caption and citation for the preceding image starts]: Biopsy showing histology of an in-situ SCC with full-thickness keratinocyte atypiaFrom the private collection of Dr Nwaneshiudu and Dr Soltani [Citation ends].
Invasive tumors:
Extend beyond the basement membrane, penetrate into the dermis, and may invade deeper structures. Atypical keratinocytes have variable large, hyperchromatic nuclei, and mitotic figures are noted. There are variable degrees of differentiation, and highly aggressive, undifferentiated SCCs may present as spindle cell tumors. Solar elastosis is usually noted in the superficial dermis, reflecting the extent of chronic UV exposure.[Figure caption and citation for the preceding image starts]: Biopsy histology showing invasive SCC with keratinocyte atypia involving all layers of the epidermis and islands budding into the dermisFrom the private collection of Dr Nwaneshiudu and Dr Soltani [Citation ends].
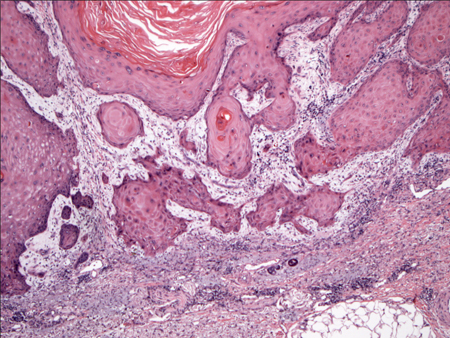 [Figure caption and citation for the preceding image starts]: Biopsy showing histology of an invasive SCC with keratinocyte atypia involving all layers of the epidermis and islands budding into the dermis. Higher magnification (left) highlights the cellular atypiaFrom the private collection of Dr Nwaneshiudu and Dr Soltani [Citation ends].
[Figure caption and citation for the preceding image starts]: Biopsy showing histology of an invasive SCC with keratinocyte atypia involving all layers of the epidermis and islands budding into the dermis. Higher magnification (left) highlights the cellular atypiaFrom the private collection of Dr Nwaneshiudu and Dr Soltani [Citation ends].
Keratoacanthomas:
Appear as endophytic nodules with a central invagination, replete with keratin. Atypia is minimal and mitoses are rare. Lymphocytic infiltrate is present at the margins of the lesion.
Marjolin ulcer:
Shares similar histopathologic features as invasive SCCs but may be more aggressive.
Verrucous carcinoma:
Appears as a well-differentiated neoplasm with warty features such as acanthosis, hyperkeratosis, and hypergranulosis.
Other investigations
For high-risk SCC (i.e., larger and more invasive lesions with risk of perineural invasion or lymphadenopathy) a computed tomography (CT), magnetic resonance imaging (MRI), or fluorine-18-fluorodeoxyglucose (FDG)-PET/CT scan may be ordered to evaluate the extent of the large tumors and/or to rule out metastatic disease.[73] Some evidence suggests that MRI is best for the detection of perineural spread, and CT is the more accurate modality to detect bony invasion and nodal metastasis.[75]
In patients at risk of metastases, CBC with differential and LFTs may be used to assist early detection of distant metastases.
Use of this content is subject to our disclaimer