Clinical evaluation
The typical patient is between 20 to 34 years of age.[13]National Cancer Institute. Cancer stat facts: testicular cancer. 2024 [internet publication].
https://seer.cancer.gov/statfacts/html/testis.html
He may report nonspecific testicular discomfort and the feeling of a mass in the testis. Symptom onset is usually more than 2 weeks but patients may present with painful swelling of sudden onset (due to associated hemorrhage or infection) in 10% of cases.[41]Dogra V, Bhatt S. Acute painful scrotum. Radiol Clin North Am. 2004 Mar;42(2):349-63.
http://www.ncbi.nlm.nih.gov/pubmed/15136021?tool=bestpractice.com
Examination of the testis is essential for detecting this condition early. Genital exam is a relatively quick and simple clinical assessment, and should be carried out when a male patient presents with genital symptoms.[42]Marcell AV, Bell DL, Joffe A; Society for Adolescent Health and Medicine, SAHM Male Health Special Interest Group. The male genital examination: a position paper of the Society for Adolescent Health and Medicine. J Adolesc Health. 2012 Apr;50(4):424-5.
http://www.ncbi.nlm.nih.gov/pubmed/22443851?tool=bestpractice.com
The exam should first be performed with the patient standing to assess asymmetry of a low-riding testis. The location of the mass can be palpated by gently rolling the testicle between thumb and fingers. The mass should be firmly attached to the testis (intratesticular) on the side or the lower pole of the testis. Special attention should be given to the shape and consistency of the mass. The mass is usually smooth, firm, and nonfluctuating. However, on occasions it presents as an uneven distortion of the contour of the testis or as homogeneous enlargement. Palpation of the spermatic cord for thickness and mobility, and presence of inguinal swelling should be noted. If there is any doubt, an ultrasound of the testis is mandatory. A urologist should evaluate every testicular mass.
A full systemic exam should be performed, as around 5% to 10% of patients have extratesticular manifestations at the time of presentation with or without apparent primary tumor in the testes.[43]Richie JP. Neoplasms of the testis. In: Walsh PC, Retik AB, Vaughan ED, et al., eds. Campell's urology. 7th ed. Philadelphia, PA: WB Saunders Company; 2001:2417-8.
Investigations
Ultrasound of the testis is the preferred initial imaging modality and has high sensitivity for testicular malignancy.[2]Stephenson A, Bass EB, Bixler BR, et al. Diagnosis and treatment of early-stage testicular cancer: AUA guideline amendment 2023. J Urol. 2024 Jan;211(1):20-5.
https://www.auajournals.org/doi/10.1097/JU.0000000000003694
http://www.ncbi.nlm.nih.gov/pubmed/37707243?tool=bestpractice.com
[44]American College of Radiology. ACR appropriateness criteria: newly diagnosed palpable scrotal abnormality. 2021 [internet publication].
https://acsearch.acr.org/docs/3158184/Narrative
[45]European Association of Urology. Testicular cancer. 2024 [internet publication].
https://uroweb.org/guideline/testicular-cancer
[Figure caption and citation for the preceding image starts]: Ultrasonographic picture of testicular mass as hypoechoic lesionBMJ Case Reports 2011; doi:10.1136/bcr.12.2010.3565 [Citation ends]. However, a negative ultrasound does not exclude the presence of cancer and should be repeated in 6 to 8 weeks in patients with indeterminate findings on ultrasound or physical exam and normal serum tumor markers.[2]Stephenson A, Bass EB, Bixler BR, et al. Diagnosis and treatment of early-stage testicular cancer: AUA guideline amendment 2023. J Urol. 2024 Jan;211(1):20-5.
https://www.auajournals.org/doi/10.1097/JU.0000000000003694
http://www.ncbi.nlm.nih.gov/pubmed/37707243?tool=bestpractice.com
Ultrasound should be carried out with color Doppler assessment to confirm the presence of a testicular mass before orchiectomy.[46]Oldenburg J, Berney DM, Bokemeyer C, et al. Testicular seminoma and non-seminoma: ESMO-EURACAN clinical practice guideline for diagnosis, treatment and follow-up. Ann Oncol. 2022 Apr;33(4):362-75.
https://www.annalsofoncology.org/article/S0923-7534(22)00007-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35065204?tool=bestpractice.com
Use of color Doppler can help to distinguish tumors from other scrotal swellings (e.g., varicocele).[47]Sohaib SA, Cook G, Koh DM. Imaging studies for germ cell tumors. Hematol Oncol Clin North Am. 2011 Jun;25(3):487-502, vii.
http://www.ncbi.nlm.nih.gov/pubmed/21570604?tool=bestpractice.com
The contralateral testis should also be evaluated for the presence of synchronous tumors and microcalcifications, and to measure the testicular volume.[46]Oldenburg J, Berney DM, Bokemeyer C, et al. Testicular seminoma and non-seminoma: ESMO-EURACAN clinical practice guideline for diagnosis, treatment and follow-up. Ann Oncol. 2022 Apr;33(4):362-75.
https://www.annalsofoncology.org/article/S0923-7534(22)00007-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35065204?tool=bestpractice.com
Biopsy of the contralateral testis may be indicated if a suspicious mass is identified, the testis is atrophied, or there is a history of cryptorchidism. It is not recommended for testicular microcalcifications alone.[45]European Association of Urology. Testicular cancer. 2024 [internet publication].
https://uroweb.org/guideline/testicular-cancer
[48]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: testicular cancer [internet publication].
https://www.nccn.org/professionals/physician_gls/default.aspx
[49]Pfail J, Santiago I, Jang TL, et al. Contralateral testicular biopsy in men with testicular cancer. Eur Urol Focus. 2024 May;10(3):370-2.
https://www.eu-focus.europeanurology.com/article/S2405-4569(24)00095-6/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/39095219?tool=bestpractice.com
Clusters of microcalcifications may be associated with increased risk of testicular cancer in the presence of other risk factors, although the clinical significance of this remains controversial.[50]'t Hoen LA, Bhatt NR, Radmayr C, et al. The prognostic value of testicular microlithiasis as an incidental finding for the risk of testicular malignancy in children and the adult population: a systematic review. On behalf of the EAU pediatric urology guidelines panel. J Pediatr Urol. 2021 Dec;17(6):815-31.
https://www.jpurol.com/article/S1477-5131(21)00313-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/34217588?tool=bestpractice.com
However, a negative ultrasound does not exclude the presence of cancer and should be repeated in 6 to 8 weeks in patients with indeterminate findings on ultrasound or physical exam and normal serum tumor markers.[2]Stephenson A, Bass EB, Bixler BR, et al. Diagnosis and treatment of early-stage testicular cancer: AUA guideline amendment 2023. J Urol. 2024 Jan;211(1):20-5.
https://www.auajournals.org/doi/10.1097/JU.0000000000003694
http://www.ncbi.nlm.nih.gov/pubmed/37707243?tool=bestpractice.com
Ultrasound should be carried out with color Doppler assessment to confirm the presence of a testicular mass before orchiectomy.[46]Oldenburg J, Berney DM, Bokemeyer C, et al. Testicular seminoma and non-seminoma: ESMO-EURACAN clinical practice guideline for diagnosis, treatment and follow-up. Ann Oncol. 2022 Apr;33(4):362-75.
https://www.annalsofoncology.org/article/S0923-7534(22)00007-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35065204?tool=bestpractice.com
Use of color Doppler can help to distinguish tumors from other scrotal swellings (e.g., varicocele).[47]Sohaib SA, Cook G, Koh DM. Imaging studies for germ cell tumors. Hematol Oncol Clin North Am. 2011 Jun;25(3):487-502, vii.
http://www.ncbi.nlm.nih.gov/pubmed/21570604?tool=bestpractice.com
The contralateral testis should also be evaluated for the presence of synchronous tumors and microcalcifications, and to measure the testicular volume.[46]Oldenburg J, Berney DM, Bokemeyer C, et al. Testicular seminoma and non-seminoma: ESMO-EURACAN clinical practice guideline for diagnosis, treatment and follow-up. Ann Oncol. 2022 Apr;33(4):362-75.
https://www.annalsofoncology.org/article/S0923-7534(22)00007-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35065204?tool=bestpractice.com
Biopsy of the contralateral testis may be indicated if a suspicious mass is identified, the testis is atrophied, or there is a history of cryptorchidism. It is not recommended for testicular microcalcifications alone.[45]European Association of Urology. Testicular cancer. 2024 [internet publication].
https://uroweb.org/guideline/testicular-cancer
[48]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: testicular cancer [internet publication].
https://www.nccn.org/professionals/physician_gls/default.aspx
[49]Pfail J, Santiago I, Jang TL, et al. Contralateral testicular biopsy in men with testicular cancer. Eur Urol Focus. 2024 May;10(3):370-2.
https://www.eu-focus.europeanurology.com/article/S2405-4569(24)00095-6/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/39095219?tool=bestpractice.com
Clusters of microcalcifications may be associated with increased risk of testicular cancer in the presence of other risk factors, although the clinical significance of this remains controversial.[50]'t Hoen LA, Bhatt NR, Radmayr C, et al. The prognostic value of testicular microlithiasis as an incidental finding for the risk of testicular malignancy in children and the adult population: a systematic review. On behalf of the EAU pediatric urology guidelines panel. J Pediatr Urol. 2021 Dec;17(6):815-31.
https://www.jpurol.com/article/S1477-5131(21)00313-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/34217588?tool=bestpractice.com
Computed tomography (CT) scan of the pelvis and abdomen with contrast is used to assess the stage of cancer spread.[2]Stephenson A, Bass EB, Bixler BR, et al. Diagnosis and treatment of early-stage testicular cancer: AUA guideline amendment 2023. J Urol. 2024 Jan;211(1):20-5.
https://www.auajournals.org/doi/10.1097/JU.0000000000003694
http://www.ncbi.nlm.nih.gov/pubmed/37707243?tool=bestpractice.com
[48]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: testicular cancer [internet publication].
https://www.nccn.org/professionals/physician_gls/default.aspx
[51]American College of Radiology. ACR appropriateness criteria: staging and surveillance of testicular cancer. 2021 [internet publication].
https://acsearch.acr.org/docs/69375/Narrative
Magnetic resonance imaging (MRI) may be useful as an alternative modality, if CT is inconclusive or the contrast media is contraindicated due to patient allergy or renal insufficiency.[2]Stephenson A, Bass EB, Bixler BR, et al. Diagnosis and treatment of early-stage testicular cancer: AUA guideline amendment 2023. J Urol. 2024 Jan;211(1):20-5.
https://www.auajournals.org/doi/10.1097/JU.0000000000003694
http://www.ncbi.nlm.nih.gov/pubmed/37707243?tool=bestpractice.com
Chest imaging is mandatory to assess for the presence of lung metastases.[2]Stephenson A, Bass EB, Bixler BR, et al. Diagnosis and treatment of early-stage testicular cancer: AUA guideline amendment 2023. J Urol. 2024 Jan;211(1):20-5.
https://www.auajournals.org/doi/10.1097/JU.0000000000003694
http://www.ncbi.nlm.nih.gov/pubmed/37707243?tool=bestpractice.com
[51]American College of Radiology. ACR appropriateness criteria: staging and surveillance of testicular cancer. 2021 [internet publication].
https://acsearch.acr.org/docs/69375/Narrative
Chest x-ray is advised as first-line chest imaging for clinical stage I seminoma only. CT chest is recommended as first-line for other tumor types, or those with rising postorchiectomy serum tumor markers, or with evidence of metastases on abdominal/pelvic imaging, chest x-ray or physical exam.[2]Stephenson A, Bass EB, Bixler BR, et al. Diagnosis and treatment of early-stage testicular cancer: AUA guideline amendment 2023. J Urol. 2024 Jan;211(1):20-5.
https://www.auajournals.org/doi/10.1097/JU.0000000000003694
http://www.ncbi.nlm.nih.gov/pubmed/37707243?tool=bestpractice.com
CT-positron emission tomography (PET) scanning has not been shown to be superior to CT alone and is not recommended for staging.[2]Stephenson A, Bass EB, Bixler BR, et al. Diagnosis and treatment of early-stage testicular cancer: AUA guideline amendment 2023. J Urol. 2024 Jan;211(1):20-5.
https://www.auajournals.org/doi/10.1097/JU.0000000000003694
http://www.ncbi.nlm.nih.gov/pubmed/37707243?tool=bestpractice.com
Serum tumor markers should be obtained before and after orchiectomy, with staging based on postorchiectomy nadir values.[2]Stephenson A, Bass EB, Bixler BR, et al. Diagnosis and treatment of early-stage testicular cancer: AUA guideline amendment 2023. J Urol. 2024 Jan;211(1):20-5.
https://www.auajournals.org/doi/10.1097/JU.0000000000003694
http://www.ncbi.nlm.nih.gov/pubmed/37707243?tool=bestpractice.com
[48]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: testicular cancer [internet publication].
https://www.nccn.org/professionals/physician_gls/default.aspx
The combination of elevated beta-human chorionic gonadotropin (beta-hCG), alpha-fetoprotein (AFP), and lactate dehydrogenase (LDH) is diagnostic of the disease. AFP can be elevated by embryonal carcinoma, teratoma, yolk sac tumors, or mixed tumors. Pure choriocarcinomas and seminomas are not associated with elevated AFP levels. If histology shows pure seminoma but serum AFP is elevated without other identifiable cause, the tumor should be reclassified and treated as nonseminomatous. Seminomas may present with modest elevations of beta-hCG due to the presence of syncytiotrophoblasts in the tumor. LDH is raised in 40% to 60% of all patients with seminoma or nonseminomatous germ cell tumors.[52]Sturgeon CM, Duffy MJ, Stenman UH, et al. National Academy of Clinical Biochemistry laboratory medicine practice guidelines for use of tumor markers in testicular, prostate, colorectal, breast, and ovarian cancers. Clin Chem. 2008 Dec;54(12):e11-79.
http://www.clinchem.org/cgi/content/full/54/12/e11
http://www.ncbi.nlm.nih.gov/pubmed/19042984?tool=bestpractice.com
In 10% of persistent or recurrent nonseminomas, LDH is the sole elevated marker.[53]Milose JC, Filson CP, Weizer AZ, et al. Role of biochemical markers in testicular cancer: diagnosis, staging, and surveillance. Open Access J Urol. 2011 Dec 30;4:1-8.
https://www.dovepress.com/getfile.php?fileID=11732
http://www.ncbi.nlm.nih.gov/pubmed/24198649?tool=bestpractice.com
However, it has a high false-positive rate and should be used mainly to assess tumor burden. Approximately 80% of nonseminomatous tumors have elevated serum markers. Both AFP and beta-hCG are increased in 44% of cases, AFP alone is elevated in 26% of cases, and beta-hCG alone is elevated in 9% of cases.[52]Sturgeon CM, Duffy MJ, Stenman UH, et al. National Academy of Clinical Biochemistry laboratory medicine practice guidelines for use of tumor markers in testicular, prostate, colorectal, breast, and ovarian cancers. Clin Chem. 2008 Dec;54(12):e11-79.
http://www.clinchem.org/cgi/content/full/54/12/e11
http://www.ncbi.nlm.nih.gov/pubmed/19042984?tool=bestpractice.com
Placental alkaline phosphatase is elevated in up to 40% of cases with advanced disease.[52]Sturgeon CM, Duffy MJ, Stenman UH, et al. National Academy of Clinical Biochemistry laboratory medicine practice guidelines for use of tumor markers in testicular, prostate, colorectal, breast, and ovarian cancers. Clin Chem. 2008 Dec;54(12):e11-79.
http://www.clinchem.org/cgi/content/full/54/12/e11
http://www.ncbi.nlm.nih.gov/pubmed/19042984?tool=bestpractice.com
However, placental alkaline phosphatase is not used in routine clinical practice and should be limited to experimental or clinical trial settings. Serum microRNA-371a-3p (M371) has emerged as a potential biomarker for both seminomatous and nonseminomatous germ cell tumors, with improved sensitivity and specificity compared to conventional tumor markers.[54]Dieckmann KP, Radtke A, Geczi L, et al. Serum levels of microRNA-371a-3p (M371 Test) as a new biomarker of testicular germ cell tumors: results of a prospective multicentric study. J Clin Oncol. 2019 Jun 1;37(16):1412-23.
https://ascopubs.org/doi/10.1200/JCO.18.01480
http://www.ncbi.nlm.nih.gov/pubmed/30875280?tool=bestpractice.com
Further prospective studies are needed to guide implementation of M371 into routine clinical practice.[55]Nestler T, Schoch J, Belge G, et al. MicroRNA-371a-3p-the novel serum biomarker in testicular germ cell tumors. Cancers (Basel). 2023 Aug 3;15(15):3944.
https://www.mdpi.com/2072-6694/15/15/3944
http://www.ncbi.nlm.nih.gov/pubmed/37568759?tool=bestpractice.com
The diagnosis of testicular cancer is generally established by removing and examining the involved testicle (orchiectomy) after obtaining serum tumor markers.
[Figure caption and citation for the preceding image starts]: Metastatic seminoma. Left image: H&E stain low power. Right image placental alkaline phosphatase (PLAP) stain high power. The H&E image shows nests of malignant cells with clear cytoplasm; the tumour cells are strongly positive for PLAP confirming the diagnosisLaw C et al. BMJ Case Rep. 2020 Apr 22;13(4):e233368. doi: 10.1136/bcr-2019-233368; used with permission [Citation ends].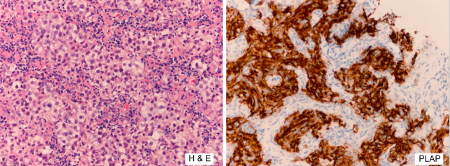 [Figure caption and citation for the preceding image starts]: NonseminomaFrom the collection of Dr Francisco G. La Rosa; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: NonseminomaFrom the collection of Dr Francisco G. La Rosa; used with permission [Citation ends].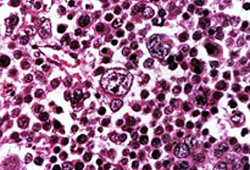 At all stages of disease, orchiectomy is essential.[2]Stephenson A, Bass EB, Bixler BR, et al. Diagnosis and treatment of early-stage testicular cancer: AUA guideline amendment 2023. J Urol. 2024 Jan;211(1):20-5.
https://www.auajournals.org/doi/10.1097/JU.0000000000003694
http://www.ncbi.nlm.nih.gov/pubmed/37707243?tool=bestpractice.com
Radical inguinal orchiectomy should be performed early in the evaluation of a suspicious testicular mass. In early-stage disease, an orchiectomy is often curative.
At all stages of disease, orchiectomy is essential.[2]Stephenson A, Bass EB, Bixler BR, et al. Diagnosis and treatment of early-stage testicular cancer: AUA guideline amendment 2023. J Urol. 2024 Jan;211(1):20-5.
https://www.auajournals.org/doi/10.1097/JU.0000000000003694
http://www.ncbi.nlm.nih.gov/pubmed/37707243?tool=bestpractice.com
Radical inguinal orchiectomy should be performed early in the evaluation of a suspicious testicular mass. In early-stage disease, an orchiectomy is often curative.
 However, a negative ultrasound does not exclude the presence of cancer and should be repeated in 6 to 8 weeks in patients with indeterminate findings on ultrasound or physical exam and normal serum tumor markers.[2] Ultrasound should be carried out with color Doppler assessment to confirm the presence of a testicular mass before orchiectomy.[46] Use of color Doppler can help to distinguish tumors from other scrotal swellings (e.g., varicocele).[47] The contralateral testis should also be evaluated for the presence of synchronous tumors and microcalcifications, and to measure the testicular volume.[46] Biopsy of the contralateral testis may be indicated if a suspicious mass is identified, the testis is atrophied, or there is a history of cryptorchidism. It is not recommended for testicular microcalcifications alone.[45][48][49] Clusters of microcalcifications may be associated with increased risk of testicular cancer in the presence of other risk factors, although the clinical significance of this remains controversial.[50]
However, a negative ultrasound does not exclude the presence of cancer and should be repeated in 6 to 8 weeks in patients with indeterminate findings on ultrasound or physical exam and normal serum tumor markers.[2] Ultrasound should be carried out with color Doppler assessment to confirm the presence of a testicular mass before orchiectomy.[46] Use of color Doppler can help to distinguish tumors from other scrotal swellings (e.g., varicocele).[47] The contralateral testis should also be evaluated for the presence of synchronous tumors and microcalcifications, and to measure the testicular volume.[46] Biopsy of the contralateral testis may be indicated if a suspicious mass is identified, the testis is atrophied, or there is a history of cryptorchidism. It is not recommended for testicular microcalcifications alone.[45][48][49] Clusters of microcalcifications may be associated with increased risk of testicular cancer in the presence of other risk factors, although the clinical significance of this remains controversial.[50]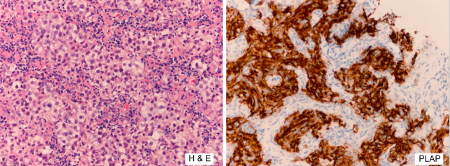 [Figure caption and citation for the preceding image starts]: NonseminomaFrom the collection of Dr Francisco G. La Rosa; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: NonseminomaFrom the collection of Dr Francisco G. La Rosa; used with permission [Citation ends].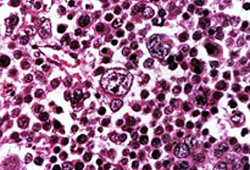 At all stages of disease, orchiectomy is essential.[2] Radical inguinal orchiectomy should be performed early in the evaluation of a suspicious testicular mass. In early-stage disease, an orchiectomy is often curative.
At all stages of disease, orchiectomy is essential.[2] Radical inguinal orchiectomy should be performed early in the evaluation of a suspicious testicular mass. In early-stage disease, an orchiectomy is often curative.