Etiology
Various spinal structures including ligaments, facet joints, paravertebral musculature and fascia, intervertebral disks, and spinal nerve roots have been implicated as pain generators.[6]
The etiologies can be subdivided into 3 groups: mechanical, systemic, and referred. By far, the most common cause is mechanical (97%).[6] Most low back pain is nonspecific and the precise cause cannot be identified.[2]
Mechanical
Mechanical back pain is defined as pain that is elicited with spinal motion and decreases with rest.
Lumbar strain/sprain
Strain: disruption of the muscle fibers at various locations within the muscle belly or musculotendinous junction. Patients experience intense pain for 24 to 48 hours then experience muscle spasm.
Sprain: subcatastrophic stretch of ≥1 spinal ligaments. Some fibers are injured but the overall continuity of the ligament is maintained.
Degenerative disk and/or facets
The disk is presumed to be the primary source of pain (discogenic).[13]
Many patients have asymptomatic degenerative disks.
Discogenic pain increases with flexion, sitting, and coughing/sneezing due to an increase in intradiscal pressures.
Facet joints may cause back pain that increases with extension as the facet joints are mechanically loaded.[14]
The facet capsule has been demonstrated anatomically to contain nociceptive fibers.[15][16]
Herniated nucleus pulposus
Natural history is of clinical improvement in most patients with only 10% requiring surgical intervention.[17][18]
Leg pain is usually greater than back pain with pain radiating into the lower extremity in a dermatomal distribution.
Back pain may occur as a result of referred pain from a corresponding tear in the annulus fibrosus.[Figure caption and citation for the preceding image starts]: Herniated nucleus pulposus causing nerve root impingement. Radicular symptoms may result from chemical mediators released by degenerative disks or mechanical compression of the nerve rootBMJ 2008;337:a2718; used with permission [Citation ends].

Spinal stenosis
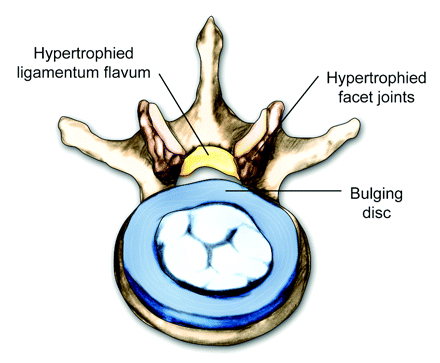
A narrowing of the anatomic dimensions of the spinal canal secondary to disk osteophyte formation and facet joint/ligamentum flavum hypertrophy.[Figure caption and citation for the preceding image starts]: Axial view of a vertebral body showing central spinal stenosisBMJ 2008;337:a2718; used with permission [Citation ends].
Patients may manifest back pain that is often referred to as neurogenic secondary to mechanical constriction of the lumbar nerve roots.[19][Figure caption and citation for the preceding image starts]: Magnetic resonance imaging of spinal stenosis: (A) demarcates the normal sagittal diameter of the spinal canal. (B) demarcates severe narrowing of the spinal canalCourtesy of Dr K. Singh; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Magnetic resonance imaging of spinal stenosis: arrow points to the moderately stenotic spinal canal caused by hypertrophic facets and ligament flavumCourtesy of Dr K. Singh; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Magnetic resonance imaging of spinal stenosis: arrow points to the moderately stenotic spinal canal caused by hypertrophic facets and ligament flavumCourtesy of Dr K. Singh; used with permission [Citation ends].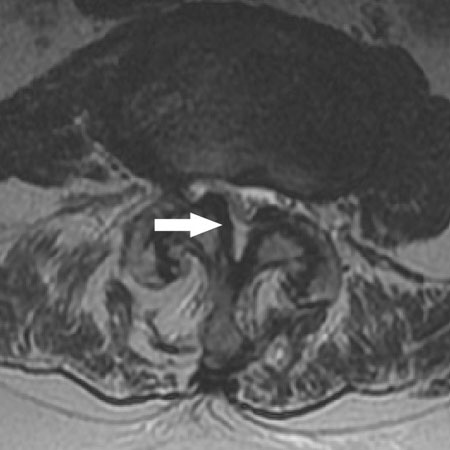
Spondylolysis and/or spondylolisthesis
General population has a pars interarticularis defect incidence of 3% to 6%,[20][21][22] but most are asymptomatic.
Patients have pain in the lower back with occasional radiation to the posterior thigh. Pain is aggravated by extension.
If spondylolisthesis is severe, an exaggerated lordosis, heart-shaped buttock, or midline step off of the spinous processes may be present.
Compression fracture
May occur without recognized trauma and patients should have a medical workup performed for the evaluation of osteoporosis, osteomalacia, and malignancy, depending on the fracture mechanism.
Patients may report sudden onset back pain after coughing, sneezing, lifting or changing position.
May be associated with a radiculopathy secondary to neuroforaminal encroachment from vertebral body height loss.
If a compression fracture occurs through a low-energy mechanism one should find metabolic reasons for the fracture, and osteoporosis should be aggressively treated to prevent further fractures.[Figure caption and citation for the preceding image starts]: Radiograph of a compression fracture: a lateral radiograph of an L2 compression fracture (A). Wedging of the vertebral body is seenCourtesy of Dr K. Singh; used with permission [Citation ends].

Sacroiliitis
The sacroiliac joint has been implicated in low back pain.[23] There may also be associated referred lower extremity pain.
The primary cause of sacroiliitis is usually degenerative, although it may be associated with inflammatory arthritis. It is common as a degenerative problem in middle to old age, but is uncommon as a secondary inflammatory problem.
Sacroiliitis is estimated to occur in 10% to 25% of patients with persistent axial low back pain without disk herniation, discogenic pain, or radiculitis.[24]
Scoliosis
Systemic
Systemic etiologies are much less common (1%) than mechanical back pain, but these causes usually warrant further workup and signal possible urgent referral to a spine surgeon.[6][27]
Tumor and infection are the more common causes of systemic etiologies of back pain.
The term "inflammatory spondyloarthropathy" incorporates several inflammatory conditions with similar features (mostly axial spondyloarthritis including ankylosing spondylitis, or psoriatic arthritis). Axial and peripheral joints can be affected.
Systemic etiologies include:
Infection
Untreated discitis, osteomyelitis, or epidural abscess can lead to sepsis, progressive kyphotic deformity, and/or neurologic deficit.
Malignancy (primary or secondary)
A benign or a malignant spinal tumor can present with back pain with radicular symptoms.
May be suspected when nocturnal pain and weight loss occurs, particularly if lower back pain does not improve after 6 weeks of conservative treatment.
May be a history of a primary malignancy known to metastasize to bone, such as breast, lung, prostate, kidney, or thyroid. Others tumors that may spread to the spine include multiple myeloma, lymphoma, and melanoma.[Figure caption and citation for the preceding image starts]: Radiograph of tumor: lymphoma (A) destroying the L5 vertebraCourtesy of Dr K. Singh; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Magnetic resonance imaging of lymphoma: arrowhead indicates a soft-tissue mass protruding into the spinal canal. Arrow points to the tumor protruding anterior to the L5 vertebral bodyCourtesy of Dr K. Singh; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Magnetic resonance imaging of lymphoma: arrowhead indicates a soft-tissue mass protruding into the spinal canal. Arrow points to the tumor protruding anterior to the L5 vertebral bodyCourtesy of Dr K. Singh; used with permission [Citation ends].
Inflammatory spondyloarthropathy (e.g., ankylosing spondylitis, psoriatic arthritis, enteropathic arthritis)[28]
Connective tissue disorder (e.g. systemic lupus erythematosus, rheumatoid arthritis).
Referred
Sources are typically nonspine related and include intra/retroperitoneal pathologies. These etiologies are much less common (2%) than mechanical back pain.[6]
Aortic aneurysm
Acute pancreatitis
Acute pyelonephritis
Renal colic
Peptic ulcer disease
Herpes zoster (shingles).
Use of this content is subject to our disclaimer