Etiology
At the time of initial infection, it is thought that a small number of Mycobacterium tuberculosis organisms are contained in various body organs. The development of active TB requires infection by M tuberculosis and inadequate containment by the immune system. Active TB disease may occur from reactivation of previously latent infection or from progression of primary infection.[13] EPTB in immunocompetent adults usually results from reactivation of TB. In children and adults with HIV infection, EPTB may result from recent infection (primary disease). TB enteritis, often seen in the ileocecal region, can also result from ingestion of infected sputum or dairy products.[14] Disseminated TB is due to the hematogenous dissemination of M tuberculosis throughout the body.
Pathophysiology
Infection with Mycobacterium tuberculosis requires inhalation of aerosolized particles called droplet nuclei. In the course of primary infection, a period of subclinical bacillemia usually occurs and a small number of M tuberculosis organisms are contained in various body organs. Exposure may be followed by clearance, persistent latent infection, or progression to primary disease.
Successful containment of TB is dependent on the cellular immune system, mediated primarily through T-helper cells (TH1 response). T cells and macrophages form a granuloma with a center that contains necrotic material (caseous center) and M tuberculosis, and peripheral granulation tissue consisting primarily of macrophages and lymphocytes. The granuloma serves to prevent further growth and spread of M tuberculosis. These individuals are not infectious and have latent TB infection; the majority of these patients will have a normal chest x-ray and positive tuberculin skin test and positive interferon-gamma release assays.
Pleural TB (particularly primary disease) may occur from a few mycobacteria gaining access to the pleural space with a resultant T-cell response and delayed hypersensitivity reaction. The effusion is due to increased capillary permeability and decreased lymphatic drainage. As TB pleural effusion results from intensive inflammatory response, recovery of M tuberculosis from the pleural fluid occurs in about 40% of cases.
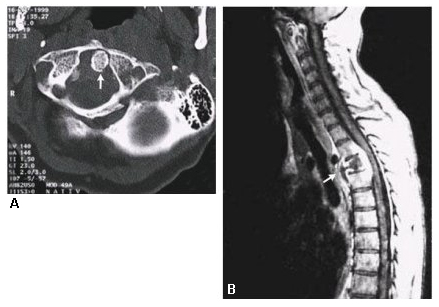
Skeletal TB is an osteomyelitis that starts in the growth plates of bones where the blood supply is the richest and from there spreads into joint spaces. Vertebral disease usually starts in the subchondral cancellous bone, from where it spreads to the cortex and on to the disk. Bone destruction is more extensive on the ventral aspect leading to anterior wedging. Paraspinous collections may also develop.[15] Spinal or vertebral TB has been known historically as Pott disease.
TB meningitis results from hematogenous spread of M tuberculosis with the development of submeningeal or intrameningeal foci called Rich foci. With rupture of a Rich focus into the subarachnoid space, meningitis develops. This may result from reactivation (more common in adults) or primary infection (more common in children). BCG vaccination is about 64% effective against TB meningitis in young children.[16] In a population in Vietnam, a polymorphism in leukotriene A4 hydrolase, which regulates the balance of pro- and anti-inflammatory eicosanoids, was associated with protection against TB meningitis, improved survival, and response to corticosteroid therapy.[17][18]
Abdominal TB includes disease of the intestines, peritoneum, and mesenteric lymph nodes. In peritoneal TB, the peritoneum becomes studded with tubercles. As protein-rich fluid is exuded, ascites accumulate.
More than 90% of patients with peritoneal TB will have ascites; the remainder generally have more advanced disease and present with fibroadhesions (“doughy abdomen”). TB enteritis may occur secondary to ingestion of infected sputum or initial hematogenous spread. If the enteric source spreads to the mesenteric lymph nodes, they may rupture into the peritoneum. TB enteritis occurs most frequently in the ileocecal region. Its appearance may be ulcerative or hypertrophic.[14]
Pericardial TB results from contiguous spread from adjacent mediastinal lymph nodes, or progression of a primary or latent focus within the pericardium. Some patients present with signs of cardiac constriction without an acute phase of pericarditis being noticed.
Disseminated TB refers to simultaneous involvement of multiple organ sites that may occur with primary infection (particularly in immunocompromised individuals) or with reactivation. Disseminated TB is sometimes called miliary TB; its lesions are yellowish granulomas 1 to 2 mm in diameter that resemble millet seeds on chest x-ray. It is due to hematogenous spread of M tuberculosis.
Classification
Extrapulmonary TB categorized by affected organ system
Acquisition of Mycobacterium tuberculosis is followed by systemic dissemination and immunologic containment in the majority of cases. As such, progression to TB disease can take place in various areas of the body:
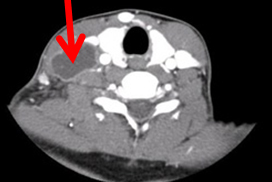
Lymphatic TB: most commonly found in the cervical or supraclavicular regions, and often seen in Asian and black women from TB-endemic areas.[1][Figure caption and citation for the preceding image starts]: CT showing necrotic cervical lymph nodeFrom the collection of Dr David J. Horne and Dr Masahiro Narita; used with permission [Citation ends].
Pleural TB: at least 40% of pleural TB is the result of primary TB (occurring shortly after acquisition of tubercle bacilli), rather than due to reactivation of latent foci (post-primary TB).[2][3] In this regard it differs from other sites of EPTB.
Skeletal TB: results from hematogenous spread. The most common sites of involvement are the vertebral column (especially the lower thoracic and lumbar regions), hip, and knee. TB involving the spine is also known as Pott disease. TB in the joints is usually monoarticular. [Figure caption and citation for the preceding image starts]: CT showing spinal TB (Pott disease)Massachusetts Medical Society; reproduced with permission from N Engl J Med. 2002;347:1849; used with permission [Citation ends].
Central nervous system TB: includes meningitis and tuberculomas, with meningitis being the most common presentation. TB meningitis typically involves the base of the brain. Meningeal TB is a devastating form of EPTB and early treatment is important to prevent irreversible deficits or death.
Peritoneal TB: arises from reactivation of M tuberculosis foci established in the peritoneum from hematogenous spread or may occur in disseminated TB. Risk factors include cirrhosis, peritoneal dialysis, and diabetes mellitus.
Genitourinary TB: may involve either the urinary or genital tract or both. Symptoms include dysuria, hematuria, and urinary frequency. Genital TB is a common cause of infertility in endemic settings.
Pericardial TB: the common findings are related to pericardial fluid (e.g., cardiac tamponade) or pericardial fibrosis (e.g., constriction).
Disseminated TB: due to the hematogenous dissemination of M tuberculosis throughout the body with involvement of multiple organs. When a characteristic chest radiograph pattern (diffuse, bilateral, symmetrical, discrete, 1-2 mm opacities) is present, this condition is also known as miliary TB.
Use of this content is subject to our disclaimer