Approach
The presentation of hypoparathyroidism is usually by clinical or laboratory manifestations of hypocalcemia. Hypocalcemia (low ionized serum calcium or total serum calcium adjusted for albumin) in the presence of an undetectable, low, or inappropriately normal intact parathyroid hormone (PTH) on two occasions at least 2 weeks apart confirms the diagnosis.[1]
As most cases of hypoparathyroidism are postsurgical, hypocalcemia is usually detected on regular follow-up screening blood tests. Patients with hypoparathyroidism are assessed for any signs or symptoms of hypocalcemia, concomitant conditions, and medications that could be altering calcium, magnesium, and PTH homeostasis, with special focus on prior neck surgery and inherited conditions.
If the presenting symptoms are severe and life-threatening, such as intractable tetany, laryngospasm, bronchospasm/wheezing, dyspnea, altered mentation, seizures, cardiac failure, or tachycardia, therapy should be immediate; treat with intravenous calcium infusion with close cardiac monitoring, clinical symptom monitoring, and repeated laboratory testing.[27]
Recent neck surgery
In individuals who have had recent thyroid or parathyroid surgery, serum calcium levels are checked during the postoperative period (often within 6 hours of surgery) and on the morning of discharge. At discharge, the patient and the family must be instructed carefully about the symptoms of hypocalcemia and prescribed a supply of calcium (with or without calcitriol) supplements for administration after surgery.
For parathyroid operations, in many centers, intraoperative PTH levels are measured at scheduled intervals during surgery to monitor the successful resection of the overactive parathyroid gland(s). Close follow-up is needed after discharge for possible transient or permanent hypoparathyroidism, depending on the extent of surgery performed (i.e., the number of glands explored and the number of abnormal glands removed).
For thyroid operations in which subtotal or total thyroidectomy, with or without lymph node dissection, has been performed, approaches vary. However, many endocrine surgeons will obtain an intraoperative PTH level at the end of the case, or in the recovery room, and rely on this level as a guide.
After laryngeal surgery, albumin-corrected serum total calcium levels must be checked at regular intervals postoperatively and symptoms of hypocalcemia closely monitored. As the in-hospital recovery time is longer (vs. thyroidectomy or parathyroidectomy), a stable regimen of calcium replacement can be attained and symptoms well controlled prior to discharge.
Manifestations of hypocalcemia
Symptoms of hypocalcemia fluctuate such that patients presenting with a new diagnosis of hypoparathyroidism, as well as those with chronic hypoparathyroidism, may become acutely symptomatic.
Severe hypocalcemia can cause:
Muscle twitching or spasm, muscle cramps, abdominal cramps
Laryngospasm, stridor, wheezing
Periorbital numbness, tingling, intermittent or persistent paresthesias
Prolonged QT interval on ECG, irregular heart beat, tachyarrhythmias, hypotension
Lethargy, confusion, disorientation
Seizures, coma.
Mild and longstanding hypocalcemia can cause:
Perioral, distal hand and foot paresthesias
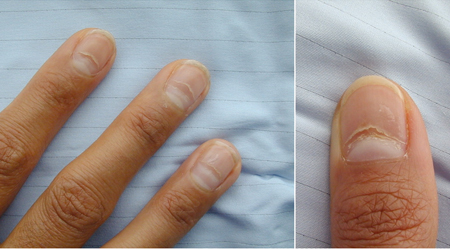
Brittle nails or nail dystrophy, dry hair
Dyspnea, irregular heartbeat, tachycardia
Fatigue
Poor memory/slowed thinking
Cataracts
Nephrocalcinosis, renal stones.[Figure caption and citation for the preceding image starts]: ECG demonstrating an atrial arrhythmia most likely to be atrial fibrillation in a patient with hypoparathyroidism and hypocalcemiaAdapted from Nijjer S, Ghosh AK, Dubrey SW. Hypocalcaemia, long QT interval and atrial arrhythmias. BMJ Case Reports 2010 [doi:10.1136/bcr.08.2009.2216]. Copyright © 2011 by the BMJ Publishing Group Ltd. [Citation ends].

Physical examination findings of severe hypocalcemia may include:
Spontaneous and sometimes painful involuntary muscle contractions, tetany
Positive Trousseau sign (painful clasping response of fingers and hands when blood pressure cuff is inflated above systolic blood pressure) Trousseau's sign: video clip Opens in new window
Positive Chvostek sign (ipsilateral contraction of facial muscles when facial nerve is tapped in front of the ear). Chvostek's sign: a video demonstration Opens in new window
If severe signs and/or symptoms are present, urgent testing includes:
Serum total calcium and albumin or serum ionized calcium. (If a normal serum calcium is found despite symptoms of hypocalcemia, an arterial blood gas for carbon dioxide can be performed to determine whether hyperventilation is present.)
Electrolyte panel (serum sodium, potassium, chloride, and bicarbonate).
Assessment of serum magnesium and phosphate, plasma intact PTH (second- or third-generation assay), renal function (serum creatinine).
ECG.[Figure caption and citation for the preceding image starts]: Nail dystrophy due to hypocalcemiaNijjer S, Ghosh AK, Dubrey SW. Hypocalcaemia, long QT interval and atrial arrhythmias. BMJ Case Reports 2010 [doi:10.1136/bcr.08.2009.2216]. Copyright © 2011 by the BMJ Publishing Group Ltd. [Citation ends].
Albumin-corrected serum total calcium is calculated as follows:
Corrected calcium (mg/dL) = 0.8 x (normal albumin [g/dL] - patient's albumin [g/dL]) + measured serum calcium [mg/dL]
Or using SI units:
Corrected calcium (mmol/L) = 0.02 x (normal albumin [g/L] - patient's albumin [g/L]) + measured serum calcium (mmol/L)
These formulae provide only an approximation, which may not be accurate in acutely ill patients, in whom obtaining the serum ionized calcium concentration is recommended to guide management.[28] [Figure caption and citation for the preceding image starts]: ECG demonstrating an atrial arrhythmia most likely to be atrial fibrillation in a patient with hypoparathyroidism and hypocalcemiaAdapted from Nijjer S, Ghosh AK, Dubrey SW. Hypocalcaemia, long QT interval and atrial arrhythmias. BMJ Case Reports 2010 [doi:10.1136/bcr.08.2009.2216]. Copyright © 2011 by the BMJ Publishing Group Ltd. [Citation ends].
Diagnosis of etiology
Hypomagnesemia and hypermagnesemia are both functional states of hypoparathyroidism.[14][15][16] In patients with hypomagnesemia, the low plasma PTH levels are readily reversed by magnesium repletion. Several risk factors, such as proton-pump inhibitor therapy, can contribute to chronic hypomagnesemia, and a large number of genetic disorders of magnesium metabolism can cause it.[14][15][16] Chronic alcoholism, malnutrition, diarrhea, and malabsorption can produce hypomagnesemia.[16][17]
Additional laboratory tests suggested for all non-postsurgical cases include:
Complete blood count
Iron studies and ferritin
Urinary calcium and creatinine
Vitamin D metabolites (25-hydroxyvitamin D and 1,25-dihydroxyvitamin D)
Liver function tests (if elevated without other explanation, then copper levels).
Presence of at least one major feature (mucocutaneous candidiasis, hypoparathyroidism, or adrenal insufficiency) and positive antibodies to type 1 interferon suggest autoimmune polyendocrine syndrome type 1 (APS1). Molecular diagnosis constitutes the presence of autoimmune regulator gene (AIRE) pathogenic variants.[1]
Specific genetic testing can also be considered in patients who:[1]
have a positive family history of nonsurgical hypoparathyroidism
present with syndromic features
are younger than 40 years.
Use of this content is subject to our disclaimer