Urgent considerations
See Differentials for more details
Easy bruising may be a sign of a life-threatening decrease in platelet count or factor levels. Early recognition of the cause may prevent severe bleeding complications. The following diagnoses may be life-threatening.
Thrombotic thrombocytopenic purpura (TTP)
Classically characterized by a pentad of symptoms:
microangiopathic hemolytic anemia
thrombocytopenia
acute renal insufficiency
neurologic abnormalities;
fever.
However, the presence of microangiopathic hemolytic anemia and thrombocytopenia alone is sufficient to consider starting treatment as this condition has a mortality rate of >90% without treatment.[18] Clinicians should maintain a high index of suspicion and initiate appropriate treatment promptly. The standard first-line therapy is plasmapheresis. Corticosteroids and other immunosuppressants are commonly used because most cases are thought to be related to autoimmune phenomena.[18]
Acquired coagulation inhibitors
Patients frequently have life-threatening bleeding and impressive bruising upon diagnosis. Diagnosis is made with a factor assay, Bethesda assay (for factor inhibitor), and von Willebrand factor (vWF) assay. Treatments for factor VIII inhibitors include bypassing agents and immunosuppression, while treatments for vWF inhibitors include vWF concentrates, intravenous immune globulin (IVIG), and immunosuppression if indicated.[16][19][20][21] [Figure caption and citation for the preceding image starts]: Large bruise on the abdomen of a patient on warfarin with acquired factor V inhibitorBMJ Case Reports; doi:10.1136/bcr-2013-010018. Copyright © 2014 by the BMJ Publishing Group Ltd [Citation ends].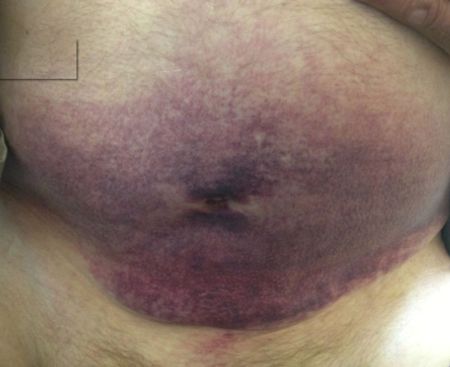
Disseminated intravascular coagulation (DIC)
Characterized by excess thrombin generation with depletion of clotting factors leading to abnormal bleeding, small vessel thrombosis, and tissue ischemia. The patient may also develop microangiopathic hemolytic anemia and thrombocytopenia. Treatment is directed at determining and managing the underlying disorder (e.g., sepsis, malignancy, drugs). Coagulation factor and fibrinogen replacement should be given to patients with coagulopathy who have bleeding or require surgery.
Immune thrombocytopenia (ITP)
Patients often present with severe thrombocytopenia and sudden onset of petechiae and mucosal bleeding. Severe thrombocytopenia can be associated with life-threatening bleeding such as intracranial bleeding. The standard first-line therapy is a corticosteroid with or without IVIG.[22][23][24] When corticosteroids are contraindicated, either Rho (D) immune globulin or IVIG is recommended.[24] If ITP is refractory, treatment options include splenectomy, rituximab, and thrombopoietin receptor agonists (e.g., eltrombopag, romiplostim).[25][26][27] Rho (D) immune globulin may be used in Rh-positive patients.
Leukemia and lymphoma
Patients with acute leukemia often present with pancytopenia and bleeding or bruising as a consequence of severe thrombocytopenia. Patients with aggressive lymphoma involving the bone marrow can also present with thrombocytopenia and bruising. Lymphadenopathy and B symptoms (e.g., fever, night sweats, weight loss) are other common presenting symptoms of lymphoma. The mortality rate of acute leukemia is 100% without proper treatment. Bone marrow biopsy is recommended to achieve definitive diagnosis and to determine the prognosis. Treatment is chemotherapy, which may need to be followed by stem cell transplantation depending on the type and prognosis.
Myelodysplastic syndrome
Most commonly presents in older patients (>65 years) with signs and symptoms of anemia, leukopenia, and/or thrombocytopenia; however, can be found during routine laboratory investigations in asymptomatic patients. Bone marrow biopsy is needed for definitive diagnosis and to rule out other life-threatening conditions such as acute myelogenous leukemia. Supportive therapy is the mainstay of treatment in many patients; however, chemotherapy or stem cell transplant may be used in selected patients. Stem cell transplant is the only potentially curative therapy. May progress to acute myelogenous leukemia in some patients.
Aplastic anemia
Patients most commonly present with signs and symptoms of anemia, leukopenia, and/or thrombocytopenia. Bone marrow biopsy is needed for definitive diagnosis and to rule out other life-threatening conditions such as acute myelogenous leukemia. The main treatment modalities include withdrawal of any potential etiologic agent, immunosuppressive therapy and/or eltrombopag, supportive therapies, and allogeneic stem cell transplantation.
Drug-induced thrombocytopenia
Common causative drugs include chemotherapy, anticonvulsants, nonsteroidal anti-inflammatory drugs (NSAIDs), and antibiotics. Discontinuation of the causative drug is crucial.
Hemolytic uremic syndrome (HUS)
HUS is sometimes difficult to differentiate from TTP because their clinical presentations can be very similar. ADAMTS13 levels are commonly used to help differentiate these two entities. Typical HUS secondary to Escherichia coli infection should be treated with supportive care only. Adequate hydration is important to minimize renal damage. Avoidance of antibiotics, antimotility agents, and NSAIDs is advised. Cautious use of opioids is also advised; there are insufficient data on the effect of opioids on the course of HUS. Anemia can be treated with red cell transfusion. Platelet transfusions are generally avoided in the absence of active bleeding.
Atypical HUS (which is not associated with bloody diarrhea) requires additional treatments, such as the monoclonal antibody eculizumab, or plasma exchange.
Coagulation factor deficiencies
Patients present with recurrent or severe bleeding and bruising. Hemophilia is an X-linked, inherited disease, so it is most commonly seen in males; however, females can be symptomatic carriers.[14] Severe type I or type III von Willebrand disease (vWD) is associated with vWF and factor VIII deficiencies, and can present with the same symptoms.[28] Bleeding can be life-threatening and bruising can be significant, especially with trauma or surgeries, if the disease is unrecognized and treatment is not started. Standard treatment is to administer appropriate factor concentrates. Desmopressin may be used in patients with vWD or mild hemophilia who have previously undergone a desmopressin challenge.
Use of this content is subject to our disclaimer