Differentials
Common
Purpura simplex
History
female sex (more common), no history of trauma or abnormal bleeding
Exam
ecchymosis (varying size, stage, and location) typically on exposed areas such as extremities (not trunk, back, nor face), no active bleeding or large hematoma
1st investigation
- CBC:
normal
- prothrombin time/activated partial thromboplastin time:
normal
More
Other investigations
Actinic purpura (also known as senile purpura)
History
older age, bilateral bruising on extensor surfaces of forearms, no history of abnormal bleeding or systemic illness
Exam
ecchymosis seen on exposed extremities (varying number, size, and stage), no other significant findings
1st investigation
- CBC:
normal
- prothrombin time/activated partial thromboplastin time:
normal
More
Other investigations
Medications
History
use of anticoagulants (especially high doses), antiplatelet agents, nonsteroidal anti-inflammatory drugs, corticosteroids, antidepressants; history of epistaxis
Exam
ecchymosis at injection site (e.g., with parenteral anticoagulants); signs of hemarthrosis or gastrointestinal bleeding
1st investigation
- INR/activated partial thromboplastin time (aPTT):
elevated INR (warfarin); prolonged aPTT (heparin)
- anti-Xa level:
>1.0
More
Other investigations
- CBC:
possible anemia
- serum creatinine:
may be high
More
Alcohol use disorder
History
heavy alcohol use
Exam
signs of cirrhosis or liver impairment (e.g., jaundice, ascites, splenomegaly) with long-term use, alcohol odor on breath with acute intoxication
1st investigation
- blood alcohol level:
may be elevated at time of test
- LFTs:
abnormal
- prothrombin time/activated partial thromboplastin time:
prolonged
More
Other investigations
Drug-induced thrombocytopenia
History
history of taking causative drug (e.g., chemotherapy, anticonvulsants, nonsteroidal anti-inflammatory drugs, antibiotics), mucosal bleeding
Exam
petechiae
1st investigation
- CBC:
thrombocytopenia
- withdrawal of causative drug:
resolution of symptoms
Other investigations
Platelet storage pool disease
History
abnormal bleeding with procedures, epistaxis, menorrhagia
Exam
ecchymosis may be seen
1st investigation
- CBC:
normal
- platelet electron microscopy:
decreased delta or alpha granules in platelets
More
Other investigations
- platelet aggregation test:
normal or nonspecific abnormality
More - platelet function analyzer (PFA-100):
normal or prolonged
- prothrombin time/activated partial thromboplastin time:
normal
von Willebrand disease (vWD)
History
positive family history, abnormal bleeding with procedures, menorrhagia, epistaxis, postpartum hemorrhage, mucosal bleeding
Exam
ecchymosis is usually the only finding
1st investigation
Other investigations
- vWF multimer analysis:
type 1: all multimers present, decreased in intensity; type 2A, loss of medium and high molecular weight multimers; type 2B, loss of high molecular weight multimers; type 2M, normal multimers
Vitamin K deficiency
History
hospitalization, prolonged intravenous antibiotics, malnutrition
Exam
may see bruises of various sizes and stages, possible cachexia
1st investigation
- prothrombin time:
prolonged; normal after mixing study
Other investigations
- factor (II, VII, IX, X) assay:
low
Cirrhosis
History
may be asymptomatic or nonspecific symptoms (e.g., anorexia, weight loss, fatigue), bleeding, hepatitis infection, heavy alcohol use, autoimmune disease
Exam
jaundice, spider angiomas, esophageal or gastric varices (could be associated with hemorrhage), abdominal distension, confusion
1st investigation
- CBC:
variable
- LFTs:
normal or elevated aspartate aminotransferase, alanine aminotransferase, and alkaline phosphatase
- prothrombin time/activated partial thromboplastin time:
prolonged
- serum albumin:
decreased
Other investigations
- ultrasound/CT/MRI abdominal:
liver surface nodularity, evidence of ascites or splenomegaly
- liver biopsy:
fibrotic changes
Vasculitis
History
arthralgia, myalgia, malaise, vision changes, abdominal pain, cutaneous ulcers, hematuria, hemoptysis, wheeze, sinus pain, ear pain, headache (temporal arteritis), chest pain (angina and/or myocardial infarction)
Exam
palpable purpura (patient may mistake for bruising), bruits, asymmetric brachial pulses
1st investigation
- erythrocyte sedimentation rate (ESR):
>100 mm/hour
More - CRP:
elevated
- antineutrophil cytoplasmic autoantibodies:
positive
- serum creatinine:
normal or elevated
- urinalysis:
hematuria, proteinuria, red blood cell casts
- biopsy of affected tissue:
vessel wall necrosis, fibrinoid necrosis, karyorrhexis (fragmentation of the nucleus and the break up of the chromatin into unstructured granules), and red blood cell extravasation
Other investigations
Uncommon
Hereditary hemorrhagic telangiectasia (HHT)
History
positive family history, recurrent epistaxis; fatigue, pica, nail changes, hair loss (symptoms of iron-deficiency anemia)
Exam
mucocutaneous telangiectasia, visceral arteriovenous malformations
1st investigation
- clinical diagnosis:
diagnosis is made based on history and examination
Other investigations
Cushing syndrome
History
chronic/excessive corticosteroid use or source of endogenous cortisol (e.g., overproduction of adrenocorticotropic hormone [ACTH] by the pituitary in Cushing disease; overproduction of cortisol by an adrenal tumor)
Exam
acne, hirsutism, thinning skin, abdominal striae, facial plethora (red discoloration), proximal myopathy, central obesity, hypertension
1st investigation
- 24-hour urinary free cortisol and/or late-night salivary cortisol:
elevated
- low-dose (1 mg) overnight dexamethasone suppression test:
serum cortisol >1.8 micrograms/dL
Other investigations
- morning plasma ACTH:
>20 picograms/mL indicates pituitary or ectopic etiology; <5 picograms/mL indicates adrenal etiology
More - pituitary MRI:
may show pituitary adenoma
- adrenal CT:
may show adrenal mass
Child abuse
History
recurrent injuries, unstable home environment, inconsistent/changing history, unexplained/inconsistent injuries
Exam
multiple ecchymosis found on any part(s) of the body, other signs of physical abuse (e.g., burn marks, bone fractures, head injuries, retinal hemorrhage)
1st investigation
- x-ray/CT area of injury:
may show bone fracture or intracranial bleeding
Other investigations
Elder abuse
History
recurrent injuries, unstable home environment, inconsistent/changing history, unexplained/inconsistent injuries
Exam
multiple ecchymosis found on any part(s) of the body, other signs of physical abuse (e.g., burn marks, bone fractures, head injuries)
1st investigation
- x-ray/CT area of injury:
may show bone fracture or intracranial bleeding
Other investigations
Immune thrombocytopenia (ITP)
History
also known as idiopathic thrombocytopenic purpura; hepatitis C, HIV, sudden onset of petechiae, mucosal bleeding, absence of systemic symptoms (or symptoms of malignancy), absence of medications that cause thrombocytopenia
Exam
petechiae and/or ecchymosis on extremities
1st investigation
- CBC:
thrombocytopenia
Thrombotic thrombocytopenic purpura (TTP)
History
altered mental status, sensation changes, headache, gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea)
Exam
petechiae, purpura, and/or ecchymosis on extremities; abnormal neurological examination (e.g., focal weakness, seizures, altered mental status), fever
1st investigation
- CBC:
thrombocytopenia, anemia
- peripheral blood smear:
microangiopathic blood film with schistocytes
- LDH:
elevated
- serum bilirubin:
elevated
- haptoglobin:
low
- ADAMTS-13 antigen level:
decreased (often <5%)
Hemolytic uremic syndrome (HUS)
History
common in children, bloody diarrhea (typical HUS); altered mental status, sensation changes, headache (atypical HUS); presentation similar to thrombotic thrombocytopenic purpura (TTP)
Exam
petechiae, purpura, and/or ecchymosis on extremities; abnormal neurological examination (e.g., focal weakness, seizures, altered mental status)
1st investigation
- CBC:
thrombocytopenia, anemia
- peripheral blood smear:
microangiopathic blood film with schistocytes
- serum creatinine level:
elevated
- ADAMTS-13 antigen level:
usually normal (may be slightly low)
More - LDH:
elevated
- haptoglobin:
low
Other investigations
Disseminated intravascular coagulation
History
presence of underlying disorder (e.g., malignancy, sepsis, organ failure, obstetric disorders or complications)
Exam
excessive bleeding or oozing from mucosal areas or intravenous sites, ischemic tissue damage (e.g., ischemic digits)
1st investigation
- CBC:
thrombocytopenia, anemia
- prothrombin time/activated partial thromboplastin time:
prolonged
- fibrinogen assay:
decreased
- peripheral blood smear:
microangiopathic blood film with schistocytes
- D-dimer/fibrin degradation products:
elevated
Other investigations
Wiskott-Aldrich syndrome
History
positive family history, typically presents at birth, prolonged bleeding from umbilical stump or with procedures
Exam
petechiae, chronic eczema, lymphadenopathy, hepatosplenomegaly
1st investigation
- CBC:
thrombocytopenia with small platelet volume
- WAS protein gene mutation analysis:
positive
Other investigations
- immunoglobulin levels:
variable: low to normal IgG and IgM, elevated IgA and IgE
MYH9-related disorders
History
formerly known as May-Hegglin anomaly; positive family history, may be associated with Alport syndrome, often found incidentally on routine blood tests
Exam
no specific findings
1st investigation
- CBC:
thrombocytopenia with large platelet volume
- peripheral blood smear:
abnormally large platelets, abnormal neutrophil inclusions (Doehle-like bodies)
Other investigations
Bernard-Soulier disease
History
positive family history, abnormal bleeding with procedures, epistaxis, menorrhagia
Exam
ecchymosis is usually the only finding
1st investigation
- CBC:
possible thrombocytopenia with large platelet volume
- peripheral blood smear:
abnormally large platelets
- platelet aggregation test:
lack of aggregation response in the presence of ristocetin; normal aggregation in response to adenosine diphosphate, epinephrine, and collagen
- flow cytometry:
lack of glycoprotein Ib/IX/V receptors
Other investigations
- platelet function analyzer (PFA-100):
prolonged
Thrombocytopenia with absent radius syndrome
History
positive family history, present at birth, may have congenital heart disease
Exam
absent bilateral radius bones (although thumbs are always present), other abnormalities of the upper limbs may be present
1st investigation
- CBC:
severe thrombocytopenia
Other investigations
- genetic testing:
positive
More
Glanzmann thrombasthenia
History
abnormal bleeding with procedures, epistaxis, menorrhagia
Exam
ecchymosis is usually the only finding
1st investigation
- CBC:
normal
- platelet aggregation test:
lack of aggregation response in the presence of adenosine diphosphate, epinephrine, and collagen; normal aggregation in response to ristocetin
- flow cytometry:
lack of glycoprotein IIb/IIIa receptors
Other investigations
- platelet function analyzer (PFA-100):
prolonged
Acute myelogenous leukemia
History
fatigue, infections, mucosal bleeding
Exam
petechiae and/or ecchymosis on extremities, pallor, fever, may appear ill
1st investigation
- CBC:
thrombocytopenia, neutropenia, anemia, elevated WBC count
- peripheral blood smear:
circulating blasts, presence of Auer rods
- bone marrow biopsy:
blasts >20%, Auer rods
More
Acute lymphocytic leukemia
History
fatigue, infections, mucosal bleeding
Exam
petechiae and/or ecchymosis on extremities, pallor, fever, may appear ill, lymphadenopathy, hepatosplenomegaly
1st investigation
- CBC:
thrombocytopenia, neutropenia, anemia, elevated WBC count
- peripheral blood smear:
leukemic lymphoblasts
- bone marrow biopsy:
blasts >20%
More
Other investigations
- coagulation studies:
may be normal or abnormal
More
Hodgkin lymphoma
History
B symptoms (e.g., fever, drenching night sweats, weight loss)
Exam
lymphadenopathy, possible splenomegaly/hepatomegaly
1st investigation
Other investigations
- PET scan:
increased uptake of tracer at involved sites
- CT scan:
may show enlarged lymph node(s), spleen, or liver
Non-Hodgkin lymphoma
History
B symptoms (e.g., fever, drenching night sweats, weight loss)
Exam
lymphadenopathy, possible splenomegaly
1st investigation
Other investigations
- PET scan:
increased uptake of tracer at involved sites
- CT scan:
may show enlarged lymph node(s), spleen, or liver
Multiple myeloma
History
bone pain, fatigue; CRAB symptoms (i.e., high calcium, renal dysfunction, anemia, bone lesions)
Exam
pallor
1st investigation
- CBC:
thrombocytopenia, neutropenia, possible anemia
- basic metabolic panel:
elevated creatinine, hypercalcemia
- bone marrow biopsy:
plasma cell infiltrates (>5%) in bone marrow
- monoclonal protein workup:
positive for monoclonal protein
More
Other investigations
- skeletal survey:
lytic lesions
- MRI spine:
bone disease and bone marrow infiltration
Solid tumor with infiltration of bone marrow
History
history of metastatic disease, bone pain
Exam
possible palpable mass
1st investigation
- CBC:
thrombocytopenia, neutropenia, possible anemia
- bone marrow biopsy:
presence of metastatic tumor cells
Other investigations
- CT scan:
mass identified
Myelofibrosis
History
nonspecific constitutional symptoms (e.g., fever, night sweats, weight loss), history of myeloproliferative disease, abdominal discomfort, early satiety
Exam
splenomegaly, hepatomegaly, features of portal hypertension
1st investigation
- CBC:
thrombocytopenia, neutropenia, possible anemia
- JAK2 mutation analysis:
positive
More - bone marrow biopsy:
marrow fibrosis, hypocellularity
Other investigations
- ultrasound/CT spleen:
enlarged spleen
- lactate dehydrogenase level:
elevated
Myelodysplastic syndrome
History
common in older patients (>65 years), history of recurrent infections, fatigue, mucosal bleeding
Exam
pallor
1st investigation
- CBC:
thrombocytopenia, neutropenia, anemia
- peripheral blood smear:
low number of red blood cells, white blood cells, and platelets; dysplastic white blood cells; occasional circulating blasts
- bone marrow biopsy and cytogenetic analyses:
hypercellular marrow, characteristic cytogenetic changes, characteristic significant dysplastic changes in ≥10% bone marrow precursor cells
Other investigations
Aplastic anemia
History
history of recurrent infections, significant fatigue, mucosal bleeding
Exam
pallor, tachycardia, dyspnea
1st investigation
- CBC:
thrombocytopenia, neutropenia, anemia
- reticulocyte count:
low
- peripheral blood smear:
pancytopenia with normal morphology
- bone marrow biopsy and cytogenetic analyses:
hypocellular marrow with no abnormal cell population or fibrosis
Other investigations
Hemophilia
History
positive family history, mostly male sex (females can be symptomatic carriers), abnormal bleeding with procedures
Exam
signs of joint bleeding (e.g., pain, swelling, erythema) or chronic hemarthrosis (e.g., limited range of motion)
1st investigation
- activated partial thromboplastin time:
usually prolonged; corrected in mixing study
- factor (VIII, IX) assay:
decreased or absent factor levels
Other investigations
Factor V, VII, X, or XI deficiency
Acquired coagulation inhibitors
History
older age, malignancy, postpartum (factor VIII inhibitors)
Exam
significant ecchymosis, active bleeding symptoms, life-threatening bleeding
1st investigation
- activated partial thromboplastin time:
prolonged; remains prolonged with mixing study
- factor assays:
low
More - Bethesda assay:
positive titer
Other investigations
Vitamin C deficiency
History
lack of fresh fruit/vegetables over prolonged periods
Exam
dental deterioration, impaired wound healing, coiled hairs
1st investigation
- serum ascorbic acid level:
low
More
Other investigations
- prothrombin time/activated partial thromboplastin time:
normal
Marfan syndrome
History
positive family history
Exam
fits diagnostic criteria (e.g., lens subluxation, aortic dilation or dissection, dural ectasia, musculoskeletal features), tall stature, stretch marks, pectus excavatum (funnel chest), mitral valve murmur, aortic valve murmur
1st investigation
- genetic testing:
positive
More
Other investigations
Ehlers-Danlos syndrome
History
positive family history, joint hypermobility (this alone is not enough for a diagnosis), hyperextensive skin, unusual scars, poor wound healing, spontaneous ruptures of organ or dissection of blood vessel
Exam
joint dislocations or subluxations, translucent skin
1st investigation
- clinical diagnosis:
diagnosis is made based on history and examination
Other investigations
- genetic testing:
positive
More
Acute liver failure
History
hepatitis infection, autoimmune disease, heavy alcohol use, right upper quadrant abdominal pain, anorexia, fatigue, bleeding
Exam
jaundice, confusion (if severe)
1st investigation
- CBC:
variable
- LFTs:
significantly elevated aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, and/or bilirubin (depending on the severity of disease)
- prothrombin time/activated partial thromboplastin time:
prolonged
Other investigations
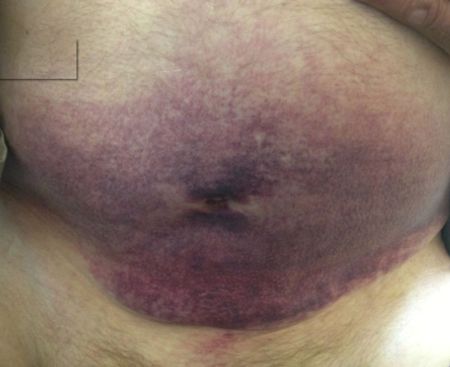
Gardner-Diamond syndrome
History
young age, female sex, psychiatric disorder, painful bruising
Exam
ecchymosis characterized by synchronous appearance, morphology of central clearing, and frequent painful prodromes
1st investigation
- clinical diagnosis:
diagnosis is made based on history and examination
Other investigations
Use of this content is subject to our disclaimer