Approach
Diagnosis of malignancy-associated hypercalcaemia is based on a history of malignancy, signs/symptoms of hypercalcaemia, presence of hypercalcaemia, and biochemical work-up to determine the underlying aetiology of hypercalcaemia.
History and physical examination
Symptoms of hypercalcaemia include neuropsychiatric changes (e.g., mood disturbance, fatigue, confusion, stupor, and coma), gastrointestinal disturbance (loss of appetite, nausea, constipation), muscle weakness, polyuria, polydipsia, and bone pain.[1][2][5][10][13] Signs of dehydration associated with hypercalcaemia include poor skin turgor and dry mucous membranes. However, hypercalcaemia may not be associated with any specific physical examination findings.
History to evaluate potential causes of hypercalcaemia unrelated to malignancy should be elicited.[1][5] These include hyperthyroidism, phaeochromocytoma, adrenal insufficiency, and granulomatous disease. A thorough medication history to evaluate for use of medications that may cause or worsen hypercalcaemia (thiazide diuretics, lithium, calcium, over-the-counter antacids, and large doses of vitamin D) should be undertaken.[1][5][10]
Severity of symptoms may correlate with duration and rapidity of onset of hypercalcaemia.[10] It is important to note that malignancy-associated hypercalcaemia is less commonly associated with life-threatening decompensation, but a hypercalcaemic crisis (characterised by oliguria, anuria, somnolence, coma) can occur.
An ECG should be performed to assess for a shortened QT interval and dysrhythmias.
Laboratory evaluation
Biochemical evidence of hypercalcaemia should be demonstrated by measuring total serum calcium and albumin in order to calculate the adjusted serum calcium level. Some sources prefer measurement of serum ionised calcium, if available. Serum ionised calcium should be measured if the albumin level is altered, and if calcium-binding immunoglobulins may be present (e.g., in multiple myeloma).[1]
Parathyroid hormone (PTH)-dependent hypercalcaemia should be ruled out by measuring a serum intact PTH level.[5] Conditions associated with elevated PTH include primary and tertiary hyperparathyroidism, familial hypocalciuric hypercalcaemia, and ectopic hyperparathyroidism.
A complete metabolic panel should be ordered to check for hypercalcaemia-induced acute kidney injury. A high bicarbonate level may indicate that malignancy or exogenous calcium excess may be a more likely cause of hypercalcaemia than primary hyperparathyroidism.
The aetiology of non-PTH-dependent hypercalcaemia should be determined. Conditions associated with hypercalcaemia and an appropriately suppressed PTH include malignancy-associated hypercalcaemia, hyperthyroidism, phaeochromocytoma, and adrenal insufficiency.
All laboratory tests should be obtained before treatment is started, as improvement of hypercalcaemia after treatment is initiated may cause difficulty in interpreting test results. The following tests are also recommended:
Screening for hyperthyroidism, phaeochromocytoma, and adrenal insufficiency, as clinically indicated.
Serum parathyroid hormone-related peptide (PTHrP). An elevated PTHrP associated with a suppressed PTH and low to low-normal calcitriol (1,25-dihydroxyvitamin D) level represents likely humoral hypercalcaemia of malignancy. PTHrP-mediated hypercalcaemia typically occurs with non-metastatic tumours that may be apparent on examination and initial imaging. Exceptions include small neuro-endocrine tumours.[1]
Serum phosphorus. In humoral hypercalcaemia of malignancy, PTHrP also acts at the level of the kidney to reduce calcium clearance, as well as to reduce the renal phosphorus threshold, leading to hyperphosphaturia and hypophosphataemia.[1][5]
Calcitriol (serum 1,25-dihydroxyvitamin D) level, if lymphoma and/or granulomatous disease are suspected. Calcitriol (1,25-dihydroxyvitamin D)-mediated hypercalcaemia occurs with lymphomas of all kinds and granulomatous disorders.
Serum 25-hydroxyvitamin D, if intravenous bisphosphonate or subcutaneous denosumab is being considered. Vitamin D deficiency should be corrected prior to administration of bisphosphonates or denosumab to avoid the risk of hypocalcaemia and, possibly, osteonecrosis of the jaw.[17][18][19][20]
If there is a history of malignancy complicated by skeletal involvement, PTHrP and calcitriol (1,25-dihydroxyvitamin D) are found to be normal, and other aetiologies of hypercalcaemia have been eliminated, local osteolytic hypercalcaemia is the most likely diagnosis.[Figure caption and citation for the preceding image starts]: CT chest showing compression fracture of multiple vertebral bodies in a child presenting with acute lymphoblastic leukaemia. Biochemistry showed hypercalcaemia with a suppressed parathyroid hormone levelSukumar SP, Balachandran K, Sahoo JP, et al. Acute lymphocytic leukaemia presenting as a metabolic bone disease. BMJ Case Reports 2013; doi:10.1136/bcr-2013-008758 [Citation ends].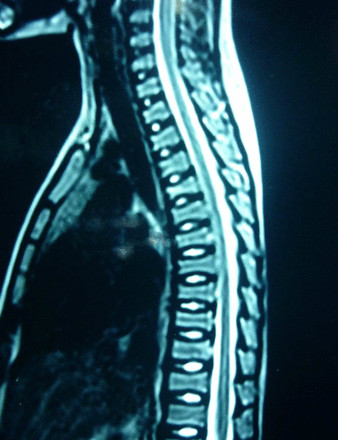 [Figure caption and citation for the preceding image starts]: Whole body planar images suggestive of skeletal infiltration in a child with acute lymphoblastic leukaemia showing areas of abnormal increased uptake. Biochemistry showed hypercalcaemia with a suppressed parathyroid hormone levelSukumar SP, Balachandran K, Sahoo JP, et al. Acute lymphocytic leukaemia presenting as a metabolic bone disease. BMJ Case Reports 2013; doi:10.1136/bcr-2013-008758 [Citation ends].
[Figure caption and citation for the preceding image starts]: Whole body planar images suggestive of skeletal infiltration in a child with acute lymphoblastic leukaemia showing areas of abnormal increased uptake. Biochemistry showed hypercalcaemia with a suppressed parathyroid hormone levelSukumar SP, Balachandran K, Sahoo JP, et al. Acute lymphocytic leukaemia presenting as a metabolic bone disease. BMJ Case Reports 2013; doi:10.1136/bcr-2013-008758 [Citation ends].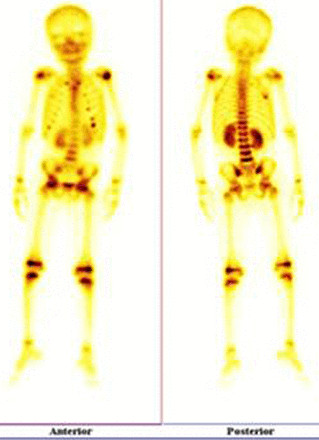
Radiology evaluation
In order to assess for underlying causes of hypercalcaemia, the following tests should be considered:
Skeletal survey in patients in whom multiple myeloma, bone metastases, or leukaemia are suspected.
Chest x-ray to assess for lung cancer, sarcoidosis, or tuberculosis.
Further imaging should be ordered, according to the suspected cancer or condition and the anatomical region involved.
Other tests
An ECG should be performed to look for shortened QT interval or other conduction abnormalities.[2]
Use of this content is subject to our disclaimer