The causes of persistent pulmonary infiltrate may be infectious or noninfectious.[1]Menendez R, Perpina M, Torres A. Evaluation of non-resolving and progressive pneumonia. Semin Respir Infect. 2003 Jun;18(2):103-11.
http://www.ncbi.nlm.nih.gov/pubmed/12840791?tool=bestpractice.com
[2]Kuru T, Lynch JP 3rd. Non-resolving or slowly resolving pneumonia. Clin Chest Med. 1999 Sep;20(3):623-51.
http://www.ncbi.nlm.nih.gov/pubmed/10516909?tool=bestpractice.com
[3]Cunha BA. Slowly resolving and nonresolving pneumonias. Drugs Today (Barc). 2000 Dec;36(12):829-34.
http://www.ncbi.nlm.nih.gov/pubmed/12845341?tool=bestpractice.com
Patients with persistent pulmonary infiltrate may present with or without clinical symptoms (e.g., cough, hemoptysis). Comprehensive investigation of the nature of persistent pulmonary infiltrate may be warranted when clinical improvement has not occurred with treatment, if chest radiographic findings remain unchanged or worsen, or if the rate of radiographic resolution is delayed.[2]Kuru T, Lynch JP 3rd. Non-resolving or slowly resolving pneumonia. Clin Chest Med. 1999 Sep;20(3):623-51.
http://www.ncbi.nlm.nih.gov/pubmed/10516909?tool=bestpractice.com
Infectious
About 10% to 25% of patients with community-acquired pneumonia and 30% to 60% of those with nosocomial pneumonia do not improve despite therapy.[13]Menendez R, Torres A. Treatment failure in community-acquired pneumonia. Chest. 2007 Oct;132(4):1348-55.
http://www.ncbi.nlm.nih.gov/pubmed/17934120?tool=bestpractice.com
[16]Arancibia F, Ewig S, Martinez JA, et al. Antimicrobial treatment failures in patients with community-acquired pneumonia: causes and prognostic implications. Am J Respir Crit Care Med. 2000 Jul;162(1):154-60.
http://www.atsjournals.org/doi/full/10.1164/ajrccm.162.1.9907023
http://www.ncbi.nlm.nih.gov/pubmed/10903235?tool=bestpractice.com
Community-acquired pneumonia may be secondary to atypical organisms (e.g., Mycoplasma pneumoniae, Chlamydophila pneumoniae, Legionella pneumophila, or respiratory viruses) and is often seen in young adults living in close proximity to those infected by these microorganisms.
Older and immunosuppressed patients are more susceptible to viral pneumonia, and secondary or superinfection with other organisms (e.g., Staphylococcus aureus, Haemophilus influenzae) is common.
Tuberculosis, in endemic areas, should be considered whenever pulmonary infiltrate persists after conventional antibiotic therapy. Fungal pneumonia (e.g., Pneumocystis jiroveci) may be accompanied by fungal granulomas. Viral pneumonia is often associated with organizing pneumonia leading to persistent pulmonary infiltrate. It may present clinically in a manner similar to community-acquired pneumonia (i.e., flu-like illness with fever, malaise, fatigue, cough), with a persisting recurrent or migratory bilateral diffuse alveolar infiltrate.[17]Gross TJ, Chavis AD, Lynch JP 3rd. Noninfectious pulmonary diseases masquerading as community-acquired pneumonia. Clin Chest Med. 1991 Jun;12(2):363-93.
http://www.ncbi.nlm.nih.gov/pubmed/1855377?tool=bestpractice.com
[18]Lynch JP 3rd, Sitrin RG. Noninfectious mimics of community acquired pneumonia. Semin Respir Infect. 1993 Mar;8(1):14-45.
http://www.ncbi.nlm.nih.gov/pubmed/8372273?tool=bestpractice.com
[19]Andrade CR, Ibiapina CC, Champs NS, et al. Avian influenza: the threat of the 21st century. J Bras Pneumol. 2009 May;35(5):470-9.
http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1806-37132009000500014&lng=en&nrm=iso&tlng=en
http://www.ncbi.nlm.nih.gov/pubmed/19547858?tool=bestpractice.com
Resistant or unusual pathogens (fungi, Mycoplasma tuberculosis, Nocardia, or Actinomyces), and allergic bronchopulmonary Aspergillus may also cause persistent pulmonary infiltrate.[20]Low DE, Mazzulli T, Marrie T. Progressive and nonresolving pneumonia. Curr Opin Pulm Med. 2005 May;11(3):247-52.
http://www.ncbi.nlm.nih.gov/pubmed/15818188?tool=bestpractice.com
[21]Weyers CM, Leeper KV. Nonresolving pneumonia. Clin Chest Med. 2005 Mar;26(1):143-58.
http://www.ncbi.nlm.nih.gov/pubmed/15802176?tool=bestpractice.com
Complications of pneumonia, like empyema and abscess, can result in nonresolving pneumonia especially in patients with comorbid conditions. Computed tomography (CT) scan is generally used as a diagnostic modality, with or without an air bronchogram in the presence of an alveolar infiltrate. Thoracentesis is a definitive procedure in case of empyema and no other tests are required. Obstruction caused by lung cancer (e.g., bronchogenic carcinoma, bronchial carcinoid tumors, papillomas, or metastatic lesions such as breast, kidneys, or gastrointestinal tract) can lead to recurrent postobstructive nonresolving pneumonia or abscess.
[Figure caption and citation for the preceding image starts]: Causes of nonresolving pneumoniaCreated by the BMJ Knowledge Centre based on tables from Athanasia Pataka [Citation ends].
Immunosuppressed
Patients with AIDS and non-HIV-immunocompromised hosts may present several possibilities for persistent pulmonary infiltrate (e.g., P jiroveci pneumonia, tuberculosis).[22]Boyton RJ. Infectious lung complications in patients with HIV/AIDS. Curr Opin Pulm Med. 2005 May;11(3):203-7.
http://www.ncbi.nlm.nih.gov/pubmed/15818180?tool=bestpractice.com
[23]Kanmogne GD. Noninfectious pulmonary complications of HIV/AIDS. Curr Opin Pulm Med. 2005 May;11(3):208-12.
http://www.ncbi.nlm.nih.gov/pubmed/15818181?tool=bestpractice.com
[24]Shorr AF, Susla GM, O'Grady NP. Pulmonary infiltrate in the non-HIV-infected immunocompromised patient: etiologies, diagnostic strategies, and outcomes. Chest. 2004 Jan;125(1):260-71.
http://www.ncbi.nlm.nih.gov/pubmed/14718449?tool=bestpractice.com
[25]Crawford S. Noninfectious lung disease in the immunocompromised host. Respiration. 1999;66(5):385-95.
http://content.karger.com/produktedb/produkte.asp?DOI=29418&typ=pdf
http://www.ncbi.nlm.nih.gov/pubmed/10516534?tool=bestpractice.com
[26]Maschmeyer G, Carratalà J, Buchheidt D, et al. Diagnosis and antimicrobial therapy of lung infiltrates in febrile neutropenic patients (allogeneic SCT excluded): updated guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Medical Oncology (DGHO). Ann Oncol. 2015 Jan;26(1):21-33.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4269340
http://www.ncbi.nlm.nih.gov/pubmed/24833776?tool=bestpractice.com
[27]Leone S, Nicastri E, Giglio S, et al. Immune reconstitution inflammatory syndrome associated with Mycobacterium tuberculosis infection: a systematic review. Int J Infect Dis. 2010 Apr;14(4):e283-91.
http://www.ncbi.nlm.nih.gov/pubmed/19656712?tool=bestpractice.com
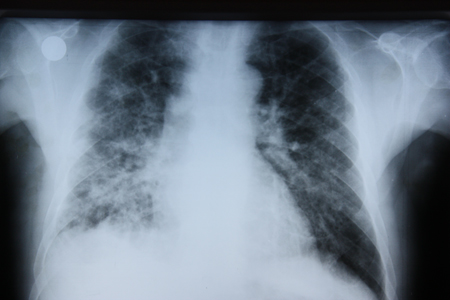
Kaposi sarcoma may cause persistent pulmonary infiltrate.[Figure caption and citation for the preceding image starts]: Posterior-anterior chest x-ray in Pneumocystis jiroveci pneumonia showing severe, bilateral pulmonary interstitial infiltrates with pneumatocelesFrom the collection of Matthew Gingo, UPMC [Citation ends].
[Figure caption and citation for the preceding image starts]: Causes of persistent pulmonary infiltrate in immunocompromised patientsCreated by the BMJ Knowledge Centre based on tables from Athanasia Pataka [Citation ends].
Malignant
Smokers ages >45 years with recurrent pneumonia, hemoptysis, and weight loss should be evaluated for a possible malignancy.[2]Kuru T, Lynch JP 3rd. Non-resolving or slowly resolving pneumonia. Clin Chest Med. 1999 Sep;20(3):623-51.
http://www.ncbi.nlm.nih.gov/pubmed/10516909?tool=bestpractice.com
Bronchoalveolar cell carcinoma may present as an alveolar infiltrate with an air bronchogram, resembling nonresolving pneumonia. Lymphoma may also present as an alveolar infiltrate, often with an air bronchogram. Kaposi sarcoma may cause persistent pulmonary infiltrate, particularly in patients with AIDS.
Pulmonary parenchymal
A foreign body in the airways may cause recurrent postobstructive nonresolving pneumonia distal to the obstructing object.[2]Kuru T, Lynch JP 3rd. Non-resolving or slowly resolving pneumonia. Clin Chest Med. 1999 Sep;20(3):623-51.
http://www.ncbi.nlm.nih.gov/pubmed/10516909?tool=bestpractice.com
[28]Teramoto S, Matsuse T, Ouchi Y. Foreign body aspiration into the lower airways may not be unusual in older adults. Chest. 1998 Jun;113(6):1733-4.
http://www.ncbi.nlm.nih.gov/pubmed/9631831?tool=bestpractice.com
Aspiration pneumonia is characterized by a history of recumbency, halitosis, and dysphagia in a debilitated or paralyzed patient. The classic radiologic finding is an infiltrate in dependent lung fields with a sputum culture of oral or mixed flora.
Lipoid pneumonia develops when lipids enter the bronchial tree.[29]Spickard A 3rd, Hirschmann JV. Exogenous lipoid pneumonia. Arch Intern Med. 1994 Mar 28;154(6):686-92.
http://www.ncbi.nlm.nih.gov/pubmed/8129503?tool=bestpractice.com
Lipids may be inhaled (e.g., nose drops with an oil base, accidental inhalation of cosmetic oil) or may fill the lumen of bronchi and microairways distal to the obstruction. Typical biopsy findings include lipid-laden foamy macrophages and giant cells. Infiltrating amyloidosis is an uncommon cause of persistent pulmonary infiltrate.[30]Utz JP, Swensen SJ, Gertz MA. Pulmonary amyloidosis: the Mayo Clinic experience from 1980 to 1993. Ann Intern Med. 1996 Feb 15;124(4):407-13.
http://www.ncbi.nlm.nih.gov/pubmed/8554249?tool=bestpractice.com
Cardiovascular
Cardiogenic pulmonary edema can manifest as asymmetric infiltrative patterns in patients with COPD.[31]Rudiger A, Gasser S, Fischler M, et al. Comparable increase of B-type natriuretic peptide and amino-terminal pro-B-type natriuretic peptide levels in patients with severe sepsis, septic shock, and acute heart failure. Crit Care Med. 2006 Aug;34(8):2140-4.
http://www.ncbi.nlm.nih.gov/pubmed/16763507?tool=bestpractice.com
[32]Maisel A. B-type natriuretic peptide levels: diagnostic and prognostic in congestive heart failure: what's next? Circulation. 2002 May 21;105(20):2328-31.
http://www.ncbi.nlm.nih.gov/pubmed/12021215?tool=bestpractice.com
[33]Gluecker T, Capasso P, Schnyder P, et al. Clinical and radiologic features of pulmonary edema: a pictorial essay. Radiographics. 1999 Nov-Dec;19(6):1507-31.
http://radiographics.rsnajnls.org/cgi/content/full/19/6/1507
http://www.ncbi.nlm.nih.gov/pubmed/10555672?tool=bestpractice.com
It persists if treated only with antibiotics. Migrating, transient infiltration is typically found on serial chest x-ray. Comparison of supine and prone views may be helpful, as the basilar infiltrate of pulmonary edema generally improves with the prone position. These patients typically have clinical signs (e.g., heart murmurs, S3, peripheral edema, elevated jugular venous pressure) that facilitate correct diagnosis.
Pulmonary embolism with infarction can mimic pneumonia that resolves slowly. The classic triad of acute dyspnea, chest pain, and hemoptysis is only rarely seen clinically. The chest x-ray findings of thromboembolic disease may be nonspecific, with cavitated consolidation and right heart enlargement. Serial studies of the chest using conventional radiography or CT demonstrate gradual clearing from the periphery of the infiltrate toward its center (melting ice sign). CT angiogram or spiral (helical) CT scanning with intravenous contrast permits visualization of the embolus, which may be accompanied by wedge-shaped consolidation.[34]van Belle A, Buller HR, Huisman MV, et al; Writing Group for the Christopher Study Investigators. Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, D-dimer testing, and computed tomography. JAMA. 2006 Jan 11;295(2):172-9.
http://jama.jamanetwork.com/article.aspx?articleid=202176
http://www.ncbi.nlm.nih.gov/pubmed/16403929?tool=bestpractice.com
[35]Stein PD, Woodard PK, Weg JG, et al. Diagnostic pathways in acute pulmonary embolism: recommendations of the PIOPED II investigators. Am J Med. 2006 Dec;119(12):1048-55.
http://www.ncbi.nlm.nih.gov/pubmed/17145249?tool=bestpractice.com
Inflammatory/immunologic
Patients with connective tissue disorders also may present with pulmonary infiltrate. Systemic lupus erythematosus may affect the lung, its vasculature, the pleura, and even the diaphragm. The most common manifestation of pulmonary disease in patients with rheumatoid arthritis is interstitial lung disease. Pulmonary disease in patients with dermatomyositis or polymyositis may reflect either a complication of the underlying inflammatory myopathy or an adverse effect of medications used for treatment. Scleroderma may cause recurrent aspiration pneumonitis due to esophageal disorders.
Interstitial lung diseases can cause different types of radiologic abnormalities, including persistent pulmonary infiltrate. These diseases may be idiopathic or associated with occupational or environmental exposures, drugs, and collagen-related or vascular diseases.[36]Travis WD, Costabel U, Hansell DM, et al; ATS/ERS Committee on Idiopathic Interstitial Pneumonias. An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013 Sep 15;188(6):733-48.
https://www.thoracic.org/statements/resources/interstitial-lung-disease/classification-of-IIPs.pdf
http://www.ncbi.nlm.nih.gov/pubmed/24032382?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Etiologies and possible differential diagnosis of interstitial lung diseaseCreated by the BMJ Knowledge Centre based on tables from Athanasia Pataka [Citation ends].
Organizing pneumonia can also be associated with connective tissue disorders, other interstitial pneumonias, infection, drugs, or malignancies. It may have clinical presentation similar with that of community-acquired pneumonia (i.e., flu-like illness with fever, malaise, fatigue, cough) and chest imaging findings similar to those of persisting recurrent or migratory bilateral diffuse alveolar infiltrates.
Diffuse alveolar hemorrhage can be caused by a variety of diseases (e.g., connective tissue vascular disorders, drugs, mitral valve disease, infection) and may mimic pneumonia that persists with diffuse opacities on chest imaging.[5]Orens JB, Sitrin RG, Lynch JP 3rd. The approach to nonresolving pneumonia. Med Clin North Am. 2004 Feb;52(2):224-9.
http://www.ncbi.nlm.nih.gov/pubmed/8078373?tool=bestpractice.com
[17]Gross TJ, Chavis AD, Lynch JP 3rd. Noninfectious pulmonary diseases masquerading as community-acquired pneumonia. Clin Chest Med. 1991 Jun;12(2):363-93.
http://www.ncbi.nlm.nih.gov/pubmed/1855377?tool=bestpractice.com
[18]Lynch JP 3rd, Sitrin RG. Noninfectious mimics of community acquired pneumonia. Semin Respir Infect. 1993 Mar;8(1):14-45.
http://www.ncbi.nlm.nih.gov/pubmed/8372273?tool=bestpractice.com
[37]Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997 Sep;40(9):1725.
http://www.ncbi.nlm.nih.gov/pubmed/9324032?tool=bestpractice.com
[38]Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988 Mar;31(3):315-24.
http://www.ncbi.nlm.nih.gov/pubmed/3358796?tool=bestpractice.com
[39]LeRoy EC, Black C, Fleischmajer R, et al. Scleroderma (systemic sclerosis): classification, subsets, and pathogenesis. J Rheumatol. 1988 Feb;15(2):202-5.
http://www.ncbi.nlm.nih.gov/pubmed/3361530?tool=bestpractice.com
Systemic vasculitis may affect the lower respiratory tract and present as cough, dyspnea, hemoptysis, persistent alveolar opacities, diffuse hazy opacities (which may reflect alveolar hemorrhage), cavitary nodules, and pleural effusion.[17]Gross TJ, Chavis AD, Lynch JP 3rd. Noninfectious pulmonary diseases masquerading as community-acquired pneumonia. Clin Chest Med. 1991 Jun;12(2):363-93.
http://www.ncbi.nlm.nih.gov/pubmed/1855377?tool=bestpractice.com
Granulomatosis with polyangiitis (formerly known as Wegener granulomatosis) is a systemic vasculitis that primarily involves the upper and lower respiratory tracts and kidneys. Pulmonary granulomatosis with polyangiitis can present as multifocal lung involvement or solitary lung lesions with no evidence of extrapulmonary disease.
Sarcoidosis can involve any organ, but respiratory symptoms combined with chest radiographs with pulmonary infiltration alone, without the characteristic bilateral hilar lymphadenopathy, can mimic pneumonia that persists despite antibiotic treatment.[40]Costabel U. Sarcoidosis: clinical update. Eur Respir J Suppl. 2001 Sep;32:56s-68s.
http://erj.ersjournals.com/cgi/content/full/18/32_suppl/56S
http://www.ncbi.nlm.nih.gov/pubmed/11816825?tool=bestpractice.com
Occupational and environmental exposures are important.[41]Infante PF, Newman LS. Beryllium exposure and chronic beryllium disease. Lancet. 2004 Feb 7;363(9407):415-6.
http://www.ncbi.nlm.nih.gov/pubmed/14962519?tool=bestpractice.com
[42]Bégin R, Cantin A, Massé S. Recent advances in the pathogenesis and clinical assessment of mineral dust pneumoconioses: asbestosis, silicosis and coal pneumoconiosis. Eur Respir J. 1989 Nov;2(10):988-1001.
http://www.ncbi.nlm.nih.gov/pubmed/2691279?tool=bestpractice.com
[43]American Thoracic Society. Diagnosis and initial management of nonmalignant diseases related to asbestos. Am J Respir Crit Care Med. 2004 Sep 15;170(6):691-715.
https://www.atsjournals.org/doi/full/10.1164/rccm.200310-1436ST#.U7_nqvldVlw
http://www.ncbi.nlm.nih.gov/pubmed/15355871?tool=bestpractice.com
[44]American Thoracic Society Committee of the Scientific Assembly on Environmental and Occupational Health. Adverse effects of crystalline silica exposure. Am J Respir Crit Care Med. 1997 Feb;155(2):761-8.
http://www.ncbi.nlm.nih.gov/pubmed/9032226?tool=bestpractice.com
Inhaled aerosols from electronic cigarettes (e-cigarettes) can contain harmful or potentially harmful substances (e.g., heavy metals, ultrafine particles, volatile organic compounds and other chemicals. Radiologic findings in people with severe pulmonary disease associated with e-cigarette use include pulmonary infiltrates on chest x-ray and bilateral ground glass infiltrates on chest CT.[45]Schier JG, Meiman JG, Layden J, et al. Severe pulmonary disease associated with electronic-cigarette-product use - interim guidance. MMWR Morb Mortal Wkly Rep. 2019 Sep 13;68(36):787-90.
https://www.cdc.gov/mmwr/volumes/68/wr/mm6836e2.htm?s_cid=mm6836e2_w
http://www.ncbi.nlm.nih.gov/pubmed/31513561?tool=bestpractice.com
Silicosis may account for diffuse persistent opacities on chest x-ray.[44]American Thoracic Society Committee of the Scientific Assembly on Environmental and Occupational Health. Adverse effects of crystalline silica exposure. Am J Respir Crit Care Med. 1997 Feb;155(2):761-8.
http://www.ncbi.nlm.nih.gov/pubmed/9032226?tool=bestpractice.com
Progressive massive fibrosis is usually associated with coal workers' pneumoconiosis and silicosis.
Asbestosis may be responsible for persistent interstitial and pleural infiltrates or rounded atelectasis (pleural adhesions and fibrosis causing deformation of the lung and bending of some small bronchi).[42]Bégin R, Cantin A, Massé S. Recent advances in the pathogenesis and clinical assessment of mineral dust pneumoconioses: asbestosis, silicosis and coal pneumoconiosis. Eur Respir J. 1989 Nov;2(10):988-1001.
http://www.ncbi.nlm.nih.gov/pubmed/2691279?tool=bestpractice.com
[43]American Thoracic Society. Diagnosis and initial management of nonmalignant diseases related to asbestos. Am J Respir Crit Care Med. 2004 Sep 15;170(6):691-715.
https://www.atsjournals.org/doi/full/10.1164/rccm.200310-1436ST#.U7_nqvldVlw
http://www.ncbi.nlm.nih.gov/pubmed/15355871?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Posterior-anterior chest x-ray with bibasilar linear interstitial changes consistent with asbestosisFrom the personal collection of Kenneth D. Rosenman, MD [Citation ends].
Eosinophilic pneumonias are a heterogeneous group of disorders characterized by abnormally increased numbers of eosinophils within the pulmonary parenchyma (with or without serum eosinophilia). They may cause persistent pulmonary infiltrate, but most patients improve with glucocorticoids.[46]Alberts WM. Eosinophilic interstitial lung disease. Curr Opin Pulm Med. 2004 Sep;10(5):419-24.
http://www.ncbi.nlm.nih.gov/pubmed/15316442?tool=bestpractice.com
[47]Allen JN, Magro CM, King MA. The eosinophilic pneumonias. Semin Respir Crit Care Med. 2002 Apr;23(2):127-34.
http://www.ncbi.nlm.nih.gov/pubmed/16088605?tool=bestpractice.com
[48]Loffler W. Transient lung infiltrations with blood eosinophilia. Int Arch Allergy Appl Immunol. 1956;8(1-2):54-9.
http://www.ncbi.nlm.nih.gov/pubmed/13331628?tool=bestpractice.com
[49]Solomon J, Schwarz M. Drug-, toxin-, and radiation therapy-induced eosinophilic pneumonia. Semin Respir Crit Care Med. 2006 Apr;27(2):192-7.
http://www.ncbi.nlm.nih.gov/pubmed/16612770?tool=bestpractice.com
[50]Zander DS. Allergic bronchopulmonary aspergillosis: an overview. Arch Pathol Lab Med. 2005 Jul;129(7):924-8.
http://www.archivesofpathology.org/doi/full/10.1043/1543-2165%282005%29129%5B924%3AABAAO%5D2.0.CO%3B2
http://www.ncbi.nlm.nih.gov/pubmed/15974818?tool=bestpractice.com
Acute idiopathic eosinophilic pneumonia may manifest as acute fever, cough, dyspnea, and pulmonary opacities that can lead to respiratory failure. Peripheral eosinophilia is rare at the time of presentation of idiopathic acute eosinophilic pneumonia (cause of acute infiltrates).
Idiopathic chronic eosinophilic pneumonia is characterized by subacute or chronic respiratory symptoms, alveolar and blood eosinophilia, and peripheral pulmonary infiltrates on chest imaging.
Loeffler syndrome was first described in 1932 in the context of parasitic infection, systemic eosinophilia, and chest infiltrates. Generally, these patients clinically present with a mild respiratory illness, with nonproductive cough, pleuritic chest pain, fever, and (rarely) hemoptysis.
Allergic bronchopneumonic aspergillosis is a hypersensitivity reaction to A fumigatus mold that has colonized the bronchi.[50]Zander DS. Allergic bronchopulmonary aspergillosis: an overview. Arch Pathol Lab Med. 2005 Jul;129(7):924-8.
http://www.archivesofpathology.org/doi/full/10.1043/1543-2165%282005%29129%5B924%3AABAAO%5D2.0.CO%3B2
http://www.ncbi.nlm.nih.gov/pubmed/15974818?tool=bestpractice.com
The disease typically affects patients with asthma or cystic fibrosis, but it is also associated with diminished immunity. Serology for Aspergillus may help to support the diagnosis. Skin-prick sensitivity for the organism is also a useful diagnostic adjunct.[Figure caption and citation for the preceding image starts]: Chest x-ray of a patient with eosinophilic pneumoniaFrom the collection of Athanasia Pataka, MD [Citation ends].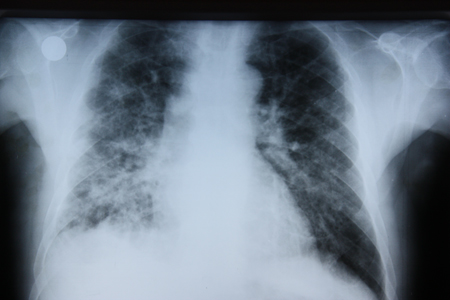
Hypersensitivity pneumonia (extrinsic allergic alveolitis) can lead to persistent pulmonary infiltrate with mid- to upper-zone predominance if exposure to the offending antigen continues.[51]Lacasse Y, Selman M, Costabel U, et al. Clinical diagnosis of hypersensitivity pneumonitis. Am J Respir Crit Care Med. 2003 Oct 15;168(8):952-8.
http://www.atsjournals.org/doi/full/10.1164/rccm.200301-137OC
http://www.ncbi.nlm.nih.gov/pubmed/12842854?tool=bestpractice.com
[52]Selman M. Hypersensitivity pneumonitis: a multifaceted deceiving disorder. Clin Chest Med. 2004 Sep;25(3):531-47.
http://www.ncbi.nlm.nih.gov/pubmed/15331190?tool=bestpractice.com
[53]Silva CI, Churg A, Muller NL. Hypersensitivity pneumonitis: spectrum of high-resolution CT and pathologic findings. AJR Am J Roentgenol. 2007 Feb;188(2):334-44.
http://www.ajronline.org/doi/full/10.2214/AJR.05.1826
http://www.ncbi.nlm.nih.gov/pubmed/17242239?tool=bestpractice.com
Pulmonary alveolar proteinosis is a rare lung disease resulting from decreased surfactant clearance, and it presents as persistent pulmonary infiltrate and shortness of breath.[17]Gross TJ, Chavis AD, Lynch JP 3rd. Noninfectious pulmonary diseases masquerading as community-acquired pneumonia. Clin Chest Med. 1991 Jun;12(2):363-93.
http://www.ncbi.nlm.nih.gov/pubmed/1855377?tool=bestpractice.com
[54]Shah PL, Hansell D, Lawson PR, et al. Pulmonary alveolar proteinosis: clinical aspects and current concepts on pathogenesis. Thorax. 2000 Jan;55(1):67-77.
http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=1745595&blobtype=pdf
http://www.ncbi.nlm.nih.gov/pubmed/10607805?tool=bestpractice.com
[55]Seymour JF, Presneill JJ. Pulmonary alveolar proteinosis: progress in the first 44 years. Am J Respir Crit Care Med. 2002 Jul 15;166(2):215-35.
http://www.atsjournals.org/doi/full/10.1164/rccm.2109105
http://www.ncbi.nlm.nih.gov/pubmed/12119235?tool=bestpractice.com
Infiltrating amyloidosis is an uncommon cause of persistent pulmonary infiltrate.
Pharmacologic/iatrogenic
Some medications (e.g., amiodarone, bleomycin, cyclophosphamide, vincristine, taxanes), cocaine, or other illicit drug use may cause persistent pulmonary abnormalities.[18]Lynch JP 3rd, Sitrin RG. Noninfectious mimics of community acquired pneumonia. Semin Respir Infect. 1993 Mar;8(1):14-45.
http://www.ncbi.nlm.nih.gov/pubmed/8372273?tool=bestpractice.com
[56]Camus P, Bonniaud P, Fanton A, et al. Drug-induced and iatrogenic infiltrative lung disease. Clin Chest Med. 2004 Sep;25(3):479-519.
http://www.ncbi.nlm.nih.gov/pubmed/15331188?tool=bestpractice.com
[57]Erasmus JJ, McAdams HP, Rossi SE. Drug-induced lung injury. Semin Roentgenol. 2002 Jan;37(1):72-81.
http://www.ncbi.nlm.nih.gov/pubmed/11987768?tool=bestpractice.com
[58]Camus P. Pneumotox online: the drug-induced respiratory disease website. Vol. 2, 2012 [internet publication].
http://www.pneumotox.com
Patients with malignancies undergoing chemotherapy or radiotherapy may present with persistent pulmonary infiltrate due to not only their malignancy but also complications of treatment.[26]Maschmeyer G, Carratalà J, Buchheidt D, et al. Diagnosis and antimicrobial therapy of lung infiltrates in febrile neutropenic patients (allogeneic SCT excluded): updated guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Medical Oncology (DGHO). Ann Oncol. 2015 Jan;26(1):21-33.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4269340
http://www.ncbi.nlm.nih.gov/pubmed/24833776?tool=bestpractice.com
[59]Carver JR, Shapiro CL, Ng A, et al. ASCO Cancer Survivorship Expert Panel. American Society of Clinical Oncology clinical evidence review on the ongoing care of adult cancer survivors: cardiac and pulmonary late effects. J Clin Oncol. 2007 Sep 1;25(25):3991-4008.
http://jco.ascopubs.org/cgi/content/full/25/25/3991
http://www.ncbi.nlm.nih.gov/pubmed/17577017?tool=bestpractice.com
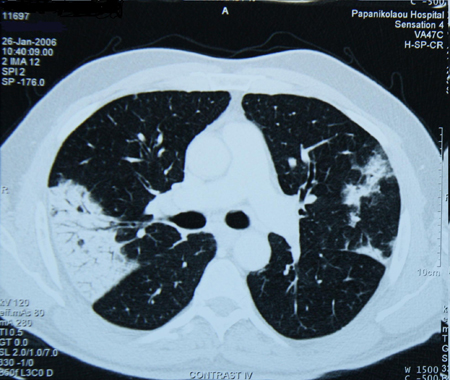
[Figure caption and citation for the preceding image starts]: Chest CT scan of a patient with amiodarone pulmonary toxicity showing asymmetric opacities with a peripheral distributionFrom the collection of Athanasia Pataka, MD [Citation ends].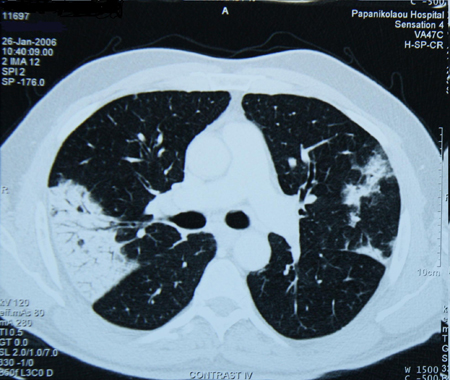 [Figure caption and citation for the preceding image starts]: Chest x-ray of a patient with amiodarone pulmonary toxicityFrom the collection of Athanasia Pataka, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Chest x-ray of a patient with amiodarone pulmonary toxicityFrom the collection of Athanasia Pataka, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Possible causal agents of drug-induced pulmonary parenchymal diseaseCreated by the BMJ Knowledge Centre based on tables from Athanasia Pataka [Citation ends].





 [Figure caption and citation for the preceding image starts]: Chest x-ray of a patient with amiodarone pulmonary toxicityFrom the collection of Athanasia Pataka, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Chest x-ray of a patient with amiodarone pulmonary toxicityFrom the collection of Athanasia Pataka, MD [Citation ends].