History and exam
Key diagnostic factors
common
history of laryngopharyngeal reflux or GERD
previous treatment for asthma without response to bronchodilators
episodic shortness of breath: rapid onset and resolution
Breathing attacks occur in response to a trigger (e.g., exercise, airborne irritant) and resolve with the elimination of that trigger. Often accompanied by tightness in the throat.
difficulty inhaling
Patients will often specifically describe air hunger and the inability to breathe in deeply, identifying the throat area specifically.
cough
Cough has been reported to be associated with paradoxical vocal fold motion (intermittent laryngeal obstruction) in up to 59% of cases.[1]
In addition to asthma and postnasal drip, cough can be related to distal and proximal acid exposure, upper-airway microaspiration, and dysphagia.[57]
It is considered to be on the continuum of vocal fold adductor behavior in response to sensory stimuli.
inspiratory stridor
Often loud and can cause fear in affected individuals and the people around them.
increased sensitivity to nonspecific triggers after initial exposure
Patients may report a paradoxical vocal fold motion (intermittent laryngeal obstruction) (PVFM/ILO) response to other airborne irritants such as smoke, cold, perfume, and chemical odors that were not triggers prior to the initial PVFM/ILO event.[58]
palpable laryngeal tension
Evidence of laryngeal elevation, pain and/or tenderness around the larynx, and narrowing of the thyroid hyoid space.[70]
uncommon
loss of consciousness
Patients may present to their primary care physician after an episode of loss of consciousness. They may report that they have been experiencing breathing difficulties for several months or years without loss of consciousness.
Risk factors
strong
laryngopharyngeal reflux (LPR)
In this condition small amounts of acid cause damage and irritation to laryngeal tissue through the retrograde flow of gastric contents to the laryngopharynx, without producing the common symptoms associated with GERD.
Endoscopic visualization of the larynx may confirm tissue damage including supraglottic, vocal fold, and diffuse laryngeal edema, erythema, posterior commissure hypertrophy, granulation tissue, and thick endolaryngeal mucus.[56][Figure caption and citation for the preceding image starts]: Laryngopharyngeal reflux: bilateral edema and erythema of the vocal folds with epithelial layer thickness, interarytenoid thicknessFrom the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].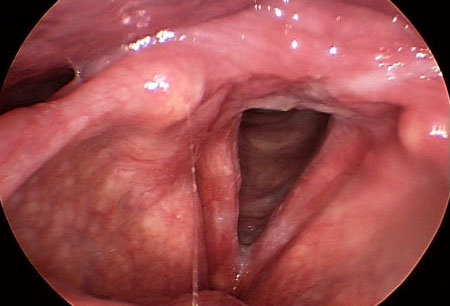
Common symptoms of LPR have been documented to include hoarseness; coughing; throat clearing; excessive mucus/postnasal drip; difficulty swallowing food, liquid, or pills; coughing after eating or lying down; breathing difficulty or choking episodes; troublesome or annoying cough; sensation of something sticking in throat; heartburn; chest pain; indigestion; and stomach acid coming up.[56]
Reflux Symptom Index score >13 indicates a correlation with LPR (a self-administered 9-question symptom score; 0-45 points).[56]
GERD
GERD is one of the most common causes of chronic cough. When GERD causes cough, there may be no other identifiable symptoms typical of GERD up to 75% of the time.[57]
GERD-associated cough may be the result of acid exposure in the distal esophagus stimulating the cough reflex via the vagus nerve or microaspiration into the laryngopharynx and trachea.[58]
asthma
occupational/environmental irritant exposure
Individuals who experience a rapid onset of respiratory symptoms following a single exposure to a respiratory irritant should be evaluated for paradoxical vocal fold motion (intermittent laryngeal obstruction), as the condition may be triggered by just 1 episode of irritant exposure. The primary differentiating factor from irritable larynx syndrome is the report of irritant exposure.[39]
weak
competitive athletics
High-level competitive athletes with paradoxical vocal fold motion (intermittent laryngeal obstruction) (PVFM/ILO) have been described as female, highly competitive, success-oriented, and intolerant of failure, or as the child of similar-minded parents.[59] A retrospective study found almost one third of pediatric patients with PVFM/ILO competed at the highest level of a sport.[44]
anxiety
Adolescents with paradoxical vocal fold motion (intermittent laryngeal obstruction) (PVFM/ILO) and coexisting asthma have been found to experience more anxiety symptoms than those with isolated moderate to severe chronic asthma.[28] Individuals with PVFM/ILO also score highly for separation anxiety, a condition associated with panic attacks.[28]
Many studies have associated stressful environments and anxiety with occurrences of PVFM/ILO, and there is support for the presence of anxiety and, possibly, conversion disorder in the condition.[18][28][59][60][61]
muscle tension dysphonia
This voice disorder is characterized by excessive or poorly regulated activity of the intrinsic and extrinsic laryngeal muscles without structural or organic pathology.
Its etiology is multifactorial and includes laryngopharyngeal reflux.[62] It has been attributed to episodic laryngospasm and is identified in the inclusion criteria for irritable larynx syndrome.[35][Figure caption and citation for the preceding image starts]: Irritable larynx: bilateral erythema of the arytenoid complex bilaterally with tissue changes suggestive of early granulomaFrom the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].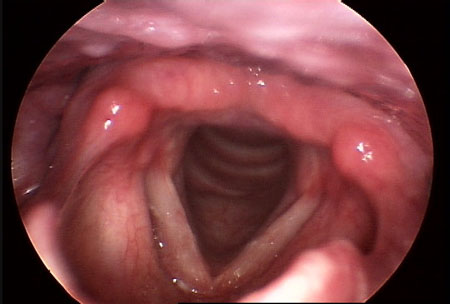
adductor laryngeal breathing dystonia
This condition is characterized by persistent inspiratory stridor with normal voice and cough.[63]
Use of this content is subject to our disclaimer