History and exam
Key diagnostic factors
common
visual field loss
Ubiquitous in patients with IIH. In some cases, the vision loss is mild and unlikely to be noticed by the patient.[38]
Other diagnostic factors
common
headache
transient visual obscurations
Episodes of transient visual loss usually last for <30 seconds and are followed by full restoration of vision. Visual obscurations occur in 68% of patients.[31] The episodes may be monocular or binocular. The cause of these episodes is thought to be transient ischemia of the optic nerve head, due to increased tissue pressure.[41]
pulse-synchronous tinnitus
Occurs in approximately 52% of patients and is a relatively specific symptom of increased intracranial pressure.[31] The sound is bilateral in two-thirds of patients and unilateral in one third.[31] In patients with intracranial hypertension, jugular compression ipsilateral to the sound abolishes it.[43]
photophobia
Usually a symptom associated with headache but has been reported independently of headache in a small number of patients.[39]
retrobulbar pain
Occurs in around half of patients, and pain with eye movements occurs in around 20% of patients.[38] However, this pain is usually milder than the pain associated with eye movements in people with optic neuritis.
optical disk swelling
Care must be taken to differentiate true papilledema from pseudopapilledema. Optic disk edema is the cause of the loss of vision in IIH. The higher the grade of papilledema, in general, the worse the visual outcome.[15] Severity of disk swelling is graded according to the Modified Frisén Scale.[37][44][Figure caption and citation for the preceding image starts]: Bilateral disk edemaFrom the personal collection of Dr M. Wall; used with permission [Citation ends].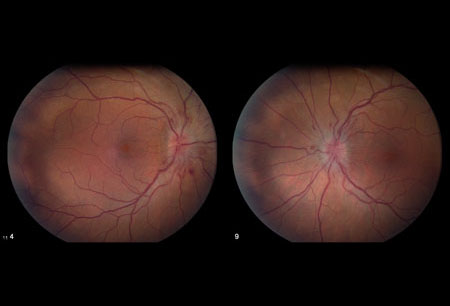 [Figure caption and citation for the preceding image starts]: Frisén stage IFrom the personal collection of Dr M. Wall; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Frisén stage IFrom the personal collection of Dr M. Wall; used with permission [Citation ends].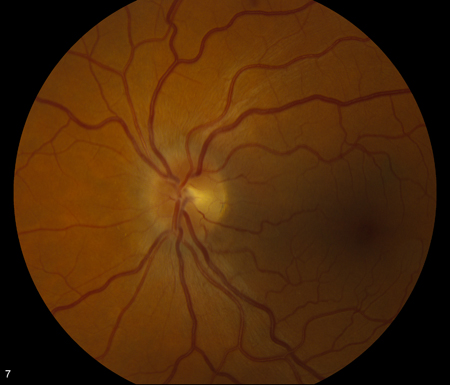 [Figure caption and citation for the preceding image starts]: Frisén stage IIFrom the personal collection of Dr M. Wall; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Frisén stage IIFrom the personal collection of Dr M. Wall; used with permission [Citation ends].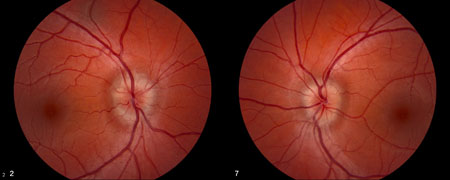 [Figure caption and citation for the preceding image starts]: Frisén stage IIIFrom the personal collection of Dr M. Wall; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Frisén stage IIIFrom the personal collection of Dr M. Wall; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Frisén stage IVFrom the personal collection of Dr M. Wall; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Frisén stage IVFrom the personal collection of Dr M. Wall; used with permission [Citation ends].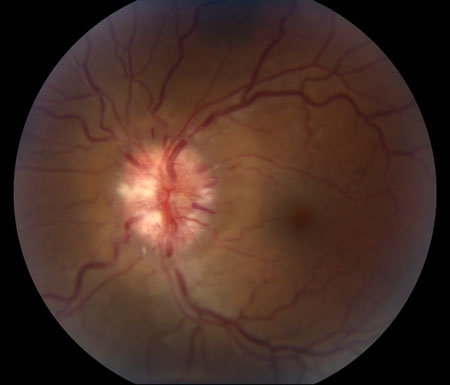 [Figure caption and citation for the preceding image starts]: Frisén stage VFrom the personal collection of Dr M. Wall; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Frisén stage VFrom the personal collection of Dr M. Wall; used with permission [Citation ends].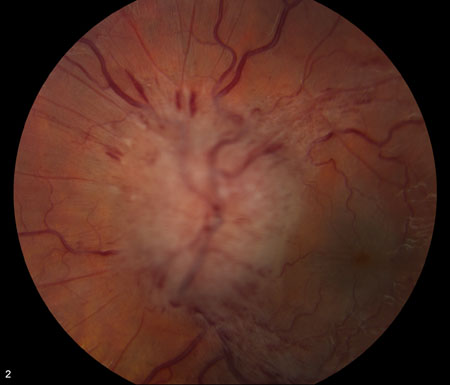
decreased visual acuity
Visual acuity usually is normal, or near normal, in patients with papilledema, except when the condition is long-standing and severe, or if there is a neurosensory detachment. Mild visual loss is common in patients with IIH, but Snellen testing is insensitive to the amount of visual loss found with perimetry and to worsening of the grade of papilledema.[38][54]
uncommon
ocular motility disturbances
Horizontal diplopia occurs in about 33% of patients, and sixth cranial nerve palsy/palsies occur in 10% to 20%.[38] Ocular motility disturbances other than sixth cranial nerve palsies are very rare, and if present suggest either a vertical ocular motor imbalance associated with the sixth nerve palsy or a diagnosis other than IIH.[1]
relative afferent pupillary defect
In one study, a relative afferent pupillary defect was found in 5.4% of eyes.[31]
Risk factors
strong
female sex
There is a female preponderance; incidence among females is estimated at 7.7 per 100,000, compared with 1.6 per 100,000 for males.[4]
obesity and weight gain
certain medication use
There is reasonable evidence that the following medications and conditions can cause increased intracranial pressure: nalidixic acid, nitrofurantoin, ketoprofen or indomethacin (in Bartter syndrome), vitamin A intoxication, isotretinoin, all-trans retinoic acid, thyroid replacement therapy in hypothyroid children, lithium, and anabolic steroids (which may cause venous sinus thrombosis).[17][18][19][20][21][22][23][24][25][26]
Although tetracycline or minocycline therapy might be a related cause, the common use of these medications, in conjunction with incomplete proof of the association, suggests that further study is needed.[27][28] Clinical differences between tetracycline-induced intracranial hypertension and IIH show a younger age, less frequent co-occurrence of obesity, and shorter mean illness duration.[29]
associated causal diseases
There are many associated causes of IIH, with varying strengths of association. One likely cause is decreased flow through arachnoid granulations, due to scarring from previous inflammation (e.g., meningitis, sequel to subarachnoid hemorrhage). Another is obstruction to venous drainage, which may result from venous sinus thromboses due to hypercoagulable states, contiguous infection (e.g., middle ear or mastoid-otitic hydrocephalus), bilateral radical neck dissections, superior vena cava syndrome, or increased right heart pressure. IIH may also be associated with endocrine conditions such as Addison disease, hypoparathyroidism, obesity, and corticosteroid withdrawal, and nutritional disorders such as hypervitaminosis A (vitamin, liver, or isotretinoin intake) and hyperalimentation in psychosocial short stature.
Other conditions that could be associated with IIH include systemic lupus erythematosus, uremia, iron deficiency anemia, sarcoidosis, arteriovenous malformations, and dural shunts.
weak
sleep apnea
IIH and sleep apnea often coexist. Whether there is a direct correlation is uncertain, although some studies have reported a high prevalence of sleep apnea in men with IIH. It is unclear whether the presence or treatment of comorbid sleep apnea affects the clinical course of IIH.[30]
Use of this content is subject to our disclaimer