Tests
1st tests to order
peripheral blood smear (Giemsa or Wright stained)
Test
Order in all patients with suspected disease for diagnostic confirmation.[6][31]
Manual review of blood smears should be requested explicitly. Multiple smears should be examined, as only a few RBCs may be infected during the initial stages of infection.[6]
Babesia may be confused with malarial parasites on blood smear (both appear as intraerythrocytic rings). Therefore, additional laboratory testing may be considered to confirm the diagnosis and identify the specific babesial pathogen.[6] Babesiosis and malaria have no geographic overlap, so the epidemiologic history of the patient is extremely important.
Test sensitivity depends on both the quality of the smear preparation and the training of the person interpreting the smear.[Figure caption and citation for the preceding image starts]: Thin blood smear, Babesia microti, with ring formsFrom the collection of Sarah Hochman, Albert Einstein College of Medicine; used with permission [Citation ends].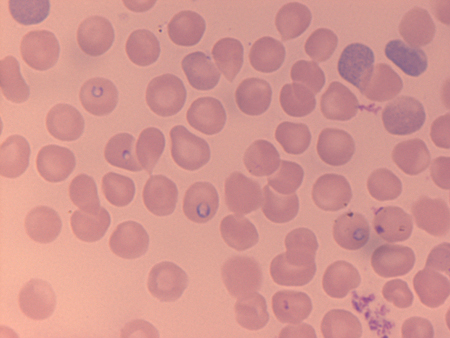 [Figure caption and citation for the preceding image starts]: Thin blood smear, Babesia microti, with triad form in centerFrom the collection of Sarah Hochman, Albert Einstein College of Medicine; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Thin blood smear, Babesia microti, with triad form in centerFrom the collection of Sarah Hochman, Albert Einstein College of Medicine; used with permission [Citation ends].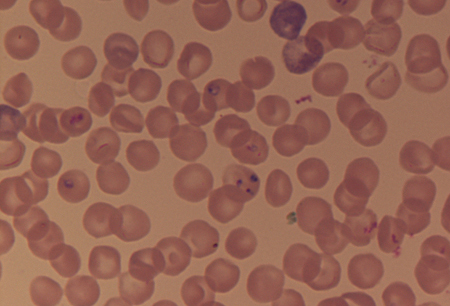
Result
presence of ring-like structures within RBCs
polymerase chain reaction for babesial DNA
Test
An alternative diagnostic confirmation option in patients with suspected babesiosis, when available.[6][31]
May be considered in patients with detectable ring-like structures on thin blood smear, to help differentiate from malaria, or for patients with no detectable ring forms on smear for whom clinical suspicion is high.[32][33]
Result
presence of Babesia microti DNA
CBC
Result
variable; leukopenia with low hematocrit; thrombocytopenia
LFTs
Test
Usually shows mildly to moderately elevated transaminases.[6]
Result
variable; transaminases may be elevated
serum creatinine and blood urea nitrogen (BUN)
Test
May be elevated in severe cases.[6]
Result
variable; may be elevated
urinalysis
Test
Presence of dark urine, with urobilinogen and conjugated bilirubin, may indicate hemolysis.
Result
variable; trace to moderate protein, urobilinogen and conjugated bilirubin may be found
ELISA and/or immunofluorescence assay for Lyme disease
Test
Excludes Lyme disease as the principal diagnosis.
Lyme disease should be included in the differential diagnosis of any patient who develops fever or clinical illness after tick bite.
Patients with confirmed babesiosis who remain symptomatic despite appropriate antibabesial therapy should also be tested for Lyme disease, as coinfection can occur and can worsen symptoms of babesiosis.
Specimens negative for Lyme disease by a sensitive ELISA or immunofluorescence assay need not be tested further.
Result
variable; typically negative; positive result may indicate coinfection
polymerase chain reaction and/or immunofluorescence assay or buffy coat smear for human granulocytic anaplasmosis
Test
Excludes human granulocytic anaplasmosis (HGA) as the principal diagnosis.
HGA should be included in the differential diagnosis of any patient who develops fever or clinical illness after tick bite.
Patients with confirmed babesiosis who remain symptomatic despite appropriate antibabesial therapy should be tested for HGA, as coinfection can occur and can worsen symptoms of babesiosis.
Anaplasma phagocytophilum may be detected as granulocytic inclusions on thin blood smear as well.
Result
variable; typically negative; positive result may indicate coinfection
Tests to consider
indirect immunofluorescence antibody assay for Babesia microti
Test
Can provide supportive evidence for the diagnosis, but does not reliably distinguish between active and prior infection.[6] The Infectious Diseases Society of America (IDSA) recommends peripheral blood smear examination or PCR for diagnostic confirmation of acute babesiosis, rather than antibody testing.[31]
A single positive antibody test is not sufficient to establish a diagnosis as Babesia antibodies can persist in the blood for a year or more following apparent clearance of infection (with or without treatment). Therefore, in patients who have a positive antibody test only, IDSA recommends confirmation with peripheral blood smear or PCR before treatment is considered.[31]
May be performed on acute and convalescent (4-6 weeks) serum samples, although many will have detectable antibodies at acute presentation.
An IgG titer ≥1:1024 or the presence of IgM indicates active or recent infection. A four-fold increase in IgG between acute and convalescent serum confirms the diagnosis.[31]
ELISA and immunoblot tests are also available but have limited use for diagnosis.[31]
Result
positive
IgG/IgM immunoblot for Lyme disease
Test
Only for patients with positive ELISA for Lyme disease.
Result
presence of bands signifying antibody to Borrelia burgdorferi
HIV serology
Test
Confirms or excludes HIV infection in patients with severe or prolonged disease. Results should be interpreted with caution as a case of false-positive HIV serology has been reported in a patient with active babesiosis.[35]
Result
variable
Use of this content is subject to our disclaimer