Tests
1st tests to order
culture and sensitivities of exudate from duct
Test
Culture of purulent discharge is advisable in acute presentations of sialadenitis, and antibiotic therapy should be targeted at causative organisms. If acute bacterial cause seems likely but culture is negative, it may be presumed to be anaerobic in nature. Presumptive antimicrobial therapy can be started while waiting for the results of culture and sensitivity.
Result
bacterial growth on culture indicates infection is present
CBC
Test
Indicated if infection is suspected. WBC count may also be elevated if infection is present elsewhere.
Result
elevated WBC count indicates the presence of infection
facial radiographs (occlusal and/or soft tissue films)
Test
Radiographic films should be requested for every patient who presents with acute sialadenitis. A small number of sialoliths may not be seen in plain films, owing to low calcium phosphate content. In this case, a CT is recommended.[Figure caption and citation for the preceding image starts]: Occlusal radiographic film showing presence of multiple sialoliths in the left Wharton ductFrom the personal collection of Dr A. Aguirre; used with permission [Citation ends].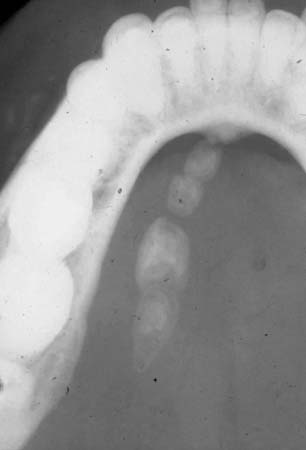
Result
sialoliths identified if present
Tests to consider
ultrasound of affected gland
Test
Indicated when abscess formation is suspected and when the clinical presentation is mild in order to limit radiation exposure to the patient. Ultrasound has an increased role in detection of IgG4-related sialadenitis with nodular features, smooth contour mass and hypoechoic foci.
Result
demonstrates a sialolith (>1 mm diameter) or fluid-filled abscess cavity if present
CT scan
Test
Indicated if conventional plain films are negative or when clinical presentation is severe. When ordering CT, consider concurrent sialography in nonacute patients. May also be useful, in addition to MRI, if neoplasia is suspected.
Result
will demonstrate presence of sialolith; atrophic or enlarged salivary glands in chronic sclerosing sialadenitis; may demonstrate presence of neoplasia
digital subtraction sialography
Test
Used in combination with CT when sialolithiasis, ductal strictures, or loss of parenchymal integrity is suspected (i.e., chronic sialadenitis). Acute inflammation is a relative contraindication.
Result
will demonstrate sialolith, ductal strictures, or loss of parenchymal integrity if present
MR sialography
Test
Three dimensional methods are preferred for detecting ductal stenoses and strictures.
Result
may enable visualization of ductal stenoses or strictures, and dilatation
scintigraphy using radioisotope sodium pertechnetate Tc-99m
Test
May be indicated when removal of a dysfunctional gland is being considered, such as in chronic sclerosing sialadenitis. It is of value in determining the degree of salivary gland hypofunction in Sjogren syndrome. May be used to assess function after treatment of obstructive sialadenitis or following radiotherapy.
Result
may show the presence of a hypo- or nonfunctional salivary gland
SSA/anti-Ro, SSB/anti-La antibodies
Test
Indicated to rule out Sjogren syndrome. If SSA and SSB negative, and Sjogren syndrome is still suspected, salivary gland biopsy is required.
Result
positive (pathognomonic of Sjogren syndrome)
antinuclear antibodies
Test
Elevated titers are suggestive of an autoimmune/connective tissue disorder.
Result
normal or elevated
rheumatoid factor
Test
Elevated titers are suggestive of an autoimmune/connective tissue disorder.
Result
normal or elevated
fine needle aspiration cytology of affected gland
Test
Chronic sclerosing sialadenitis can present in a similar fashion to a tumor; FNA is useful to exclude the presence of a neoplasm.
Result
no neoplastic change if chronic sclerosing sialadenitis is present
MRI
Test
May be required if neoplasia is suspected. Useful for delineating soft tissue changes.
Result
detects neoplastic change; demonstrates tumor size
minor salivary gland biopsy
Test
Between 5 and 8 minor salivary glands from the lower lip can be harvested for microscopic examination. Histopathology and microscopic examination may be necessary to distinguish chronic sialadenitis from neoplasms of glandular or other origin.
Subacute necrotizing sialadenitis can be identified by biopsy of the swelling on the hard palate to distinguish it from necrotizing sialometaplasia or malignancy.
Result
severe lymphocytic infiltrate of salivary gland parenchyma with loss of acinar structures and persistence of ducts with autoimmune etiology; glandular necrosis without squamous metaplasia in subacute necrotizing sialadenitis
IgG4 and IgE
Test
Diagnosis of IgG4-related sialadenitis involves combining the clinical features with elevated absolute serum IgG4 levels and an increased ratio of IgG4 to IgG plasma cells.
Result
IgG and IgG4 levels elevated in IgG4-related sialadenitis, elevated IgG4 to IgG ratio of greater than 50%, often with increased IgE. SSA/anti-Ro, SSB/anti-La antibodies usually absent.
major salivary gland biopsy
Test
IgG4-related sialadenitis diagnosis is based on biopsy of the affected gland primarily on elevated IgG4 to IgG ratio of greater than 50% and secondarily on increased number of IgG4 positive cells per high power field. Lower lip biopsy may be an alternative option.
Result
marked lymphoplasmacytic infiltration and fibrosis
sialoendoscopy
Test
A minimally invasive technique for the treatment and management of sialadenitis and obstructive salivary gland disease. Avoided in acute inflammation because of an increased risk of infection and duct perforation.[38] Sialendoscopy is an established technique though tends to be available in tertiary centers.
Result
visualization of sialoliths, anatomic malformations, polyps, foreign bodies, and ductal strictures
Use of this content is subject to our disclaimer