Approach
All patients presenting with evidence of infection and respiratory symptoms should undergo investigation for a parapneumonic effusion, especially those who fail to improve despite antibiotic treatment for pneumonia.[2]
The initial test of choice is a chest radiograph, and if the clinician is skilled with point-of-care ultrasound (POCUS) then this can also be used to help quantify and qualify the effusion.[8] If a significant effusion is seen, a diagnostic thoracentesis (pleural aspiration) with ultrasound guidance is required.[8] In patients where a complicated parapneumonic effusion or empyema is suspected, it is reasonable to pursue tube thoracostomy up front to help achieve source control and provide an avenue for continuous drainage and possible instillation of therapeutics.[8] Aspiration of frank pus is diagnostic of empyema, but if this is not present, further biochemical and microbiological tests are required to diagnose whether or not a parapneumonic effusion is complicated.
Clinical history
Presenting symptoms
The key presenting symptoms of empyema are breathlessness (secondary to large pleural effusion or pneumonia), fever, and pleuritic chest pain (pain worsened by deep breathing, coughing, sneezing, and chest movement). Other associated symptoms include those of pneumonia (productive cough, green or rust-colored sputum, shortness of breath) and systemic infection (anorexia, malaise, fatigue, rigors).
Patients tend to have a subacute history of illness, with a mean duration of symptoms before admission of 2 weeks.[23][24] Failure of patients with pneumonia to respond to antibiotics or a deterioration in clinical condition suggests the development of a complicated parapneumonic effusion or empyema.
The lack of characteristic clinical signs can delay diagnosis. Immunocompromised patients or patients who are already taking antibiotics may present with few clinical signs of infection. Patients with anaerobic empyemas can present with a more indolent illness characterized by weight loss, constitutional upset, and fatigue.
Past medical history
The majority of patients who develop empyema have a recent history of pneumonia, thoracic trauma, or iatrogenic intervention in the pleural space such as thoracic surgery, or medical procedures such as chest drain insertion (4%), thoracentesis (pleural aspiration), tube thoracostomy (chest drain insertion), and aspiration of pneumothoraces or pleural effusions.[3]
Patients may have a history of a medical condition predisposing them to the development of pneumonia and hence empyema, such as pre-existing lung diseases (e.g., bronchiectasis, COPD, lung cancer) or conditions associated with an increased risk of aspiration (e.g., stroke, presence of a nasogastric or endotracheal tube). Immunocompromised patients (e.g., due to hematologic disease, chemotherapy, HIV, or malnutrition) are also at increased risk of developing empyema.
Social history
Alcohol abuse and drug addiction are additional risk factors for the development of empyema.
Clinical exam
Examination reveals evidence of a pleural effusion with or without signs of systemic infection.
Large pleural effusions are characterized by dullness on percussion (classically described as "stony" in quality) and diminished breath sounds with reduced vocal resonance on the affected side. Smaller pleural effusions may not be detectable on clinical exam.
Septic shock presents with pyrexia, tachypnea, tachycardia, and hypotension (BP <90/60). Such patients require urgent resuscitation.
Blood tests
A complete blood count, C-reactive protein (CRP), and blood cultures should be undertaken in all patients with suspected empyema at presentation.[8] In empyema, the white blood cell count and the CRP will be raised as part of a systemic response to infection. Blood cultures may be positive for specific pathogens even if the pleural fluid culture is negative. Ideally, blood cultures should be taken before the initiation of antibiotics if the clinical state of the patient permits. Additionally, a basic metabolic panel including albumin and renal function tests can be obtained in order to help prognosticate patients at high risk for a poor outcome, using the RAPID (Renal [urea], Age, fluid Purulence, Infection source, Dietary [albumin]) clinical score.[18][25]
Initial imaging studies
The initial investigations of choice are chest x-ray and thoracic ultrasound, and should be undertaken in all patients with a suspected empyema at presentation.[8] Chest computed tomography (CT) should be reserved for complicated cases (e.g., children that fail to respond to treatment, or if there is doubt about the diagnosis).[26][27]
An urgent chest x-ray (CXR) should be organized in all patients who present with respiratory symptoms and evidence of sepsis, as it can demonstrate the presence of a pleural effusion. A lateral decubitus CXR is more sensitive than a posteroanterior view for detecting an effusion, but its use has been superseded by thoracic ultrasound given the ease of rapid use and ubiquitous nature of ultrasound. The presence of a loculated effusion suggests an empyema. Empyemas may have a pleurally based "D"-shaped appearance which can be mistaken for a lung mass. There may be associated pulmonary consolidation due to pneumonia and, in ventilated supine patients, a pleural effusion will appear as a diffuse unilateral increase in opacification. An effusion measuring >10 mm on a lateral decubitus CXR, in association with evidence of infection, requires thoracentesis (pleural aspiration).[1]
Thoracic ultrasound is more sensitive than a CXR for the detection of pleural effusions.[8] Features suggestive of an empyema on thoracic ultrasound include the presence of echogenic fluid, loculations, and septations, as shown below.[28][Figure caption and citation for the preceding image starts]: Ultrasound image of heavily septated empyemaFrom the collection of Najib Rahman, RTU, Oxford [Citation ends].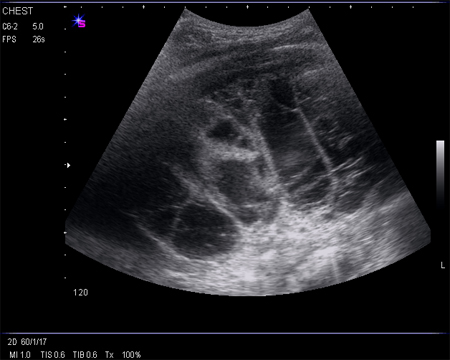 As empyemas are often associated with a raised hemidiaphragm or tethered lung, image guidance decreases complication rate substantially and so is preferred for all procedures. The use of ultrasound to guide thoracentesis (pleural aspiration) in order to reduce its associated complication rate is advised.[29] Ultrasonography is also recommended to guide chest drain insertion, especially in small or loculated effusions.[8]
As empyemas are often associated with a raised hemidiaphragm or tethered lung, image guidance decreases complication rate substantially and so is preferred for all procedures. The use of ultrasound to guide thoracentesis (pleural aspiration) in order to reduce its associated complication rate is advised.[29] Ultrasonography is also recommended to guide chest drain insertion, especially in small or loculated effusions.[8]
Thoracentesis
All patients with evidence of infection and a significant pleural effusion should undergo thoracentesis (pleural aspiration) with ultrasound guidance.[1][8][30]
Video demonstrating how to perform a pleural aspiration
Aspiration of frank pus is diagnostic of an empyema and no other investigations are required to establish the diagnosis, with the exception of pleural fluid microbiology to guide antibiotic therapy. If the aspirate does not reveal frank pus, further analysis is required to assess whether it is a complicated parapneumonic effusion. This involves measurement of the pleural fluid pH, total protein concentration, lactate dehydrogenase (LDH) level, glucose concentration, and white cell differential.
All samples should be sent for microscopy, culture, and sensitivity testing. Cytology may be used in cases where the diagnosis is unclear (e.g., for the detection of malignant cells in a malignant pleural effusion).
Pleural fluid appearance: Empyema is characterized by frank pus. Complicated parapneumonic effusions may be serous or cloudy. Use caution when interpreting fluid appearance, as infection can be present even in simple appearing fluid.
Pleural fluid odor: Putrid odor is suggestive of an anaerobic infection.
Pleural fluid pH: Samples should be stored anaerobically.[31] Local anesthetics can falsely lower the pH. Physicians should have access to a blood gas analyzer so that samples can be tested immediately to enable immediate insertion of a chest drain if indicated. If the sample is frank pus, the pH should not be tested as it can damage the analyzer.
Pleural fluid total protein concentration: If frank pus is aspirated, the protein concentration does not require analysis.[8][18]
Pleural fluid LDH level: If frank pus is aspirated, the LDH level does not require analysis.
Pleural fluid glucose concentration: If frank pus is aspirated, glucose does not require analysis. If an accurate pleural fluid pH is not available, low glucose levels can be used as an alternative predictor of a complicated parapneumonic effusion requiring urgent chest drain insertion. Pleural fluid glucose has been shown to be a robust predictor in this circumstance.[32]
Pleural fluid white cell differential: Polymorphonuclear leukocytes are the predominating (>90%) cell type. The predominance of lymphocytes in the exudate raises the suspicion of tuberculosis or malignancy.
Pleural fluid microscopy, culture, and sensitivity: A positive Gram stain or culture is obtained in 60% to 70% of samples.[23] This can be used to guide antibiotic treatment.
Further imaging studies
Further imaging studies are performed when there is doubt about the diagnosis or to confirm the correct position of the chest drain.[8]
Contrast-enhanced thoracic CT can help to distinguish empyema from other pleural effusions and lung abscesses, and should be done with tissue phase contrast.[33][Figure caption and citation for the preceding image starts]: CT scan of thoracic empyemaFrom the collection of Najib Rahman, RTU, Oxford [Citation ends].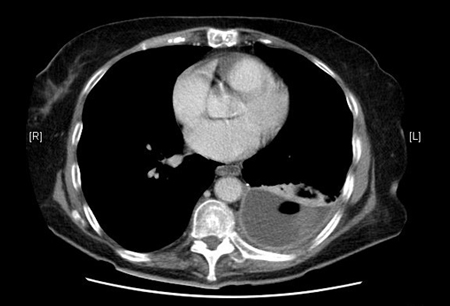 [Figure caption and citation for the preceding image starts]: CT scan of thoracic empyemaFrom the collection of Najib Rahman, RTU, Oxford [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan of thoracic empyemaFrom the collection of Najib Rahman, RTU, Oxford [Citation ends].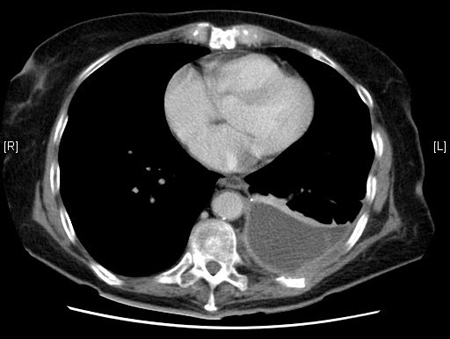 Enhancement of the pleura with contrast is characteristic of empyema. The split pleura sign represents enhancement of the visceral and parietal pleura with interposed fluid. Pleural thickening may be visible, but this is also seen in malignancy; therefore, using pretest probability of malignancy can help guide initial therapy. Contrast-enhanced thoracic CT is especially useful for confirmation of the correct positioning of the chest drain and may help in the planning of surgery.
Enhancement of the pleura with contrast is characteristic of empyema. The split pleura sign represents enhancement of the visceral and parietal pleura with interposed fluid. Pleural thickening may be visible, but this is also seen in malignancy; therefore, using pretest probability of malignancy can help guide initial therapy. Contrast-enhanced thoracic CT is especially useful for confirmation of the correct positioning of the chest drain and may help in the planning of surgery.
Magnetic resonance imaging is unable to accurately diagnose an empyema and is not routinely performed in the diagnosis or management of empyema. It is generally reserved for patients who are unable to undergo contrast-enhanced CT.[34] It may show septations, loculated pleural fluid, or chest wall invasion. [Figure caption and citation for the preceding image starts]: MRI scan of septated empyemaFrom the collection of Najib Rahman, RTU, Oxford [Citation ends].
A positron emission tomography scan is another possible imaging technique, but its use is limited by the fact that it is unable to distinguish between malignancy and empyema.[35] It is generally not performed in the diagnosis or management of empyema.[8]
As the causative organism in 40% of pleural infections remains unidentified, pleural fluid polymerase chain reaction may aid pathogen identification, allowing specific antibiotics to be chosen.[23] However, further prospective evidence is required on this technique before it can be routinely recommended.
Use of this content is subject to our disclaimer
