Aetiology
Aetiology is any blow to the head that meets the diagnostic criteria for mild traumatic brain injury.[5][7][18] The injury to the head results in bio-mechanical forces contorting the brain. Brain rotation occurs because the head is attached to the neck, on which it pivots when struck or during rapid deceleration. Movement of the brain within the skull is constrained by the falx and anchor points along the skull base and as such, selected areas are subject to high strain forces.[19] These areas, which include the corpus callosum, internal capsule, and fornix, are most likely to undergo axonal injury after a mild traumatic brain injury.[20]
The most common causes of a mild traumatic brain injury include:[21]
Motor vehicle accidents
Being struck by or against objects, e.g., during sports and recreational activities (frequency varies across lifespan)
Assaults (frequency varies across lifespan)
Falls (frequency varies across lifespan).
Pathophysiology
Studies indicate that mild traumatic brain injuries can result in structural changes detectable on computed tomography or structural magnetic resonance imaging (MRI). Structural traumatic abnormalities are seen on MRI in up in approximately 30% of patients with mild TBI who had a normal CT on presentation.[22][23] The most common structural changes observed are cerebral contusions, and less common observations include epidural haematomas, subdural haematomas, and axonal injury.
[Figure caption and citation for the preceding image starts]: Sites of contusions and epidural haematomas: (A) pre-frontal cortex, (B) pterion, (C) temporal-parietal cortex (often during contre-coup)From the collection of L. Henry; used with permission [Citation ends].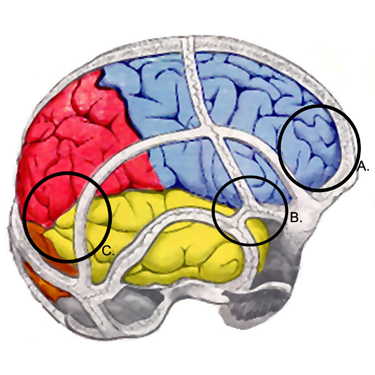 Techniques such as MRI volumetry suggest that mild traumatic brain injury may lead to global brain atrophy.[24][25]
Techniques such as MRI volumetry suggest that mild traumatic brain injury may lead to global brain atrophy.[24][25]
The biochemical cascade is marked by an initial period of indiscriminate neurotransmitter release and unchecked ionic fluxes.[26] Excitatory neurotransmitters, such as glutamate, bind to N-methyl-D-aspartate receptors leading to further neuronal depolarisation with the influx of calcium and the efflux of potassium. These ionic shifts lead to acute and subacute changes in cellular metabolism and physiology. Acutely, the sodium-potassium pump works overtime to restore a homeostatic balance, requiring increasing amounts of adenosine triphosphate and a corresponding increase in glucose metabolism. This hypermetabolic state co-occurs with diminished cerebral blood flow. The disparity in energy balance and the tendency to restore ionic balance is met with the decrease in blood flow, creating a cellular energy crisis that is suspected to be the mechanism for post-injury vulnerability, leaving the brain more vulnerable to a second injury and potentially longer-lasting, more severe deficits. After this initial period of hypermetabolism, the brain goes into a state of hypometabolism where the persistent increase of calcium may be responsible for impairing mitochondria, further affecting cellular metabolism and neural integrity, worsening the energy crisis, and potentially affecting post-traumatic neural connectivity.[26]
Axonal compression and stretching is also thought to be a major injury mechanism, creating a focal abnormality on the surface membrane of the axon within hours of injury, sufficient to impair axoplasmic transport, resulting in oedema. The swollen axon then separates, with the proximal section remaining attached to the cell body while the distal end undergoes phagocytosis by neighbouring glial cells. Axonal swellings may persist unchanged, or regeneration may occur over several weeks. If axons do not regenerate, reactive deafferentation may occur.[27]
Neuro-imaging studies using functional MRI suggest that a depressed mood after a mild traumatic brain injury may reflect an underlying pathophysiological abnormality consistent with a limbic-frontal model of depression.[27][28]
Classification
Injury severity classification of mild traumatic brain injury[5][6]
Criteria used to classify mild traumatic brain injury include:
Structural imaging: normal
Loss of consciousness <30 minutes
Post-traumatic amnesia: 0 to 1 day
Glasgow Coma Scale score: 13 to 15
Abbreviated Injury Scale score (head): 1 to 2.
2022 Concussion in Sport Group consensus statement[7]
Several common features may be utilised in clinically defining the nature of a sport-related concussive head injury:
A traumatic brain injury caused by a direct blow to the head, neck, or body resulting in an impulsive force being transmitted to the brain that occurs in sports and exercise-related activities.
A range of clinical symptoms and signs that may or may not involve loss of consciousness.
Symptoms and signs which may present immediately, or evolve over minutes or hours, and commonly resolve within days, but may be prolonged.
No abnormality seen on standard structural neuroimaging studies (computed tomography or magnetic resonance imaging T1- and T2-weighted images); in the research setting, abnormalities may be present on functional, blood flow, or metabolic imaging studies.
Use of this content is subject to our disclaimer