Approach
Patients can present with ocular irritation, burning, and tearing due to local inflammation and tear film disturbances or loss of epithelium overlying the pterygium. Patients may also present due to impaired ocular cosmesis. Others may have impaired vision (due to irregular astigmatism and occasional progressive growth of the pterygium to the visual axis/centre of cornea).[13][14] Rarely, double vision may be the presenting complaint, caused by tethering of the medial rectus.
Typically, there is a history of excessive, chronic ultraviolet light exposure (e.g., outdoor occupations, surfers, sailors, residency within 40° of latitude of the equator).[1][2]
Pterygia are easily diagnosed by ocular examination. Pterygia appear as triangular-shaped, fibrovascular, conjunctival overgrowths onto the corneal surface. They occur in the interpalpebral region usually from the nasal side and are not uncommonly bilateral.[15] They consist of a cap of a sub-epithelial arc-shaped corneal opacity at the leading edge with a sub-epithelial brownish line of iron deposition known as Stocker's line, a head (white fibrous mass attached to cornea), and a body (fleshy, triangular-shaped fibrovascular tissue continuous with the conjunctiva at its base).
Slit-lamp examination facilitates thorough assessment of the ocular surface and allows accurate measurement of the nature and extent of the pterygia and detection of any other ocular surface anomalies.
Fluorescein staining of the tear film allows assessment of associated tear film anomalies.[Figure caption and citation for the preceding image starts]: Pterygium: A) cap, B) head, C) bodyFrom personal collection of David O'Brart; used with permission [Citation ends].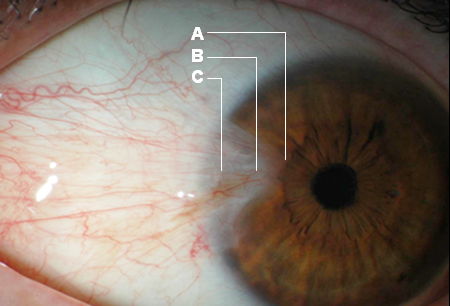
If astigmatism is suspected, further evaluation needs to be carried out, including corneal topography. See Astigmatism.
Use of this content is subject to our disclaimer