Approach
Clinical examination is not useful in establishing a diagnosis. Echo and, in particular, trans-oesophageal echo (TOE) form the cornerstone of diagnosis. [Figure caption and citation for the preceding image starts]: Trans-oesophageal echo showing a 2D image of the interatrial septum with location of the PFOFrom the collection of Kul Aggarwal, MD [Citation ends].
History and physical examination
The majority of patients are completely asymptomatic and no abnormal physical findings are associated. Suspicion of PFO is increased if a patient younger than 60 years presents with:
A cryptogenic stroke
A sudden onset of cold and pain in a limb
No obvious source of embolism.
A high index of suspicion is more likely to lead to a diagnosis. In patients with other obvious causes of a stroke, such as atrial fibrillation, aortic disease, or severe carotid artery disease, detection of a PFO is less useful, as it is unlikely to change management. Due to the presence of multiple variables that could contribute to an embolic stroke, a multi-disciplinary approach - with neurology and cardiology teams - is warranted to identify patient subsets where the presence of PFO could contribute to the embolic phenomenon and benefit from PFO closure procedure.
Patients with a decompression syndrome can also present with mild-to-severe manifestation due to the presence of PFO. Decompression syndrome is most often associated with a change of pressure from deep sea diving. A similar phenomenon and potential risk with PFO has been reported with high elevation flying, but it is not a well-established phenomenon.
Rarely, migraine headaches may indicate the presence of PFO.
A history of congenital heart disease (e.g., Ebstein anomaly) increases the likelihood of PFO and a high index of suspicion is warranted in divers with a history of decompression illness.
Dyspnoea associated with postural change (worse when the patient is upright; improves when the patient is recumbent) may be a clue to a PFO and platypnoea-orthodeoxia syndrome.
On cardiac examination, splitting of the second heart sound and a systolic murmur (sometimes fixed) are found in secundum atrial septal defect (ASD).
Echocardiography
Echocardiography is the principal modality used in the comprehensive evaluation of a PFO.[16] A transthoracic echo, paying careful attention to the interatrial septum, may serve as a screening test in suspected cases; however, the more invasive TOE is the method of choice. TOE is favoured due to the following factors:
more sensitive and specific in the detection of a PFO
Better visualisation
Allows differentiation of a PFO from an ASD
Decreases the rate of missed PFOs.
TOE is also very useful in the thorough evaluation of a PFO prior to device closure.[17]
Intracardiac echo is reserved for use during percutaneous closure of a PFO due to its high cost and invasive nature.
Colour flow Doppler imaging shows colour flow across the small defect in the interatrial septum. This flow is typically right to left but could sometimes be left to right or bidirectional. Intravenous injection of agitated saline with provocative manoeuvres (e.g., Valsalva and coughing) to increase right atrial pressure is utilised to evaluate for right to left crossover of microbubbles. Excessive mobility of the interatrial septum or presence of an atrial septal aneurysm indicates a PFO.[Figure caption and citation for the preceding image starts]: Trans-oesophageal echo showing a 2D image of the interatrial septum with location of the PFOFrom the collection of Kul Aggarwal, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Intracardiac echo showing a catheter placed across the PFO into the left atriumFrom the collection of Kul Aggarwal, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Intracardiac echo showing a catheter placed across the PFO into the left atriumFrom the collection of Kul Aggarwal, MD [Citation ends].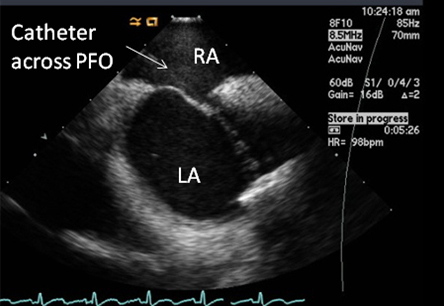 [Figure caption and citation for the preceding image starts]: Trans-oesophageal echo with intravenous injection of agitated saline showing contrast crossing through PFO into left atriumFrom the collection of Kul Aggarwal, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Trans-oesophageal echo with intravenous injection of agitated saline showing contrast crossing through PFO into left atriumFrom the collection of Kul Aggarwal, MD [Citation ends].
Other imaging modalities
Less commonly utilised, a transcranial Doppler may be performed to diagnose shunting through a PFO.[18] Although it is sensitive in the detection of abnormal flow, it does not actually visualise the PFO defect and therefore could produce a false positive.
Magnetic resonance imaging (MRI) and computed tomography (CT) scanning have not yet been demonstrated as useful in everyday diagnosis but may serve as important modalities for diagnosing ASDs. Imaging of the lower extremity with ultrasound or MRI may aid in the diagnosis of deep vein thrombosis and the overall diagnosis of paradoxical embolism and PFO.
Platypnoea-orthodeoxia syndrome
Diagnosis of platypnoea-orthodeoxia syndrome is best made by tilt-table TOE. The PFO is established as causative if an inserted TOE probe shows a significant amount of right-to-left shunting across the PFO resulting in hypoxaemia in an upright position, and if there is a resolution of shunting and hypoxaemia when the patient is in the recumbent position.
Use of this content is subject to our disclaimer