It is important to detect neck pain caused by significant causes (e.g., primary or metastatic cancer) and neck pain associated with neurological compromise. The diagnostic approach to neck pain has not been as well studied as back pain, but a similar approach is recommended.
Traumatic neck pain: initial evaluation and imaging
The risk for cervical spine injury needs to be assessed in patients presenting acutely with neck pain following trauma. The presenting clinical features and mechanism of injury should be considered when assessing risk for cervical spine injury. High risk criteria include the following:[34]American College of Radiology. ACR appropriateness criteria: acute spinal trauma. 2024 [internet publication].
https://acsearch.acr.org/docs/69359/Narrative
[50]Stiell IG, Clement CM, McKnight RD, et al. The Canadian C-spine rule versus the NEXUS low-risk criteria in patients with trauma. N Engl J Med. 2003 Dec 25;349(26):2510-8.
https://www.nejm.org/doi/full/10.1056/NEJMoa031375
http://www.ncbi.nlm.nih.gov/pubmed/14695411?tool=bestpractice.com
[51]Vandemark RM. Radiology of the cervical spine in trauma patients: practice pitfalls and recommendations for improving efficiency and communication. AJR Am J Roentgenol. 1990 Sep;155(3):465-72.
https://www.ajronline.org/doi/abs/10.2214/ajr.155.3.2117342
http://www.ncbi.nlm.nih.gov/pubmed/2117342?tool=bestpractice.com
Age >65 years
Paraesthesias in extremities
Altered mental status
Multiple fractures
Drowning or diving accident
Significant head or facial injury
"Dangerous mechanism", defined as: a fall from an elevation of 90 cm (3 feet ) or more, or 5 stairs; axial load to the head (e.g., diving); motor vehicle collision at high speed (>100 km/h or >60 mph) or with rollover or ejection; collision involving a motorised recreational vehicle; or a bicycle collision.
Immobilisation of the cervical spine must be maintained in all patients with suspected cervical spine injury until cleared either clinically or radiologically. In trauma patients who have their necks stabilised with a cervical collar, hypotension, tachycardia, and hypoxia are signs of significant trauma and should be assessed thoroughly.
Screening imaging must be done before any neck movement exam (e.g., range of motion). A cervical spine computed tomography (CT) scan is the study of choice for suspected cervical spine injury in the setting of multi-system trauma or with a high-risk mechanism.[34]American College of Radiology. ACR appropriateness criteria: acute spinal trauma. 2024 [internet publication].
https://acsearch.acr.org/docs/69359/Narrative
[41]Cain GS, Shepherdson J, Elliott V, et al. Imaging suspected cervical spine injury: plain radiography or computed tomography? systematic review. Radiography. 2010;16(1):68-77.
https://www.sciencedirect.com/science/article/abs/pii/S1078817409000698
[52]National Institute for Health and Care Excellence. Head injury: assessment and early management. May 2023 [internet publication].
https://www.nice.org.uk/guidance/ng232
Cervical magnetic resonance imaging (MRI) should be ordered in addition to cervical CT scan when ligamentous injury is suspected, or if neurological signs and symptoms referable to the cervical spine are present.[34]American College of Radiology. ACR appropriateness criteria: acute spinal trauma. 2024 [internet publication].
https://acsearch.acr.org/docs/69359/Narrative
[52]National Institute for Health and Care Excellence. Head injury: assessment and early management. May 2023 [internet publication].
https://www.nice.org.uk/guidance/ng232
[53]Schoenfeld AJ, Bono CM, McGuire KJ, et al. Computed tomography alone versus computed tomography and magnetic resonance imaging in the identification of occult injuries to the cervical spine: a meta-analysis. J Trauma. 2010 Jan;68(1):109-13;discussion 113-4.
http://www.ncbi.nlm.nih.gov/pubmed/20065765?tool=bestpractice.com
Guidelines advise that cervical spine CT scan alone can be used to exclude cervical spine injuries in obtunded or intubated patients without neurological evidence to the contrary.[54]Plumb JOM. Clinical review: Spinal imaging for the adult obtunded blunt trauma patient: update from 2004. Intensive Care Med. 2012 May;38(5):752-71.
http://www.ncbi.nlm.nih.gov/pubmed/22407141?tool=bestpractice.com
[55]Panczykowski DM, Tomycz ND, Okonkwo DO, et al. Comparative effectiveness of using computed tomography alone to exclude cervical spine injuries in obtunded or intubated patients: meta-analysis of 14,327 patients with blunt trauma. J Neurosurg. 2011 Sep;115(3):541-9.
http://www.ncbi.nlm.nih.gov/pubmed/21619408?tool=bestpractice.com
[56]British Orthopaedic Association. BOAST - cervical spine clearance in the trauma patient. May 2021 [internet publication].
https://www.boa.ac.uk/resource/boast-cervical-spine-clearance-in-the-trauma-patient.html
Cervical spine x-rays may be performed in patients rather than CT scan following trauma when the injury is less severe, high risk criteria are not met, and there are no other features making examination findings less reliable (e.g., alcohol intoxication, painful distracting injuries). No further imaging is required in the following cases:[41]Cain GS, Shepherdson J, Elliott V, et al. Imaging suspected cervical spine injury: plain radiography or computed tomography? systematic review. Radiography. 2010;16(1):68-77.
https://www.sciencedirect.com/science/article/abs/pii/S1078817409000698
Clinical decision rules have been proposed to help physicians working in emergency care settings be more selective about when to use cervical spine radiography to assess alert and stable trauma patients.
Canadian C-spine rule
Applied in less severely injured patients, and may eliminate the need for any radiography. The rule must be properly applied and it does not pertain to a patient over the age of 65.[57]Stiell IG, Wells GA, Vandemheen KL, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001 Oct 17;286(15):1841-8.
https://jama.ama-assn.org/cgi/content/full/286/15/1841
http://www.ncbi.nlm.nih.gov/pubmed/11597285?tool=bestpractice.com
There is insufficient evidence to determine whether it can be used safely in children.[58]Tavender E, Eapen N, Wang J, et al. Triage tools for detecting cervical spine injury in paediatric trauma patients. Cochrane Database Syst Rev. 2024 Mar 22;3(3):CD011686.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011686.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/38517085?tool=bestpractice.com
The Canadian C-spine rule comprises 3 sets of questions:
Is there any high-risk factor present that mandates radiography (i.e., age ≥65 years, dangerous mechanism, or paraesthesias in extremities)?
Is there any low-risk factor present that allows safe assessment of range of motion (i.e., simple rear-end motor vehicle collision, sitting position in accident and emergency department, ambulatory at any time since injury, delayed onset of neck pain, or absence of midline C-spine tenderness?
Is the patient able to actively rotate neck 45° to the left and right?
Imaging is indicated for any trauma patient identified by the Canadian C-spine rule as having:
a high-risk factor for cervical spine injury or
a low-risk factor for cervical spine injury, and they are unable to actively rotate their neck 45° to both left and right.
NEXUS criteria
Intended to help physicians identify which patients need cervical spine radiography following blunt trauma. Five criteria must be met in order for the patient to be classified as having a low risk of cervical spine injury, as follows:[59]Hoffman JR, Mower WR, Wolfson AB, et al. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000 Jul 13;343(2):94-9.
https://www.nejm.org/doi/10.1056/NEJM200007133430203?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dwww.ncbi.nlm.nih.gov
http://www.ncbi.nlm.nih.gov/pubmed/10891516?tool=bestpractice.com
No tenderness at the posterior midline of the cervical spine
No focal neurological deficit
Normal level of alertness
No evidence of intoxication
No clinically apparent, painful injury that might distract the patient from the pain of a cervical spine injury.
Evidence from some retrospective studies suggests there is a risk of false-negative results when using the NEXUS criteria alone in children.[58]Tavender E, Eapen N, Wang J, et al. Triage tools for detecting cervical spine injury in paediatric trauma patients. Cochrane Database Syst Rev. 2024 Mar 22;3(3):CD011686.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011686.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/38517085?tool=bestpractice.com
Further evidence is needed to determine whether it is an appropriate tool for the clearance of cervical spine following blunt trauma in paediatric trauma care.
Non-traumatic neck pain: clinical features of concern
The presentation of a patient with neck pain with no history of trauma can vary considerably, and the pain may be acute or chronic in nature. It is important to be aware of features that increase the risk of a more ominous cause.
Fever in a patient with new neck pain
In these patients, neck pain should be assumed to be secondary to an infection until proven otherwise.
Patients with an infectious cause may be hypotensive or tachycardic.
There may be a history of recent infection (especially skin or urinary tract), immune compromise, or intervention associated with infection, such as surgery, trauma, or intravenous (IV) drug use.
Cervical osteomyelitis and cervical epidural abscesses arise from haematogenous spread in most cases. About one third of cases of cervical epidural abscesses arise from contiguous spread from the skin.[24]Darouiche RO. Spinal epidural abscess. N Engl J Med. 2006 Nov 9;355(19):2012-20.
http://www.ncbi.nlm.nih.gov/pubmed/17093252?tool=bestpractice.com
The most common symptoms are pain, fever, and neurological compromise.
Patients with meningitis may also have nuchal rigidity.
A history of, or symptoms suggestive of, cancer
In a patient with a history of cancer, the aetiology of neck pain should be assumed to be from cancer until this is ruled out.
Cancers that may cause neck pain include pharyngeal cancer and those that are more likely to metastasise to the cervical spine, such as thyroid cancer.
Tumour-related neck pain is more commonly unrelenting pain that is often worse at night (this symptom is unusual in most other causes of neck pain).[23]Abdu WA, Provencher M. Primary bone and metastatic tumors of the cervical spine. Spine (Phila Pa 1976). 1998 Dec 15;23(24):2767-77.
http://www.ncbi.nlm.nih.gov/pubmed/9879102?tool=bestpractice.com
Other signs and symptoms of cancer include unexplained weight loss, fatigue, or an unusual lump or swelling.
Neurological symptoms or deficits
Investigations should be expedited in patients presenting with pain radiating from the neck into the arm, numbness in the arms, weakness, loss of coordination, changes in gait, and change in bowel or bladder function. All are indicative of possible neurological compromise.
Symptoms suggestive of stroke or transient ischaemic attack could indicate cervical artery dissection.
Ipsilateral headache, eye pain, Horner’s syndrome, cranial nerve palsies, hemiplegia, hemisensory loss, neglect, and homonymous hemianopia can occur in carotid artery dissection, while vertigo, ataxia, dysarthria, and headache can occur in cases of vertebral artery dissection.[32]Gottesman RF, Sharma P, Robinson KA, et al. Clinical characteristics of symptomatic vertebral artery dissection: a systematic review. Neurologist. 2012 Sep;18(5):245-54.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3898434
http://www.ncbi.nlm.nih.gov/pubmed/22931728?tool=bestpractice.com
Non-traumatic neck pain: further history
Occupational history should be considered. Neck pain is prevalent among workers in the construction industry and in the agricultural sector.[60]Umer W, Antwi-Afari MF, Li H, et al. The prevalence of musculoskeletal symptoms in the construction industry: a systematic review and meta-analysis. Int Arch Occup Environ Health. 2018 Feb;91(2):125-44.
http://www.ncbi.nlm.nih.gov/pubmed/29090335?tool=bestpractice.com
[61]Jackson JA, Liv P, Sayed-Noor AS, et al. Risk factors for surgically treated cervical spondylosis in male construction workers: a 20-year prospective study. Spine J. 2023 Jan;23(1):136-45.
https://www.thespinejournalonline.com/article/S1529-9430(22)00872-5/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/36028215?tool=bestpractice.com
[62]Czępińska A, Zawadka M, Wójcik-Załuska A, et al. Association between pain intensity, neck disability index, and working conditions among women employed in horticulture. Ann Agric Environ Med. 2023 Sep 28;30(3):531-5.
https://www.aaem.pl/Association-between-pain-intensity-neck-disability-index-and-working-conditions-among,162028,0,2.html
http://www.ncbi.nlm.nih.gov/pubmed/37772530?tool=bestpractice.com
[63]Fethke NB, Merlino LA, Gerr F, et al. Musculoskeletal pain among Midwest farmers and associations with agricultural activities. Am J Ind Med. 2015 Mar;58(3):319-30.
http://www.ncbi.nlm.nih.gov/pubmed/25345841?tool=bestpractice.com
[64]Scutter S, Türker KS, Hall R. Headaches and neck pain in farmers. Aust J Rural Health. 1997 Feb;5(1):2-5.
http://www.ncbi.nlm.nih.gov/pubmed/9437926?tool=bestpractice.com
Office workers and computer users are also at risk for neck pain.[65]Ye S, Jing Q, Wei C, et al. Risk factors of non-specific neck pain and low back pain in computer-using office workers in China: a cross-sectional study. BMJ Open. 2017 Apr 11;7(4):e014914.
https://bmjopen.bmj.com/content/7/4/e014914
http://www.ncbi.nlm.nih.gov/pubmed/28404613?tool=bestpractice.com
[66]Côté P, van der Velde G, Cassidy JD, et al. The burden and determinants of neck pain in workers: results of the Bone and Joint Decade 2000-2010 Task Force on neck pain and its associated disorders. Spine (Phila Pa 1976). 2008 Feb 15;33(4 suppl):S60-74.
https://journals.lww.com/spinejournal/fulltext/2008/02151/the_burden_and_determinants_of_neck_pain_in.11.aspx
http://www.ncbi.nlm.nih.gov/pubmed/18204402?tool=bestpractice.com
[67]Mazaheri-Tehrani S, Arefian M, Abhari AP, et al. Sedentary behavior and neck pain in adults: a systematic review and meta-analysis. Prev Med. 2023 Oct;175:107711.
http://www.ncbi.nlm.nih.gov/pubmed/37775083?tool=bestpractice.com
A history of mental stress, perceived inadequacy, and previous injury has been found to be associated with neck pain. Psychological and psychosocial factors, such as anxiety, catastrophising, hypervigilance, and limited health literacy, may be important in predicting those who will go on to develop chronic neck pain.[9]Kazeminasab S, Nejadghaderi SA, Amiri P, et al. Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord. 2022 Jan 3;23(1):26.
https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-021-04957-4
http://www.ncbi.nlm.nih.gov/pubmed/34980079?tool=bestpractice.com
[68]Verwoerd M, Wittink H, Maissan F, et al. Consensus of potential modifiable prognostic factors for persistent pain after a first episode of nonspecific idiopathic, non-traumatic neck pain: results of nominal group and Delphi technique approach. BMC Musculoskelet Disord. 2020 Oct 7;21(1):656.
https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-020-03682-8
http://www.ncbi.nlm.nih.gov/pubmed/33028268?tool=bestpractice.com
These factors may also lead to decreased compliance with exercise secondary to concern over injury or worsening the injury.[69]van der Donk J, Schouten JS, Passchier J, et al. The associations of neck pain with radiological abnormalities of the cervical spine and personality traits in a general population. J Rheumatol. 1991 Dec;18(12):1884-9.
http://www.ncbi.nlm.nih.gov/pubmed/1795327?tool=bestpractice.com
[70]Makela M, Heiliovaara M, Sievers K, et al. Prevalence, determinants, and consequences of chronic neck pain in Finland. Am J Epidemiol. 1991 Dec 1;134(11):1356-67.
http://www.ncbi.nlm.nih.gov/pubmed/1755449?tool=bestpractice.com
A previous history of injury, such as whiplash injury, may predispose to cervical facet syndrome.[71]Schofferman J, Bogduk N, Slosar P. Chronic whiplash and whiplash-associated disorders: an evidence-based approach. J Am Acad Orthop Surg. 2007 Oct;15(10):596-606.
http://www.ncbi.nlm.nih.gov/pubmed/17916783?tool=bestpractice.com
Patients with neck pain secondary to rheumatoid arthritis have often had the diagnosis of rheumatoid arthritis for several years by the time cervical spine involvement presents.[72]van Eijk IC, Nielen MM, van Soesbergen RM, et al. Cervical spine involvement is rare in early arthritis. Ann Rheum Dis. 2006 Jul;65(7):973-4.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1798217/?tool=pubmed
http://www.ncbi.nlm.nih.gov/pubmed/16769788?tool=bestpractice.com
Neck pain typically radiates upward to the head.
Non-traumatic neck pain: physical exam
Neck examination:
Includes assessment of outward appearance, palpation for tenderness, and assessment of range of motion (ROM).[Figure caption and citation for the preceding image starts]: Patient with severe left torticollis (note hypertrophy of right sternocleidomastoid muscle)From the personal collection of David B. Sommer, MD, MPH [Citation ends].
In general, abnormal appearance, abnormal ROM, and a tender cervical spine are non-specific and indicate only that there is cervical spine disease, not a specific cause.
Apart from other systemic signs, patients with meningitis may have nuchal rigidity.[26]National Institute for Health and Care Excellence. Meningitis (bacterial) and meningococcal disease: recognition, diagnosis and management. Mar 2024 [internet publication].
https://www.nice.org.uk/guidance/ng240
[35]Durand ML, Calderwood SB, Weber DJ, et al. Acute bacterial meningitis in adults: a review of 493 episodes. N Engl J Med. 1993 Jan 7;328(1):21-8.
https://www.nejm.org/doi/full/10.1056/NEJM199301073280104#t=article
http://www.ncbi.nlm.nih.gov/pubmed/8416268?tool=bestpractice.com
This is demonstrated by the inability of the patient to touch his/her chin to the chest with passive or active flexion of the neck. Kernig's sign (painful/resisted extension of leg bent at hip and knee) and Brudzinski's sign (reflective flexion of the knees when patient is on his/her back and the neck is bent forwards) are tests used to demonstrate nuchal rigidity. The sensitivity and negative predictive value of Kernig's and Brudzinski's sign is low in the diagnosis of meningitis.[27]van de Beek D, Cabellos C, Dzupova O, et al. ESCMID guideline: diagnosis and treatment of acute bacterial meningitis. Clin Microbiol Infect. 2016 May;22 Suppl 3:S37-62.
https://www.clinicalmicrobiologyandinfection.com/article/S1198-743X(16)00020-3/fulltext
Examination of the upper extremities:
Neurological exam:
Includes careful evaluation for evidence of any:
decrease in sensation or strength, or abnormal reflexes, in the upper extremities
increased tone or spasticity, and abnormal reflexes, in the lower extremities.
Abnormal reflex responses include:
hyperreflexia or positive Babinski sign (hallux dorsiflexes with other toes fanning out)
positive Hoffman’s sign (involuntary flexion and adduction of the thumb and flexion of the index finger when the nail of the middle finger is flicked downwards), or
positive clonus (a rhythmic, oscillating, stretch reflex in response to rapid dorsiflexion of the ankle).
The hallmark clinical manifestations of cervical radiculopathies are pain, sensory loss, and motor weakness in the distribution of the affected nerve root.[73]Polston DW. Cervical radiculopathy. Neurol Clin. 2007 May;25(2):373-85.
http://www.ncbi.nlm.nih.gov/pubmed/17445734?tool=bestpractice.com
The most commonly affected nerve roots are C7 (50% to 70%), C6 (>20%), C8 (10%), and C5 (2% to 10%).[73]Polston DW. Cervical radiculopathy. Neurol Clin. 2007 May;25(2):373-85.
http://www.ncbi.nlm.nih.gov/pubmed/17445734?tool=bestpractice.com
Patients with rheumatoid arthritis may present with uncomplicated neck pain, which may progress to myelopathy due to cervical spine subluxation. Painless sensory loss in the hands and feet may be present. With cervical subluxation, there may be extremity weakness or spasticity. Deep tendon reflexes are also increased.
Assess for hemiplegia, hemisensory loss, cranial nerve palsies, visual field defects, and cerebellar dysfunction if cervical artery dissection is suspected.
Skin inspection:
Central nervous system (CNS) infections (e.g., due to Neisseria meningitidis) can cause skin manifestations, such as petechiae and palpable purpura.
A papulovesicular rash in a dermatomal distribution indicates herpes zoster infection.[Figure caption and citation for the preceding image starts]: Zostiform vesicular eruption within the D8 dermatome on the leftBMJ Case Reports 2009; doi:10.1136/bcr.2006.114116. Copyright © 2011 by the BMJ Publishing Group Ltd [Citation ends].
Provocative tests
Spurling, shoulder abduction, and upper limb tension tests may be performed to test for cervical radiculopathy.[74]Bono CM, Ghiselli G, Gilbert TJ, et al; North American Spine Society. An evidence-based clinical guideline for the diagnosis and treatment of cervical radiculopathy from degenerative disorders. Spine J. 2011 Jan;11(1):64-72.
http://www.ncbi.nlm.nih.gov/pubmed/21168100?tool=bestpractice.com
These tests should not be performed in patients with rheumatoid arthritis, cancer, infection, or possible neck injury.
To perform the Spurling manoeuvres, while sitting, the patient's neck is slightly flexed to the side of pain and downward pressure is applied to the top of the head. The test is positive if pain radiates into the limb on the side that the head is rotated to. A positive test is highly suggestive of cervical radiculopathy.[75]Tong HC, Haig AJ, Yamakawa K. The Spurling test and cervical radiculopathy. Spine (Phila Pa 1976). 2002 Jan 15;27(2):156-9.
http://www.ncbi.nlm.nih.gov/pubmed/11805661?tool=bestpractice.com
The test has low sensitivity (30%) using electrodiagnostic studies as reference, but high specificity (93%).[75]Tong HC, Haig AJ, Yamakawa K. The Spurling test and cervical radiculopathy. Spine (Phila Pa 1976). 2002 Jan 15;27(2):156-9.
http://www.ncbi.nlm.nih.gov/pubmed/11805661?tool=bestpractice.com
Non-traumatic neck pain: laboratory investigations
There is no evidence that routine laboratory testing is helpful in the assessment of neck pain. However, the following tests are indicated if there is suspicion of serious aetiology, such as infection, malignancy, or inflammatory arthritis:
If there is a concern for meningitis or encephalitis
Lumbar puncture should be performed, and the following cerebrospinal fluid investigations requested:[26]National Institute for Health and Care Excellence. Meningitis (bacterial) and meningococcal disease: recognition, diagnosis and management. Mar 2024 [internet publication].
https://www.nice.org.uk/guidance/ng240
Fungal and viral cultures can be ordered if the patient is immunocompromised and there is concern for these infections. Acid-fast bacilli stain and smear is ordered if there is any history of tuberculosis exposure or if the patient is purified protein derivative positive.[76]Lewinsohn DM, Leonard MK, LoBue PA, et al. Official American Thoracic Society/Infectious Diseases Society of America/Centers for Disease Control and Prevention clinical practice guidelines: diagnosis of tuberculosis in adults and children. Clin Infect Dis. 2017 Jan 15;64(2):e1-33.
https://academic.oup.com/cid/article/64/2/e1/2629583
http://www.ncbi.nlm.nih.gov/pubmed/27932390?tool=bestpractice.com
If there is concern for cervical spine infection
Blood cultures should be drawn upon presentation if a patient is febrile and is suspected of having a cervical spine infection.
If vertebral osteomyelitis is suspected, and a microbiological diagnosis for a known associated organism has not been established by blood cultures or serological tests, a biopsy of the vertebra(e) thought to be infected should be sent for Gram stain and cultures with sensitivity.[77]Berbari EF, Kanj SS, Kowalski TJ, et al. 2015 Infectious Diseases Society of America (IDSA) clinical practice guidelines for the diagnosis and treatment of native vertebral osteomyelitis in adults. Clin Infect Dis. 2015 Sep 15;61(6):e26-46.
https://academic.oup.com/cid/article/61/6/e26/452579
http://www.ncbi.nlm.nih.gov/pubmed/26229122?tool=bestpractice.com
Non-traumatic neck pain: imaging
Cervical spine x-ray
Indicated in patients aged >50 years with new neck pain, or constitutional symptoms such as signs of infection. In cases of infection such as discitis, endplate destruction at the level of infection may be seen.[1]Guzman J, Haldeman, S, Carroll LJ, et al. Clinical practice implications of the bone and joint decade 2000-2010 task force on neck pain and its associated disorders: from concepts and findings to recommendations. Spine (Phila Pa 1976). 2008 Feb 15;33(4 suppl):S199-213.
http://www.ncbi.nlm.nih.gov/pubmed/18204393?tool=bestpractice.com
However, a negative cervical spine x-ray in a patient with fever is not sensitive enough to rule out infection; an MRI should be considered in those patients.[37]Expert Panel on Neurological Imaging, Ortiz AO, Levitt A, et al. ACR appropriateness criteria: suspected spine infection. J Am Coll Radiol. 2021 Nov;18(11S):S488-501.
https://www.jacr.org/article/S1546-1440(21)00724-9/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/34794603?tool=bestpractice.com
The recommended imaging of the cervical spine is an x-ray with anterior-posterior, lateral, and open mouth views. Flexion/extension radiographs have limited value in degenerative disease.[78]White AP, Biswas D, Smart LR, et al. Utility of flexion-extension radiographs in evaluating the degenerative cervical spine. Spine (Phila Pa 1976). 2007 Apr 20;32(9):975-9.
http://www.ncbi.nlm.nih.gov/pubmed/17450072?tool=bestpractice.com
Cervical spondylosis (osteoarthritis of the spine, which includes the spontaneous degeneration of either disc or facet joints) is an almost universal finding with increasing age.[15]Theodore N. Degenerative cervical spondylosis. N Engl J Med. 2020 Jul 9;383(2):159-68. Only a subset of patients present with axial neck pain; many patients are asymptomatic.[16]Binder AI. Cervical spondylosis and neck pain. BMJ. 2007 Mar 10;334(7592):527-31.[17]Kelly JC, Groarke PJ, Butler JS, et al. The natural history and clinical syndromes of degenerative cervical spondylosis. Adv Orthop. 2012;2012:393642.
http://www.ncbi.nlm.nih.gov/pubmed/22162812?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Normal lateral cervical spine x-rayWith permission of the University of Colorado Department of Radiology [Citation ends].
[Figure caption and citation for the preceding image starts]: C3-4 discitis with endplate destructionWith permission of the University of Colorado Department of Radiology [Citation ends]. [Figure caption and citation for the preceding image starts]: Bilateral facet dislocationWith permission of the University of Colorado Department of Radiology [Citation ends].
[Figure caption and citation for the preceding image starts]: Bilateral facet dislocationWith permission of the University of Colorado Department of Radiology [Citation ends].
Cranial CT imaging
Indicated in patients with suspected bacterial meningitis when it is associated with one or more of the following: immunocompromised state, history of CNS disease, new onset seizure, papilloedema, abnormal level of consciousness, or focal neurological deficit.[27]van de Beek D, Cabellos C, Dzupova O, et al. ESCMID guideline: diagnosis and treatment of acute bacterial meningitis. Clin Microbiol Infect. 2016 May;22 Suppl 3:S37-62.
https://www.clinicalmicrobiologyandinfection.com/article/S1198-743X(16)00020-3/fulltext
[36]Hasbun R, Abrahams J, Jekel J, et al. Computed tomography of the head before lumbar puncture in adults with suspected meningitis. N Engl J Med. 2001 Dec 13;345(24):1727-33.
https://www.nejm.org/doi/10.1056/NEJMoa010399
http://www.ncbi.nlm.nih.gov/pubmed/11742046?tool=bestpractice.com
Cervical spine MRI
Definitive test to evaluate patients for cervical radiculopathy or cervical myelopathy.[42]American College of Radiology. ACR appropriateness criteria: cervical pain or cervical radiculopathy. 2024 [internet publication].
https://acsearch.acr.org/docs/69426/Narrative
[79]American College of Radiology. ACR appropriateness criteria: myelopathy. 2020 [internet publication].
https://acsearch.acr.org/docs/69484/Narrative
Should be ordered if the patient with neck pain has neurological signs and symptoms of cord compression (cervical myelopathy), progressive neurological dysfunction (especially weakness) and lack of response to conservative therapy.[40]Carette S, Fehlings MG. Clinical practice. Cervical radiculopathy. N Engl J Med. 2005 Jul 28;353(4):392-9.
http://www.ncbi.nlm.nih.gov/pubmed/16049211?tool=bestpractice.com
MRI is not indicated as first-line imaging for patients with chronic, uncomplicated neck pain.[42]American College of Radiology. ACR appropriateness criteria: cervical pain or cervical radiculopathy. 2024 [internet publication].
https://acsearch.acr.org/docs/69426/Narrative
MRI is the imaging study of choice for patients with suspected local infection.[37]Expert Panel on Neurological Imaging, Ortiz AO, Levitt A, et al. ACR appropriateness criteria: suspected spine infection. J Am Coll Radiol. 2021 Nov;18(11S):S488-501.
https://www.jacr.org/article/S1546-1440(21)00724-9/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/34794603?tool=bestpractice.com
It is the recommended examination when there is evidence of bone or disc margin destruction. If an epidural abscess is suspected, MRI should be performed without and with IV contrast.[37]Expert Panel on Neurological Imaging, Ortiz AO, Levitt A, et al. ACR appropriateness criteria: suspected spine infection. J Am Coll Radiol. 2021 Nov;18(11S):S488-501.
https://www.jacr.org/article/S1546-1440(21)00724-9/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/34794603?tool=bestpractice.com
The use of an IV contrast agent not only increases lesion conspicuity, but also helps to define the extent of the infectious process.[37]Expert Panel on Neurological Imaging, Ortiz AO, Levitt A, et al. ACR appropriateness criteria: suspected spine infection. J Am Coll Radiol. 2021 Nov;18(11S):S488-501.
https://www.jacr.org/article/S1546-1440(21)00724-9/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/34794603?tool=bestpractice.com
[80]Diehn FE. Imaging of spine infection. Radiol Clin North Am. 2012 Jul;50(4):777-98.
http://www.ncbi.nlm.nih.gov/pubmed/22643395?tool=bestpractice.com
Cervical spine MRI should be used to evaluate neck pain in patients with a history of cancer.[42]American College of Radiology. ACR appropriateness criteria: cervical pain or cervical radiculopathy. 2024 [internet publication].
https://acsearch.acr.org/docs/69426/Narrative
Cervical MRI should document encroachment of the cervical root(s) suspected by history and physical examination.
Anatomical abnormalities such as disc protrusion (herniation/bulge) have been reported in 57% of patients (aged >64 years) with asymptomatic degenerative disk disease.[81]Teresi LM, Lufkin RB, Reicher MA, et al. Asymptomatic degenerative disk disease and spondylosis of the cervical spine: MR imaging. Radiology. 1987 Jul;164(1):83-8.
http://www.ncbi.nlm.nih.gov/pubmed/3588931?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: MRI cervical spine. Axial three-dimensional cosmic at C5/C6 with anterior indentation of the thecal sacBMJ Case Reports 2009; doi:10.1136/bcr.07.2008.0573. Copyright © 2011 by the BMJ Publishing Group Ltd [Citation ends].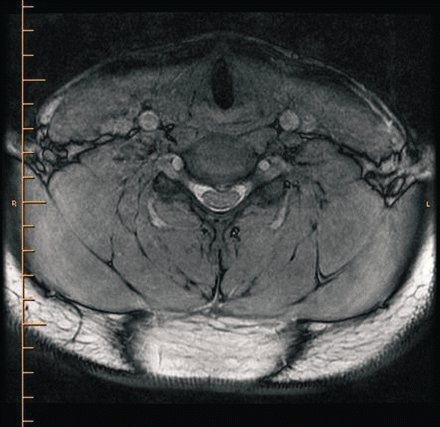 [Figure caption and citation for the preceding image starts]: MRI cervical spine. Sagittal T1, SE with a central disc at C5/C6 indenting the thecal sacBMJ Case Reports 2009; doi:10.1136/bcr.07.2008.0573. Copyright © 2011 by the BMJ Publishing Group Ltd [Citation ends].
[Figure caption and citation for the preceding image starts]: MRI cervical spine. Sagittal T1, SE with a central disc at C5/C6 indenting the thecal sacBMJ Case Reports 2009; doi:10.1136/bcr.07.2008.0573. Copyright © 2011 by the BMJ Publishing Group Ltd [Citation ends].
Cervical spine CT scan and CT myelography
CT imaging may be indicated if MRI cannot be performed.[42]American College of Radiology. ACR appropriateness criteria: cervical pain or cervical radiculopathy. 2024 [internet publication].
https://acsearch.acr.org/docs/69426/Narrative
CT myelography is used to visualise neurological encroachment, as with MRI. It requires invasive placement of radiological contrast into the epidural space and the use of radiation (and is therefore only recommended when cervical MRI is contraindicated).
Bone scan
Patients with new neck pain and a history of cancer, no matter how remote, should be evaluated for recurrence of their cancer with a bone scan to look for metastatic disease.[82]Canale ST, Beaty JH, eds. Campbell's operative orthopaedics. Philadelphia, PA: Mosby Elsevier; 2007.
Cervical facet injection and arthrography
Evidence to support use of cervical facet/medial branch nerve blocks to identify the origin of a patient’s pain is inconsistent.[83]Hurley RW, Adams MCB, Barad M, et al. Consensus practice guidelines on interventions for cervical spine (facet) joint pain from a multispecialty international working group. Reg Anesth Pain Med. 2022 Jan;47(1):3-59.
https://rapm.bmj.com/content/47/1/3
http://www.ncbi.nlm.nih.gov/pubmed/34764220?tool=bestpractice.com
Image-guided medial branch nerve blocks may, however, be the most efficacious way of isolating a specific facet joint as the origin of pain.
When selecting targets for blocks, levels should be determined based on clinical presentation (tenderness on palpation, preferably performed under fluoroscopy, and pain referral patterns).[83]Hurley RW, Adams MCB, Barad M, et al. Consensus practice guidelines on interventions for cervical spine (facet) joint pain from a multispecialty international working group. Reg Anesth Pain Med. 2022 Jan;47(1):3-59.
https://rapm.bmj.com/content/47/1/3
http://www.ncbi.nlm.nih.gov/pubmed/34764220?tool=bestpractice.com
History and physical examination cannot reliably identify painful atlanto-occipital and atlantoaxial joints, but can guide injection decisions.[83]Hurley RW, Adams MCB, Barad M, et al. Consensus practice guidelines on interventions for cervical spine (facet) joint pain from a multispecialty international working group. Reg Anesth Pain Med. 2022 Jan;47(1):3-59.
https://rapm.bmj.com/content/47/1/3
http://www.ncbi.nlm.nih.gov/pubmed/34764220?tool=bestpractice.com
Use of a single diagnostic block is recommended.[83]Hurley RW, Adams MCB, Barad M, et al. Consensus practice guidelines on interventions for cervical spine (facet) joint pain from a multispecialty international working group. Reg Anesth Pain Med. 2022 Jan;47(1):3-59.
https://rapm.bmj.com/content/47/1/3
http://www.ncbi.nlm.nih.gov/pubmed/34764220?tool=bestpractice.com
Dual blocks increase false-negative diagnoses (but can reduce the rate of false-positive diagnoses and enhance radiofrequency treatment success rates).[83]Hurley RW, Adams MCB, Barad M, et al. Consensus practice guidelines on interventions for cervical spine (facet) joint pain from a multispecialty international working group. Reg Anesth Pain Med. 2022 Jan;47(1):3-59.
https://rapm.bmj.com/content/47/1/3
http://www.ncbi.nlm.nih.gov/pubmed/34764220?tool=bestpractice.com
[84]Cohen SP, Huang JH, Brummett C. Facet joint pain-advances in patient selection and treatment. Nat Rev Rheumatol. 2013 Feb;9(2):101-16.
http://www.ncbi.nlm.nih.gov/pubmed/23165358?tool=bestpractice.com
Cervical discography
CT angiography (CTA) and MR angiography (MRA)
Can identify cervical artery dissections.[29]Yaghi S, Engelter S, Del Brutto VJ, et al. Treatment and outcomes of cervical artery dissection in adults: a scientific statement from the American Heart Association. Stroke. 2024 Mar;55(3):e91-106.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000457
http://www.ncbi.nlm.nih.gov/pubmed/38299330?tool=bestpractice.com
[46]Hanning U, Sporns PB, Schmiedel M, et al. CT versus MR techniques in the detection of cervical artery dissection. J Neuroimaging. 2017 Nov;27(6):607-12.
http://www.ncbi.nlm.nih.gov/pubmed/28574627?tool=bestpractice.com
The sensitivity and specificity of CTA is similar to digital subtraction angiography (the historical gold standard for diagnosis of cervical artery dissection).[29]Yaghi S, Engelter S, Del Brutto VJ, et al. Treatment and outcomes of cervical artery dissection in adults: a scientific statement from the American Heart Association. Stroke. 2024 Mar;55(3):e91-106.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000457
http://www.ncbi.nlm.nih.gov/pubmed/38299330?tool=bestpractice.com
CTA involves the administration of IV contrast. CTA is better than MRA in identifying pseudo-aneurysms, intimal flaps, and high-grade stenosis. MRA may perform better in identifying small intramural haematomas.[29]Yaghi S, Engelter S, Del Brutto VJ, et al. Treatment and outcomes of cervical artery dissection in adults: a scientific statement from the American Heart Association. Stroke. 2024 Mar;55(3):e91-106.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000457
http://www.ncbi.nlm.nih.gov/pubmed/38299330?tool=bestpractice.com
[85]Hakimi R, Sivakumar S. Imaging of carotid dissection. Curr Pain Headache Rep. 2019 Jan 19;23(1):2.
http://www.ncbi.nlm.nih.gov/pubmed/30661121?tool=bestpractice.com
American Heart Association guidelines advise that either CTA or MRA can be used to evaluate patients with suspected extracranial carotid and vertebral artery disease.[29]Yaghi S, Engelter S, Del Brutto VJ, et al. Treatment and outcomes of cervical artery dissection in adults: a scientific statement from the American Heart Association. Stroke. 2024 Mar;55(3):e91-106.
https://www.ahajournals.org/doi/10.1161/STR.0000000000000457
http://www.ncbi.nlm.nih.gov/pubmed/38299330?tool=bestpractice.com
[86]Brott TG, Halperin JL, Abbara S, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery. Developed in collaboration with the American Academy of Neurology and Society of Cardiovascular Computed Tomography. Catheter Cardiovasc Interv. 2013 Jan 1;81(1):E76-123.
https://onlinelibrary.wiley.com/doi/full/10.1002/ccd.22983
http://www.ncbi.nlm.nih.gov/pubmed/23281092?tool=bestpractice.com



 [Figure caption and citation for the preceding image starts]: Bilateral facet dislocationWith permission of the University of Colorado Department of Radiology [Citation ends].
[Figure caption and citation for the preceding image starts]: Bilateral facet dislocationWith permission of the University of Colorado Department of Radiology [Citation ends].
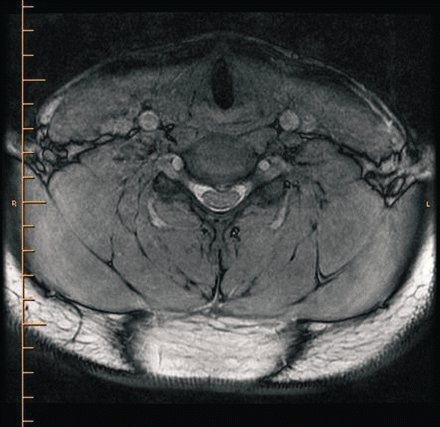 [Figure caption and citation for the preceding image starts]: MRI cervical spine. Sagittal T1, SE with a central disc at C5/C6 indenting the thecal sacBMJ Case Reports 2009; doi:10.1136/bcr.07.2008.0573. Copyright © 2011 by the BMJ Publishing Group Ltd [Citation ends].
[Figure caption and citation for the preceding image starts]: MRI cervical spine. Sagittal T1, SE with a central disc at C5/C6 indenting the thecal sacBMJ Case Reports 2009; doi:10.1136/bcr.07.2008.0573. Copyright © 2011 by the BMJ Publishing Group Ltd [Citation ends].