Aetiology
Cervical spondylosis
Cervical spondylosis (osteoarthritis of the spine, which includes the spontaneous degeneration of either disc or facet joints) is an almost universal finding with increasing age.[15]
Patients with cervical spondylosis may present with neck pain or with neurological complications (e.g., cervical spondylotic radiculopathy).[15][16] Mechanical and degenerative factors are more likely to be present in chronic neck pain.[16]
Neck pain is not, however, specific to cervical spondylosis. Only a subset of patients present with axial neck pain; many patients are asymptomatic.[16][17] Therefore, the clinical relevance of magnetic resonance imaging (MRI)-defined degenerative changes remains unclear.[16][18]
Some studies suggest that cervical degenerative changes may contribute to the aetiology of neck symptoms, but the associations are modest and should not guide clinical decisions.[18][19]
Whiplash
Whiplash commonly occurs after a rear-end motor vehicle collision. The injury from whiplash is unclear but is speculated to be predominantly related to ligamentous and muscular injury from the rapid-acceleration hyper-extension of the neck from the rear-end collision.[6][20][21]
Whiplash is a mechanism of injury, consisting of acceleration-deceleration forces to the neck.
Other causes of neck pain
Musculoskeletal (traumatic and non-traumatic)
Fracture: trauma, severe osteoporosis.
Dislocations: trauma.
Torticollis: aetiology unknown.
Cervical strain.
Osteoarthritis: degenerative joint destruction.
Rheumatoid arthritis: systemic illness, which can cause premature joint destruction.
Cervical stenosis: narrowing of the cervical spinal canal due to degenerative changes that can lead to compression of the nerve roots or spinal cord.
Cervical facet syndrome: chronic neck pain from any cause. The pain is referred to the head, neck, shoulder, and back in a non-dermatomal but reproducible pattern. There is no characteristic feature of cervical facet syndrome on examination. The examination must rule out cervical radiculopathy, myelopathy, or other causes of chronic neck pain.[Figure caption and citation for the preceding image starts]: Patient with severe left torticollis (note hypertrophy of right sternocleidomastoid muscle)From the personal collection of David B. Sommer, MD, MPH [Citation ends].

Neurological
Cervical radiculopathy: usually from cervical spinal stenosis, intervertebral disc herniation, and cervical spondylosis.
Cervical myelopathy: the most common cause is a combination of a congenitally narrow spinal canal and progressive cervical spondylosis.[Figure caption and citation for the preceding image starts]: MRI cervical spine. Sagittal T1, SE with a central disc at C5/C6 indenting the thecal sacBMJ Case Reports 2009; doi:10.1136/bcr.07.2008.0573. Copyright © 2011 by the BMJ Publishing Group Ltd [Citation ends].
 [Figure caption and citation for the preceding image starts]: MRI cervical spine. Axial three-dimensional cosmic at C5/C6 with anterior indentation of the thecal sacBMJ Case Reports 2009; doi:10.1136/bcr.07.2008.0573. Copyright © 2011 by the BMJ Publishing Group Ltd [Citation ends].
[Figure caption and citation for the preceding image starts]: MRI cervical spine. Axial three-dimensional cosmic at C5/C6 with anterior indentation of the thecal sacBMJ Case Reports 2009; doi:10.1136/bcr.07.2008.0573. Copyright © 2011 by the BMJ Publishing Group Ltd [Citation ends].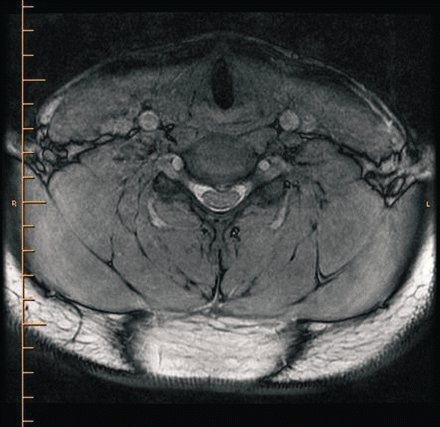
Neoplastic
Primary bone tumours are rare, accounting for less than 1% of all cancers.[22][23] Osteosarcoma is the most common primary bone cancer overall.[22] Incidence of other primary bone cancers (e.g., chondrosarcoma, Ewing sarcomas) varies with age.
Metastatic disease of the cervical spine is uncommon (8% to 20% with known metastases) compared with the rest of the spine (30% to 70%). The most common primary cancers for cervical metastases are breast, lung, prostate, kidney, and thyroid.[23]
Infectious
Osteomyelitis or epidural abscess: most patients have an underlying disease (diabetes, alcoholism, infection with HIV), spinal abnormality or intervention (trauma, surgery, drug injection), or systemic source of infection (skin or soft tissue infection, urinary tract infection, sepsis).[24]
Meningitis and encephalitis: aseptic meningitis (inflammation of the meninges without a known bacterial cause) is not typically life-threatening. Bacterial meningitis is life-threatening; delay in the administration of antibiotics is associated with poor outcomes. Encephalitis is evident by loss of cerebral function in addition to signs and symptoms of meningitis.[25][26][27]
Herpes zoster: most patients will have neuropathic pain localised to the affected dermatome. The symptoms may precede the rash. The rash characteristically has a red base with vesicles, which later scab over. Post-herpetic neuralgia is more common with older age, with 80% to 85% of cases occurring in people >50 years of age.[28][Figure caption and citation for the preceding image starts]: Zostiform vesicular eruption within the D8 dermatome on the leftBMJ Case Reports 2009; doi:10.1136/bcr.2006.114116. Copyright © 2011 by the BMJ Publishing Group Ltd [Citation ends].

Vascular
Cervical artery dissection is a significant cause of ischaemic stroke in younger adults. It can occur spontaneously or following cervical trauma.[29] In 8% of cases of spontaneous cervical artery dissection, pain is the only presenting symptom.[30]
Neck pain can occur with internal carotid and vertebral artery dissection.[31]
Carotid artery dissection: there may be associated symptoms of ipsilateral headache, eye pain, Horner’s syndrome, cranial nerve palsies, hemiplegia, hemisensory loss, visual neglect, and homonymous hemianopia.
Vertebral artery dissection: may be associated symptoms of vertigo, ataxia, dysarthria, and headache.[32] ‘Crossed’ syndromes with ipsilateral cranial nerve palsy and contralateral motor or sensory limb dysfunction are characteristic of posterior circulation stroke.[33]
Use of this content is subject to our disclaimer