Investigations
1st investigations to order
serum cryptococcal polysaccharide antigen (CrAg)
Test
CrAg can be detected using rapid antigen tests.[32][36]
A lateral flow assay (LFA) is a point-of-care rapid diagnostic test that provides results within 10 minutes. Plasma, serum, whole blood, or cerebrospinal fluid (CSF) can be tested.[37] Validation of one available CrAg LFA has shown sensitivity of 99.3% and specificity of 99.1%.[38] Latex agglutination (latex particles coated with polyclonal cryptococcal capsular antibodies), a direct antigen detection assay, is performed on blood, CSF, or body fluids such as pleural fluid and bronchoalveolar lavage samples. Latex agglutination sensitivity ranges from 97.0% to 97.8%, and specificity ranges from 85.9% to 100%.[38] False-positive results may occur at a rate of up to 0.4% due to the presence of rheumatoid factor or infections with Trichosporon beigelii, Stomatococcus mucilaginosus, Capnocytophaga canimorsus, or Klebsiella pneumoniae.[39][40][41] False-negative results are caused by a low fungal burden.
Serum CrAg is generally universally positive in patients with HIV infection and cryptococcal meningitis, and CSF involvement becomes increasingly probable as serum CrAg titres increase above 1:160 (LFA). At a serum titre of >1:1280, or >1:640 (LFA) in patients with HIV, even if CSF is CrAg negative, central nervous system brain parenchymal involvement should be assumed.[20][42] In pulmonary cryptococcosis, serum CrAg is usually negative if the infection is confined to the lung with ≤1 cm nodule. A positive result may indicate disseminated disease. Serial fluctuations in serum CrAg titres should not be used to guide treatment as the kinetics of CrAg elimination remain unclear.[1][43]
Result
positive
cerebrospinal fluid (CSF) cryptococcal polysaccharide antigen (CrAg)
pleural fluid cryptococcal polysaccharide antigen (CrAg)
cultures
Test
Cryptococcus neoformans and Cryptococcus var. gattii can be grown from biological samples, and colonies are observed on solid agar plates after 48 to 72 hours' incubation at 86°F (30°C) to 95°F (35°C) in aerobic conditions.[1] Samples from patients treated with systemic antifungal therapy may require more time to produce visible colonies.
Blood cultures may be positive in up to 50% of patients with HIV-associated cryptococcal meningitis.[20] Negative cerebrospinal fluid cultures in patients with cryptococcal meningitis may be caused by a low fungal burden. Bronchial secretions and urine can be contaminated by many micro-organisms that may mask the growth of cryptococci, especially in patients with AIDS. Prostatic massage can improve fungal detection on urine culture. Although Cryptococcus species is not considered normal respiratory flora in humans, it can occasionally colonise the respiratory tract of patients with lung disease, and sputum cultures may be positive.
Result
growth of Cryptococcus species
HIV antibodies
Test
Testing for HIV antibodies in patients with unknown HIV status who present with de novo cryptococcal meningitis or disseminated disease is recommended.[32]
Result
positive or negative
chest x-ray
Test
Radiological features of pulmonary cryptococcosis vary widely according to the immune state of the patient and include nodules, consolidation, cavitation, lobar infiltrates, hilar lymphadenopathy, mediastinal lymphadenopathy, pleural effusions, and collapse. Immunocompetent patients present with discrete nodules, whereas alveolar and interstitial infiltrates, cavitations, pleural disease, and collapse are more commonly seen in immunocompromised patients.[1][4][45][46][Figure caption and citation for the preceding image starts]: Bilateral cannonball lesions secondary to Cryptococcus neoformansFrom the collection of the radiology department, The Prince Charles Hospital, Chermside, Brisbane, Australia; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Pulmonary nodules in right lower lobe and left lower lobe secondary to Cryptococcus neoformansFrom the collection of the radiology department, The Prince Charles Hospital, Chermside, Brisbane, Australia; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Pulmonary nodules in right lower lobe and left lower lobe secondary to Cryptococcus neoformansFrom the collection of the radiology department, The Prince Charles Hospital, Chermside, Brisbane, Australia; used with permission [Citation ends].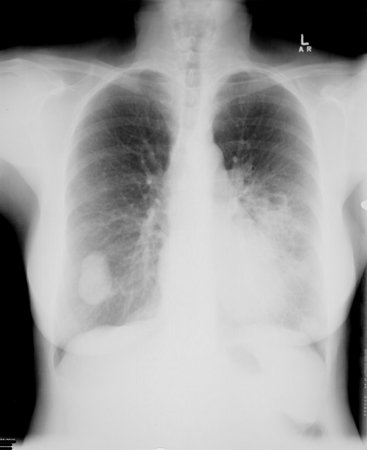 [Figure caption and citation for the preceding image starts]: Bibasal pneumonic consolidation secondary to Cryptococcus neoformansFrom the collection of the radiology department, The Prince Charles Hospital, Chermside, Brisbane, Australia; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Bibasal pneumonic consolidation secondary to Cryptococcus neoformansFrom the collection of the radiology department, The Prince Charles Hospital, Chermside, Brisbane, Australia; used with permission [Citation ends].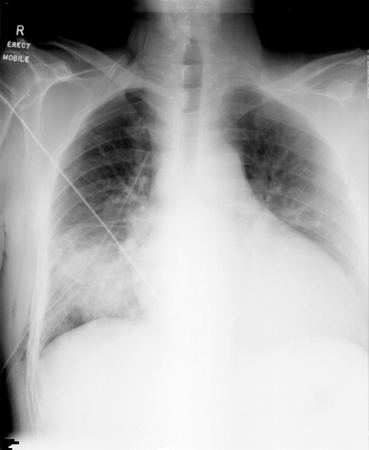 [Figure caption and citation for the preceding image starts]: Bilateral patchy opacification in mid-to-lower zones secondary to Cryptococcus neoformansFrom the collection of the radiology department, The Prince Charles Hospital, Chermside, Brisbane, Australia; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Bilateral patchy opacification in mid-to-lower zones secondary to Cryptococcus neoformansFrom the collection of the radiology department, The Prince Charles Hospital, Chermside, Brisbane, Australia; used with permission [Citation ends].
Result
nodules, consolidation, cavitation, lobar infiltrates, hilar lymphadenopathy, mediastinal lymphadenopathy, pleural effusions, and collapse
lumbar puncture
Test
Asymptomatic immunocompetent patients with pulmonary cryptococcosis and a negative serum cryptococcal polysaccharide antigen (CrAg) do not necessarily require a lumbar puncture to rule out central nervous system disease. Immunocompromised patients should undergo lumbar puncture regardless of symptoms, particularly when the serum CrAg titre is ≥1:160.[42]
Radiographical imaging of the brain with CT or MRI should be undertaken before lumbar puncture in patients with focal neurological signs or papilloedema, to identify mass lesions that may contraindicate lumbar puncture.[1][2]
Elevated intracranial pressure, defined as an opening pressure of >20 cm H₂O, measured with the patient in the lateral decubitus position, occurs in up to 80% of patients with cryptococcal meningitis and is associated with a poorer clinical response.[23][49][50][51] Opening pressures ≥25 cm H₂O may be detected in 60% to 80% of HIV-positive patients with cryptococcal meningitis.[20] US guidelines recommend measuring opening pressure at diagnosis in all patients with suspected cryptococcal meningitis.[20] About 25% of people may have normal glucose and protein.[53]
Result
elevated opening pressure (>20 cm H₂O); glucose: normal or slightly low (normal CSF glucose levels correspond to 60% to 70% of the concentration in blood [i.e., 2.5 to 4.4 mmol/L {45-80 mg/dL}]); protein: normal or slightly elevated (2.7 to 11.1 mmol/L [50-200 mg/dL], normal CSF total protein is 0.8 to 3.3 mmol/L [15-60 mg/dL] in adults)
cerebrospinal fluid (CSF) microscopy
Test
Direct microscopic examination of the CSF for the presence of encapsulated yeasts with India ink is a rapid and inexpensive diagnostic test for cryptococcal meningitis.[1][2][4][36] However, many laboratories no longer perform the India ink test, and its usefulness in the management of cryptococcal meningitis is limited.[20] India ink staining allows detection of yeasts in a CSF specimen when more than 10³ yeasts/mL are present, and shows encapsulated yeast in 60% to 80% of cases.[20]
In non-HIV cryptococcal meningitis, the sensitivity is 30% to 50%, whereas in HIV-associated cryptococcal meningitis it is up to 80%.[20] Centrifuging the CSF specimen can improve the sensitivity.
Dead yeast cells after appropriate antifungal treatment can remain in the CSF and cause false-positive results despite a negative culture. Myelin globules, fat droplets, lysed lymphocytes, and lysed tissue cells can also cause false-positive results.[1]
Result
presence of encapsulated yeasts
cerebrospinal fluid (CSF) white blood cell count (cells/mm³)
Test
Between 25% and 50% of people may have a normal CSF white cell count.[53]
Result
5-200 cells/mm³; lymphocytes (normal: 0-5 cells/mm³; lymphocytes)
Investigations to consider
CT chest
Test
Radiological features of pulmonary cryptococcosis vary widely according to the immune state of the patient and include nodules, consolidation, cavitation, lobar infiltrates, hilar lymphadenopathy, mediastinal lymphadenopathy, pleural effusions, and collapse. Immunocompetent patients present with discrete nodules, whereas alveolar and interstitial infiltrates, cavitations, pleural disease, and collapse are more commonly seen in immunocompromised patients.[1][4][45][46]
Result
nodules, consolidation, cavitation, lobar infiltrates, hilar lymphadenopathy, mediastinal lymphadenopathy, pleural effusions, and collapse
MRI brain
Test
MRI of the brain detects significantly more cryptococcosis-related lesions than CT.[47][48]
Cryptococcus var. gattii has a predilection to cause disease in the brain parenchyma rather than the meninges, resulting in cerebral cryptococcomas (represented by single or multiple focal mass lesions) or hydrocephalus.[1]
Result
single or multiple focal mass lesions in cryptococcoma, granulomas without significant mass effect, cysts (gelatinous pseudocysts), hydrocephalus, dilated Virchow-Robin spaces, and enhancing cortical nodules
CT brain
Test
MRI of the brain detects significantly more cryptococcosis-related lesions than CT.[47][48]
Cryptococcus var. gattii has a predilection to cause disease in the brain parenchyma rather than the meninges, resulting in cerebral cryptococcomas (represented by single or multiple focal mass lesions) or hydrocephalus.[1]
Result
single or multiple focal mass lesions in cryptococcoma, granulomas without significant mass effect, cysts (gelatinous pseudocysts), hydrocephalus, dilated Virchow-Robin spaces, and enhancing cortical nodules
bronchoscopy
Test
Cryptococcal polysaccharide antigen (CrAg) testing and cultures of bronchoalveolar lavage samples and washings may be positive in pulmonary cryptococcosis.[4]
CrAg testing in bronchoalveolar lavage samples is highly effective in diagnosing cryptococcal pneumonia with a titre >1:8, having 100% sensitivity and 98% specificity.[4]
Result
CrAg positive, growth of Cryptococcus species on culture
biopsy
Test
Histological examination of lung, skin, bone marrow, brain, or prostatic tissue can be undertaken to detect systemic dissemination.
Fine-needle aspiration (FNA) specimens obtained from the lymph nodes and adrenal glands can be used for cytological study. Percutaneous transthoracic FNA of pulmonary nodules or infiltrative lesions, under ultrasound or CT guidance, can be performed to diagnose pulmonary cryptococcosis.
Other specimens for cytological examination include bronchoalveolar lavage fluid, centrifuged cerebrospinal fluid, vitreous aspiration fluid, and seminal fluid.[1][2][4][36]
Result
presence of Cryptococcus species
Emerging tests
cryptococcus polymerase chain reaction (PCR)
Test
BioFire® FilmArray® PCR assay is available in the US.[20]
May give false-negative results if fungal burden is low in the cerebrospinal fluid, so should not be used as a diagnostic test in isolation.[20]
Likely to be most useful in differentiating a second episode of cryptococcal meningitis (PCR positive) from immune reconstitution inflammatory syndrome (PCR negative) in patients with HIV.[20]
Result
positive
Use of this content is subject to our disclaimer