Approach
Achalasia cannot be diagnosed on the basis of history alone. Symptoms are often slowly progressive, during which time many patients may adapt to significant symptoms by slowly altering their diet or eating habits. A minority of patients present with heartburn, regurgitation, or slow eating compared with other family members, rather than dysphagia.[22]
Barium swallow or endoscopy can appear normal in patients with early disease. Therefore, many patients with achalasia may be symptomatic for months or years before the correct diagnosis is made.[22][23]
History
Dysphagia to solids and liquids is the key symptom of achalasia. Dysphagia to liquids is uncommon in structural causes of oesophageal obstruction, except in advanced disease. Therefore, its occurrence at presentation suggests an oesophageal motility disorder.[22]
Patients often develop a range of strategies to live with dysphagia, such as arching the neck and shoulders, raising the arms, standing or sitting up straight during the meal, and walking around after a meal.[22] These manoeuvres increase intrathoracic pressure to overcome the increased lower oesophageal sphincter pressure, allowing oesophageal contents to empty into the stomach. Patients may eat slowly and take longer than others to finish their meal.
Drinking fluid may initially cause a sensation of retrosternal pressure, which is relieved by continued drinking.
Retrosternal pain typically affects younger patients and may be relieved by drinking cold water.[24] It is often described as cramp-like in nature and may wake the patient from sleep. This may persist even when dysphagia has improved following successful dilatation.
Regurgitation results from retention of food and liquids in the oesophagus, and is more common in established disease when the oesophagus has become dilated. Bland, undigested food or saliva retained in the oesophagus regurgitates when the patient is in the recumbent position and may wake the patient from sleep with coughing and choking, sometimes leading to chest infections. This differs from regurgitation from gastro-oesophageal reflux, where the gastric regurgitate tastes sour.
As a result of regurgitation of retained food, aspiration may result in chest infections with symptoms of coughing and choking, which can interrupt sleep.
Coughing or choking while recumbent may occur secondary to regurgitation of retained food and liquids in the oesophagus.
Heartburn can also occur, possibly secondary to fermentation of food retained in the oesophagus rather than gastric acid reflux past a high-pressure lower oesophageal sphincter.
Weight loss is usually gradual and mild, unlike in pseudoachalasia where the underlying malignancy often causes rapid and profound weight loss.[23]
Atypical symptoms include a globus sensation (i.e., of a lump in the throat) and hiccups.
Physical examination
There are no specific physical signs in achalasia, but recent, rapid weight loss should alert the clinician to the possibility of underlying malignancy, which can present as pseudoachalasia.
Initial investigations
Dysphagia should always be promptly investigated.
Upper gastrointestinal endoscopy, to exclude malignancy, is usually the first investigation for dysphagia.[25] However, barium swallow may be the best initial test for high dysphagia in older individuals, in case there is a pharyngeal pouch. In early achalasia, endoscopic abnormalities can be subtle and the endoscopy may be reported as normal.
Following endoscopy, people with suspected achalasia will usually undergo a barium swallow and oesophageal manometry.
Barium swallow may also be normal in the early stages of the disease, but often demonstrates loss of peristalsis and delayed oesophageal emptying. The typical appearance in achalasia is that of a dilated oesophagus that tapers smoothly to a beak-like narrowing. In severe disease, the oesophagus may be tortuous and sigmoid-shaped with diverticula. Fluoroscopy is often used during a barium swallow.[26]
Oesophageal manometry: incomplete relaxation of the lower oesophageal sphincter (LOS) and oesophageal aperistalsis are the two most important manometric criteria for the diagnosis of achalasia.[27]
High-resolution manometry is more accurate than conventional manometry and is the preferred investigation in the diagnosis of achalasia.[28][29]
Three subtypes of achalasia, based on the pattern of oesophageal contractility, have been described using high-resolution manometry and are classified using the Chicago criteria.[30] The subtypes are impaired LOS relaxation without peristalsis (type I), impaired LOS relaxation with pan-oesophageal pressurisation (type II), and impaired LOS relaxation with premature oesophageal contractions or distal peristalsis (type III). Achalasia subtype predicts treatment response.
Subsequent studies
Chest x-ray may offer some clues: absence of the gastric gas bubble and a dilated oesophagus with an air-fluid level may be noted, but is not diagnostic.
CT is a useful investigation to exclude gastro-oesophageal infiltration by invading extrinsic or intrinsic malignancy. Asymmetrical thickening on CT may suggest pseudoachalasia. CT is recommended in an older individual or if there is rapid or profound weight loss.
Radionucleotide oesophageal emptying studies can be used for monitoring response to therapy.[31] They can demonstrate delayed transit time but are not first line for the initial diagnosis of achalasia.
Timed barium oesophagogram (i.e., barium swallow in which multiple sequential films are shot at pre-set time intervals) is a simple technique that directly measures liquid oesophageal emptying. It does not require any special equipment or expertise and is repeatable; therefore, it can be used to assess the progress of the disease and the outcome of treatment.[32][33][Figure caption and citation for the preceding image starts]: Classic appearance of dilated oesophagus with tapered beak-like narrowing on barium studyFrom the collection of Dr Jin-Yong Kang; used with permission [Citation ends].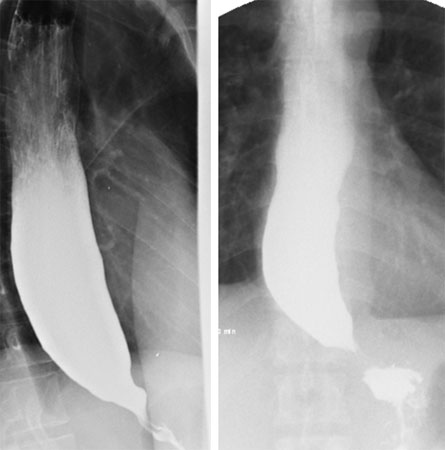 Impedance planimetry is a method for evaluating sphincter function by measuring changes in pressure with diameter and volume.[34] This can be utilised at the time of endoscopy or surgery at the gastro-oesophageal junction to measure the gastro-oesophageal junction distensibility using the functional luminal imaging probe (FLIP) device. This may provide complementary information to high-resolution manometry where the diagnosis of achalasia is not clear and may provide peri-operative or endoscopic response to treatment in real-time.[35]
Impedance planimetry is a method for evaluating sphincter function by measuring changes in pressure with diameter and volume.[34] This can be utilised at the time of endoscopy or surgery at the gastro-oesophageal junction to measure the gastro-oesophageal junction distensibility using the functional luminal imaging probe (FLIP) device. This may provide complementary information to high-resolution manometry where the diagnosis of achalasia is not clear and may provide peri-operative or endoscopic response to treatment in real-time.[35]
Use of this content is subject to our disclaimer