Approach
Hoarseness is a common symptom that may present to a variety of different specialists including primary care physicians, paediatricians, and internists.[44][45][46][47] A clear understanding of the causes of hoarseness and an appreciation that it may represent a serious underlying pathology are vitally important.[1] Prompt referral to the appropriate specialist for assessment and treatment of hoarseness is essential in order to provide the best possible care and improve prognosis.
The diagnosis and management of hoarseness involves a multi-disciplinary team with otolaryngologists and speech language pathologists (many of whom specialise in the voice); neurologists, psychiatrists, or psychologists may be consulted depending on the underlying pathology.[48][49][50][51] Specialised voice centres offer a collaborative approach towards the treatment of hoarseness involving a thorough evaluation and initiation of a comprehensive medical and behavioural management plan.[52]
History
Vocal symptoms
Patients typically present with a combination of vocal symptoms depending on the causative condition. The onset, duration, progression, and variability of these symptoms should be assessed to aid diagnosis.[3]
The most common vocal symptoms are hoarseness and roughness, breathiness, tremor, raspiness, stridor, weakness, reduced pitch range, low vocal pitch or inappropriately high vocal pitch, reduced volume range, quiet voice, vocal fatigue, vocal strain and increased phonatory effort, voice breaks, voice loss and aphonia, and pain or discomfort.
As voice changes may develop gradually over a long period of time, patients often delay presentation to their primary care physician for evaluation and treatment until they experience a disruption to their quality of life.
Vocal coaches and professional singers may identify vocal fold pathology at an earlier stage through recognition of subtle changes in the quality of the voice and thus present sooner.
Phonotrauma may be present and is indicated by the onset of laryngitis. For example, following attendance at a football game and post-game party, a patient may experience throat tenderness, pitch breaks, voice breaks, and occasional complete loss of voice by the end of the day.
There may be a multi-factorial hoarseness characterised by a 2- to 5-year history of gradual voice changes with intermittent voice loss, loss of high notes, symptoms of uncontrolled reflux, and occasional tenderness in the neck. A history of frequent bouts of bronchitis and upper respiratory illness in winter is also common.
Acute laryngitis is characterised by an acute onset of breathiness, vocal weakness, and fatigue, while chronic laryngitis presents with roughness, altered pitch and volume, and voice breaks.
Reflux laryngitis typically presents with altered vocal pitch; chronic cough and throat clearing with excess throat mucous or post-nasal drip; dysphagia to solids, liquids, or pills; coughing after eating or lying down; breathing difficulty or choking episodes; globus; and heartburn (in <50% of cases).[53]
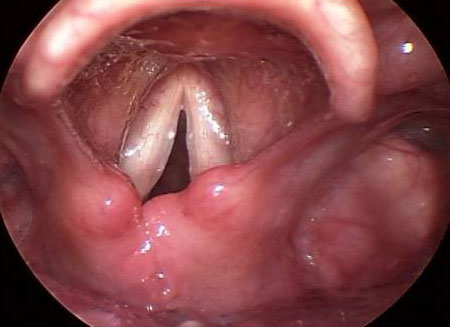
[Figure caption and citation for the preceding image starts]: Reflux laryngitisFrom the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].

Hypokinetic dysarthria is characterised by reduced pitch range and loudness, monotonal vocal production, decreased phrase length, dysarthria, altered rate of speech (faster or slower) with short rushes of speech, and impaired intelligibility.[54]
Past medical history
Surgery to the base of the skull, neck region (e.g., thyroidectomy, anterior cervical fusion), or thorax (e.g., thoracic aortic aneurysm repair, oesophagectomy) can damage the superior or recurrent laryngeal nerves supplying the intrinsic laryngeal muscles.
Previous intubation may result in granuloma formation, post-intubation phonatory insufficiency, and vocal fold paresis.[55]
Laryngopharyngeal reflux has been implicated in the pathogenesis of acute and chronic laryngitis, benign vocal fold lesions, and muscle tension dysphonia.[5]
Psychological stress and other emotional issues have been associated with the development of hoarseness.[9][56][57][58] Voice changes reflecting deeper emotional concerns should not be overlooked.
Some neurological conditions are known to result in hoarseness such as Parkinson disease, essential tremor, brainstem lesions, and stroke.
Drug history
Determine which, if any, prescription medicines the patient is taking. This may highlight a condition known to cause hoarseness, or reveal a drug that may be a contributing factor in the development of hoarseness.[3] Examples include: fluticasone/salmeterol inhaler (secondary to fungal laryngitis), alendronic acid (secondary to increased reflux), and ACE inhibitors (secondary to chronic cough).
Family history
Some conditions known to be associated with hoarseness - including laryngopharyngeal reflux, essential tremor, Parkinson's disease, spasmodic dysphonia, and some cancers - can be hereditary.
Social history
Past and present tobacco use history (including a calculation of the number of pack-years smoked), amount of alcohol and caffeine consumed, and any recreational drug use should be assessed.
Employment history is important to evaluate the importance and pattern of vocal use in the patient's profession and to assess exposure to environmental irritants and noise.
Physical examination
All patients presenting with hoarseness should receive a thorough physical examination to identify any underlying causative medical conditions. Particular attention should be given to examination of the head and neck and the neurological and respiratory systems.[3]
Head and neck examination
Equipment such as a white light source (halogen), gauze, tongue blade, and gloves are required.
Examination should include inspection and palpation for masses and enlargement of the cervical lymph nodes, thyroid gland, and salivary glands; cranial nerve examination; intra-oral inspection and palpation of the lips, cheeks, floor of mouth, tongue (including lateral borders), tonsillar pillars and fossae, hard and soft palate, and gingival tissue.[59]
Important findings include regional cervical lymphadenopathy in leukoplakia, vocal fold cancer, and vocal fold paralysis or paresis (if secondary to a malignant cause); unilateral or bilateral oral and facial muscle weakness in vocal fold paralysis; white patches on the tongue, buccal mucosa, and/or palate in leukoplakia.
Neurological examination
The patient should be examined for progressive dysarthria, vocal weakness, fatigability, gait abnormalities, rigidity (cogwheel), resting and intention tremor, bradykinesia (masked facies, decreased arm swing, shuffling gait), hyper/hypo-nasality, and dysphagia (choking on solids or liquids, effortful swallowing).
Parkinson's disease is characterised by rigidity (cogwheel), resting tremor (4 to 6 Hz), and bradykinesia resulting in masked facies, a shuffling gait, and decreased arm swing.[60]
Essential tremor is characterised by a slowly progressive clinical course (at least a 3-year history of tremor).[61] Rest tremor can occur in severe essential tremor. The head and voice may be involved. The vocal tremor is more evident with connected speech than with singing or sustained phonation.[62]
Respiratory examination
Inspiratory or biphasic stridor, noisy resting breathing, dyspnoea, respiratory distress with accessory muscle use and tachypnoea, shortness of breath while speaking with the inability to complete sentences in a single breath, and/or a non-productive cough are important signs of airway obstruction and require immediate attention.
Non-invasive assessment
Patient self-evaluation
The Voice Handicap Index (VHI)-30, the abbreviated VHI-10, and the Pediatric VHI for children aged 4-13 years allow evaluation of the patient's perception of the severity of their voice problem.[63][64][65]
The Reflux Symptom Index assesses the severity of laryngopharyngeal reflux symptoms and the possible relationship with the presenting hoarseness.[53]
Perceptual assessment
Although there is ongoing controversy related to inter-rater reliability of perceptual assessment and there is no consensus on standard perceptual scales, listening to the voice in conjunction with observing physical appearance, patient interaction, posture, breathing patterns, and signs of musculoskeletal tension contributes to the development of a behavioural management plan.[66]
Perceptual voice assessments are designed to describe voice attributes and serve as a standardised means of communication among clinicians. Overall severity of the voice complaint is defined as the global, integrated impression of voice deviance.[67]
Voice attributes are described in terms of roughness (perceived irregularity in the voicing source), breathiness (audible air escape in the voice), strain (perception of excessive vocal effort or hyper-function), pitch (perceptual correlate of fundamental frequency related to gender, age, and referent culture), and loudness (perceptual correlate of sound intensity).
Two of the commonly used perceptual scales are GRBAS and the Consensus Auditory-Perceptual Evaluation of Voice (CAPE-V):[68][67]
GRBAS: subjective rating scale providing a measure of the overall grade (G), roughness (R), breathiness (B), asthenia or weakness (A), and strain (S) of dysphonia as judged by the listener on a scale of 0-4 (0: normal, 1: mild, 2: moderate, 3: moderate to severe, 4: severe).
CAPE-V: represents each voice attribute with a visual analogue scale displaying the terms MI (mildly deviant), MO (moderately deviant), and SE (severely deviant) referring to the perceived degree of deviance from normal.
Acoustic assessment
Acoustic recordings of the voice allow documentation of vocal function and provide a means for the determination of outcome measures.[69] Acoustic signs of voice problems can be identified through several parameters: fundamental frequency (average, variability, range, perturbation), amplitude (sound pressure level, variability, range, perturbation), signal-to-noise ratio, vocal rise/fall time, tremor, phonation time, voice, and pitch breaks.[3]
The Dysphonia Severity Index (DSI) is used as an objective outcome measure for the voice. It is based on highest frequency (F0-High in Hz), lowest intensity (I-Low in dB), maximum phonation time (MPT in seconds), and jitter (%). DSI ranges from +5 (perceptually normal voice) to -5 (severely dysphonic voice); the more negative the DSI, the worse the vocal quality. A high correlation exists between the DSI and the VHI score.[70]
Aerodynamic assessment
Aerodynamic measures can be assessed simply by the primary physician, through the measurement of maximum phonation time (longest time the patient can hold a sustained vowel, typically the 'ah' sound) and s/z ratio (length of time the patient can hold the 's' in comparison with the 'z' sound).[71] The normal s/z ratio is 1:1, but subjects with laryngeal pathology will have a lower phonation time for 'z' than for 's.'[72]
Aerodynamic assessment measures:
Air flow (measurement of steady and peak airflows during connected speech; increases with vocal fold pathology)
Air pressure (measurement of the air pressure below the vocal folds required for vibration and loudness; high air pressure levels may indicate excessive lung pressure or inefficient valving of the larynx indicative of vocal fold paralysis; variation in air pressure may indicate poor motor control or a neurolaryngeal disorder)
Phonation threshold pressure (minimum level of lung pressure required to sustain vocal fold oscillation at a specific pitch; dependent on hydration, pitch, skill and fatigue; influenced by vocal fold lesions).[73]
Invasive tests
Laryngoscopy
Performed if dysphonia doesn’t resolve or improve by 4 weeks of symptom onset, or if a serious underlying cause is suspected (regardless of symptom duration).[3]
Indirect laryngoscopy allows the evaluation of laryngeal colour and structure and visualisation of laryngeal lesions.[70]
Direct laryngoscopy is an endoscopic evaluation of the larynx. It allows the evaluation of laryngeal structure and function by means of a flexible fibre-optic nasendoscope or a rigid oral endoscope with a halogen light source.[74] Benefits include the ability to visualise the vocal folds in a patient who cannot tolerate indirect laryngoscopy and observation of the larynx in a more natural position, allowing for observation of resting breathing, speaking, and singing.[75] Direct laryngoscopy may include the use of videostroboscopy.
Videostroboscopy
A critical component of the voice examination, as it allows evaluation beyond what the naked eye is able to detect.[76]
Allows the evaluation of laryngeal structure and function, providing detailed information on laryngeal anatomy (including the vocal fold edges) and voice physiology. It also provides a permanent record of the measurements taken.[Figure caption and citation for the preceding image starts]: Normal vocal fold layer structureFrom the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].
Indications for referral for videostroboscopic evaluation include abnormal voice changes or concerns of unknown organic aetiology, abnormal voice changes after surgery or trauma, presence of laryngeal pathology, comparison with previous evaluations, and voice characteristics that differ from known laryngeal status.[77]
Examination is performed with a rigid endoscope placed in the mouth up to the tongue base, or with a flexible fibre-optic nasendoscope with a xenon light source passed through the hypo-pharynx for an unimpaired view of the larynx.
Flexible fibre-optic nasendoscopy is preferred for evaluation of neurolaryngeal disorders (including hypokinetic dysarthria, spasmodic dysphonia, and essential tremor) for:[62]
Visualisation of vocal fold mobility
Differentiation of vocal fold paralysis from paresis
Hypo- and hyper-functional vocal fold behaviours
Laryngeal muscle tone and agility.
Flexible fibre-optic nasendoscopy is also used when examination with a rigid endoscope does not allow adequate visualisation due to structural interference or patient discomfort.
Examination should be performed by a skilled physician or speech language pathologist with knowledge of voice disorders and laryngeal physiology.
High-speed digital imaging
Measures and records each cycle of vocal fold vibration, vocal fold amplitude, glottal width, left-right asynchrony, temporal changes in vocal fold vibration, mucosal wave, vertical plane differences of the vocal folds, and vocal fold closure patterns.
Commercially available clinical systems record ≥2000 frames per second for a duration of 2-8 seconds.
Laryngeal electromyography
This electrophysiological study is performed by a neurologist or otolaryngologist and evaluates muscle motor unit potentials and loss of innervating neurons, the function of the recurrent and superior laryngeal nerves, and the chronicity of injury to the laryngeal nerves.
It also allows prediction of recovery and provides assistance with treatment of laryngeal dystonia.[78]
Biopsy
Biopsy is mandatory in any case of suspected vocal fold cancer.[3] Conservative therapy (with avoidance of irritants and treatment of laryngeal candidiasis) may be considered prior to biopsy for leukoplakia present on otherwise mobile vocal folds.[3]
Although microscopic analysis of benign vocal fold lesions is generally performed, the incidence of malignancy in such lesions is extremely low, and the biopsy results are hindered by a hypo-cellular specimen and small sample size. It should be noted that benign vocal fold lesions are derived from the vocal fold lamina propria, whereas vocal fold cancer develops in the epithelium that envelops the lamina propria.
Imaging
Radiological imaging
Indicated when there is suspicion of vocal fold cancer or neurological impairment.
Should not be obtained among patients with a primary voice complaint until laryngoscopy has been performed.[3]
CT of the head, neck, larynx, and chest is used to identify and locate tumours on the recurrent laryngeal nerve and lung or mediastinal masses.[79]
Small laryngeal lesions may be missed on a CT scan, but these will be seen on flexible fibre-optic laryngoscopy.
MRI may be used for patients who cannot undergo a CT scan, or as a complementary tool if CT does not provide adequate information.
Use of this content is subject to our disclaimer