Aetiology
The aetiology of vocal fold tissue pathologies causing disruption of normal voice quality and production can be hard to identify in the absence of acute illness, accident, or injury. Additionally, several laryngeal and extra-laryngeal disorders are associated with the development of hoarseness. These disorders may be classified as functional, inflammatory, benign, neurological, malignant, or pre-malignant.
Functional disorders
Muscle tension dysphonia
A condition that results from imbalance of the intrinsic and extrinsic laryngeal muscles, hindering voice production.
Associated with various interacting factors including GORD, laryngopharyngeal reflux, asthma, allergies, sinusitis, neuromuscular abnormalities, vocal use and behaviour, emotion, depression, or anxiety.[4][5] Introverted personality type has been implicated in the aetiology of muscle tension dysphonia.[6][7]
In primary muscle tension dysphonia, laryngeal muscle imbalance occurs in the absence of an associated organic vocal fold pathology.
In secondary muscle tension dysphonia, compensatory behaviours secondary to an associated organic or psychogenic disorder (conversion disorder) result in laryngeal muscle imbalance.
Inflammatory causes
Prolonged and severe inflammation can be harmful to laryngeal tissue. However, the inflammatory process is sometimes beneficial in order to limit damage to areas of injury, and promote healing and repair. Severe infections and other conditions causing inflammation of the larynx should be treated promptly and aggressively. There are several causes of laryngeal inflammation.
[Figure caption and citation for the preceding image starts]: Mirza inflammatory treeReprinted with permission from Merati AL, Bielamowicz SA, eds. Textbook of laryngology. San Diego, CA: Plural Publishing; 2006. All rights reserved [Citation ends].
Acute laryngeal inflammation
Occurs quickly in response to infection, trauma, or surgery.
Causes include respiratory infection (bacterial, viral, fungal), tuberculosis (TB), phonotrauma, and/or exposure to environmental irritants or noxious agents.
Signs include erythema, oedema, ulceration, and loss of function.
Most causes of acute laryngitis are self-limiting.[8]
Chronic laryngeal inflammation
May last for several weeks.
Causes include chronic or recurrent respiratory infections (bacterial, viral, fungal), TB, laryngopharyngeal reflux, phonotrauma, and/or exposure to environmental irritants or noxious agents.
Results in less initially dramatic pathological changes than those observed in acute inflammation.
May lead to tissue fibrosis and scarring.
Reflux laryngitis [Figure caption and citation for the preceding image starts]: Reflux laryngitisFrom the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].
Secondary to laryngopharyngeal reflux.
May be complicated by vocal fold granuloma formation, aspiration, laryngospasm, and sub-glottic stenosis.[9]
Sub-acute laryngeal inflammation is a poorly defined and infrequently identified condition caused by episodic events such as environmental exposure to airborne irritants or allergies.
Benign vocal fold lesions
Benign vocal fold lesions are characterised by a disturbance in the extracellular matrix protein structure of the superficial lamina propria.[9]
Vocal fold nodules, cysts, polyps, fibrous masses, granulomata, and scars[Figure caption and citation for the preceding image starts]: Vocal fold polypFrom the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].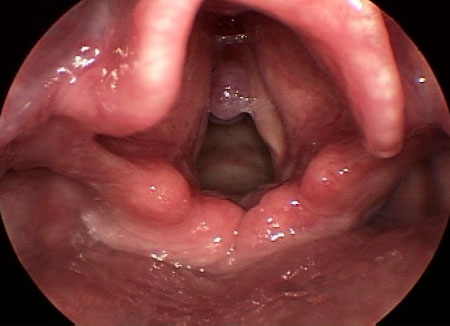
Develop as a result of the abnormal physiological healing of injury and inflammation inflicted on vocal fold tissue by excessive mechanical stress secondary to phonotrauma and vocal overuse or misuse.[9][10] If the precipitating factor is removed at an early stage, oedema and vocal fold nodules may be potentially reversible.
Phonotrauma is caused by vocal behaviours such as: increased laryngeal tension or strain; hard glottal attack; inappropriate pitch level and lack of pitch variability; excessive talking; prolonged use of excessive vocal volume; strained and excessive use of the voice during periods of swelling; inflammation or other tissue pathologies; excessive coughing and throat clearing; screaming or other noise making; misuse of the voice through cheering at a sports event, teaching, cheerleading, and untrained singing.[9]
Dehydration, chronic or recurrent respiratory infections (bacterial, viral, fungal), TB, laryngopharyngeal reflux, phonotrauma, and exposure to environmental irritants or noxious agents are additional contributory factors in the development of these lesions.[9]
People with benign vocal fold lesions have been found to be socially dominating extroverts.[6][11]
Vocal fold cysts may be congenital or acquired. A mucous retention cyst occurs due to obstruction of a mucous-producing gland, and an epidermoid cyst occurs due to phonotrauma or, possibly, from a remnant of epithelium trapped in the medial layer of the vocal fold.[9][Figure caption and citation for the preceding image starts]: Vocal fold cystFrom the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].
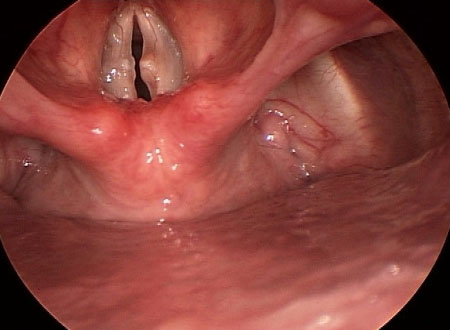
Vocal fold granulomata form as a result of prolonged or recurrent trauma (phonotrauma or post-intubation) and acid irritation (secondary to laryngopharyngeal reflux) to the posterior glottis and vocal folds.[12] There is a high rate of recurrence of granulomata post-treatment if the underlying cause is not eliminated. [Figure caption and citation for the preceding image starts]: Granuloma 1From the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].
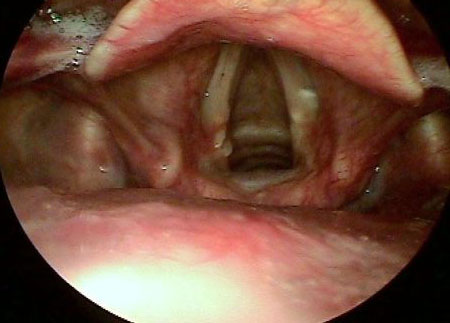 [Figure caption and citation for the preceding image starts]: Granuloma 2From the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].
[Figure caption and citation for the preceding image starts]: Granuloma 2From the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].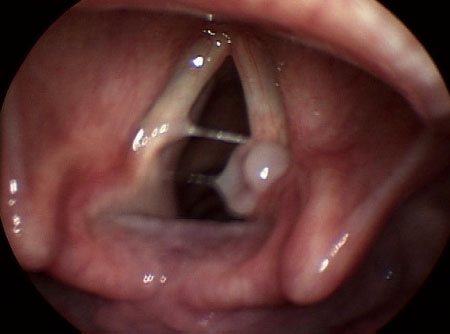
Vocal fold scarring is characterised by permanent change in the superficial lamina propria secondary to the loss of the viscoelastic properties of the vocal fold epithelium, due to prolonged phonotrauma, laryngeal microsurgery, or laryngeal radiation for cancer of the head and neck.
Recurrent respiratory papilloma [Figure caption and citation for the preceding image starts]: Recurrent respiratory papillomaFrom the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].
Epithelial growth on the vocal folds due to infection with human papillomavirus.
Reinke's oedema [Figure caption and citation for the preceding image starts]: Reinke's oedemaFrom the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].
Accumulation of gelatinous material in the superficial lamina propria with oedema along the entire vocal fold length secondary to heavy smoking.[13] Laryngopharyngeal reflux and phonotrauma are possible contributory factors.
Presbylarynx
Term describing the age-related physiological changes of tissue atrophy, decreased muscle fibre mass, increased fat infiltration, cartilage ossification, joint arthritis, and decreased respiratory support that can alter voice quality, pitch, and loudness.[14]
Common cause of hoarseness with age over 60 years.[14]
It is important to exclude other progressive neurological disorders that may have early involvement of similar voice characteristics such as Parkinson's disease.
Neurological causes
Laryngeal dysfunction secondary to neurological disease may first present with voice changes, swallowing problems, or breathing difficulty and is often missed by the non-specialist.[15] Disruption to any of the neuroanatomical systems and pathways (cerebellum, extra-pyramidal system, upper and lower motor neurons, neuromuscular junction, muscle unit) involved in voice production and speech can result in hoarseness. The 4 most common neurological causes of hoarseness are vocal fold paralysis or paresis, hypokinetic dysarthria, essential tremor, and spasmodic dysphonia.
Vocal paralysis or paresis
May be due to complete immobility (paralysis) or some mobility in the presence of partial dysfunction (paresis). These terms are used to describe unilateral or bilateral immobility or weakness of the arytenoid complex.
Unilateral or bilateral injury to or lesion of the recurrent or superior laryngeal nerves that supply the intrinsic muscles of the larynx can lead to hoarseness.
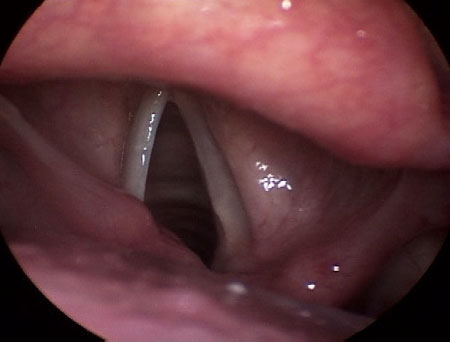
Unilateral vocal fold paralysis is commonly idiopathic or secondary to nerve dysfunction.[16][Figure caption and citation for the preceding image starts]: Left vocal fold paralysisFrom the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].
Other causes include surgical trauma (thyroidectomy, anterior cervical fusion, thoracic aortic aneurysm repair, oesophagectomy, skull base surgery) and central venous catheterisation; malignant or benign tumours of the brain, base of skull, thyroid, thymus, and oesophagus; masses in the parapharyngeal space and vagal neuromas; and neurological disease (stroke, amyotrophic lateral sclerosis, post-polio syndrome, Charcot-Marie-Tooth disease, bulbar palsy).[16][17]
Bilateral vocal fold paralysis has similar aetiologies to its unilateral counterpart but is significantly rarer.[18][19] Common causes include thyroidectomy, congenital disorders (Chiari malformation), brainstem lesions, prolonged intubation, head and neck radiation fibrosis, and granulomatous diseases (TB, sarcoidosis, amyloidosis).
Hypokinetic dysarthria
Most commonly caused by Parkinson's disease, a degenerative movement disorder characterised by decreased dopamine levels in the basal ganglia. Associated with a high incidence of voice and communication impairment, with approximately 75% to 90% of those affected experiencing some form of speech difficulty such as low volume speech, impaired intelligibility, and monotonicity.[20]
Essential tremor
A movement disorder characterised by an involuntary tremor on movement that affects the voice in approximately 25% of cases.[21][22] It is important to differentiate essential tremor from Parkinson's disease and spasmodic dysphonia.
Spasmodic dysphonia
A rare laryngeal dystonia or movement disorder due to spasm of either the adductor or abductor muscles. Very rarely it can affect both muscles. Typical age of onset is around 30 years and it is more common in females than in males.[23]
Family history of neurological disorders, heavy voice use, and recent viral illness have all been identified as possible risk factors.[24]
Malignant/pre-malignant vocal fold lesions
Causes include laryngeal malignancies, the most common of which is vocal fold cancer, and the pre-malignant condition leukoplakia.
Squamous cell carcinoma is the most common histological type of laryngeal cancer and accounts for the majority of cases. Less common malignancies include sarcoma, lymphoma, adenocarcinoma, and neuroendocrine carcinoma.[25][26]
Granulomata should be differentiated from squamous cell carcinoma.[27]
The most important risk factor for the development of laryngeal malignancies is tobacco use, and this risk is accentuated by excessive alcohol intake.[28][29][30][31] Other risk factors include human papilloma virus infection (typically subtypes 16 and 18) and GORD.[32][33]
Vocal fold leukoplakia is a pre-malignant change of vocal cord epithelium secondary to tobacco use or excessive alcohol.[34] Previous radiotherapy to the head and neck and laryngopharyngeal reflux have also been implicated in the development of leukoplakia.[35][36][Figure caption and citation for the preceding image starts]: Vocal fold cancerFrom the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends]. [Figure caption and citation for the preceding image starts]: LeukoplakiaFrom the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].
[Figure caption and citation for the preceding image starts]: LeukoplakiaFrom the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].
Use of this content is subject to our disclaimer