Investigations
1st investigations to order
CT scan with contrast/CT angiogram
Test
Prioritise an urgent CT scan of the abdomen if you suspect acute or chronic mesenteric ischaemia.[8][20][30] Obtain the scan early; prompt diagnosis (and intervention) is essential to improve the clinical outcome.
Use multidetector CT scanning with intravenous contrast for suspected acute mesenteric ischaemia.[20]
Consider a CT scan even in the presence of renal impairment in order to save life and prevent worsening renal injury.[8][9][20]
CT provides evidence for the extent of bowel compromise from ischaemia.[39][40] It also enables stratification of patients to differentiate those who would benefit from mesenteric angiography from those who require primary surgery; CT can inform pathological staging, the degree of involvement of each layer of the gastrointestinal tract (mucosa, submucosa, muscularis, and serosa) can be used to estimate the probability of reversibility of the ischaemia, therefore helping to guide treatment.[42]
[Figure caption and citation for the preceding image starts]: CT scan: colonic thickening with pneumatosis intestinalisFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: 84-year-old man presenting with symptoms suggestive of ischaemic bowel disease: (A) Abdominal CT revealing a massive circumferential and band-like air formation as intestinal pneumatosis (arrows) and pronounced oedema of mesenteric fat (arrowhead) around necrotic bowel loops; (B) Another slice of abdominal CT showing long segmental pneumatosis of the small bowelLin I, Chang W, Shih S, et al. Bedside echogram in ischaemic bowel. BMJ Case Reports 2009:bcr.2007.053462 [Citation ends].
[Figure caption and citation for the preceding image starts]: 84-year-old man presenting with symptoms suggestive of ischaemic bowel disease: (A) Abdominal CT revealing a massive circumferential and band-like air formation as intestinal pneumatosis (arrows) and pronounced oedema of mesenteric fat (arrowhead) around necrotic bowel loops; (B) Another slice of abdominal CT showing long segmental pneumatosis of the small bowelLin I, Chang W, Shih S, et al. Bedside echogram in ischaemic bowel. BMJ Case Reports 2009:bcr.2007.053462 [Citation ends].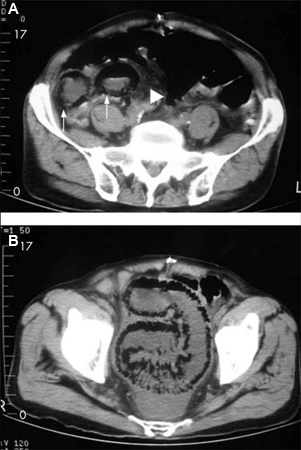
Presence of the thumbprinting sign, indicative of mucosal oedema, suggests a worse prognosis.
[Figure caption and citation for the preceding image starts]: CT scan: circumferential wall thickening of the transverse colon; white arrow shows thumbprintingFrom the collection of Dr Amir Bastawrous; used with permission [Citation ends].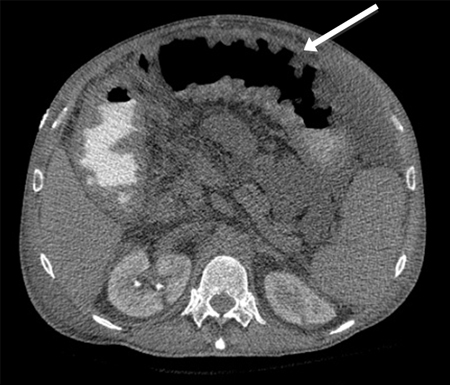
It also enables stratification of patients to differentiate those who would benefit from mesenteric angiography from those who require primary surgery; CT can also inform pathological staging; the degree of involvement of each layer of the gastrointestinal tract (mucosa, submucosa, muscularis, and serosa) can be used to estimate the probability of reversibility of the ischaemia, therefore helping to guide treatment.[42]
For diagnosing acute mesenteric vein thrombosis (MVT), contrast-enhanced CT is the procedure of choice, enabling diagnosis in >90% of patients. A central lucency in the mesenteric veins after injection of contrast is suggestive of a thrombosis. Other suggestive findings include enlargement of the superior mesenteric vein, thickening of the bowel wall, or dilated collaterals in a thickened mesentery. If MVT is diagnosed on CT scan, angiography may not be necessary, although it does provide better delineation of thrombosed veins and facility for intra-arterial vasodilators.[32]
Consider early CT angiography in a patient with abdominal pain and lactic acidosis.[8]
CT angiography has replaced conventional angiography as standard practice for diagnosis of acute mesenteric ischaemia. It can be used in the diagnosis of non-occlusive mesenteric ischaemia (NOMI).[43] CT angiography can also provide information to help decide on treatment modality, such as endovascular repair.
[Figure caption and citation for the preceding image starts]: CT angiography: 3-dimensional reconstruction with superior mesenteric artery stenosis from severe atherosclerotic plaque in a patient on follow-up imaging for endovascular aneurysm repairFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: CT angiogram: Acute superior mesenteric artery thrombusFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CT angiogram: Acute superior mesenteric artery thrombusFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends].
In ischaemic colitis, features of colitis such as bowel wall thickening and pericolic fat stranding may be seen on CT.[36][37] Right-sided involvement seen on CT may indicate severe disease needing surgical intervention.[36]
Result
bowel wall thickening, bowel dilation, pneumatosis intestinalis, portal venous gas, occlusion of the mesenteric vasculature, bowel wall thickening with thumbprinting sign suggestive of submucosal oedema or haemorrhage
FBC
Test
More than 90% of patients with acute mesenteric ischaemia will have an abnormally elevated leukocyte count.[8]
May reveal anaemia (often as a result of repeated episodes of melaena) that exacerbates ischaemia.
Result
leukocytosis, anaemia, evidence of haemoconcentration
arterial blood gases and serum lactate
Test
Metabolic acidosis is a common finding in patients with acute mesenteric ischaemia.[8]
Elevated serum lactate does not determine the presence or absence of ischaemic or necrotic bowel; however, it can be used to assist with making the diagnosis and determining the severity of the illness.[8]
Result
acidosis
urea and electrolytes
Test
Helps assess renal dysfunction and dehydration, frequently present in patients with ischaemic bowel disease.
Result
uraemia, elevated creatinine
liver function tests
Test
Check for derangement.
Result
may be elevated as a consequence of septic shock or concomitant with bowel ischaemia
CRP
Test
Request in suspected ischaemic colitis.[36]
Result
elevated in the presence of inflammation; not specific but may be indicative of disease severity
coagulation studies, group and save and crossmatch
Test
Aids in the diagnosis of any underlying coagulopathy as a risk factor for further thrombosis. Allows correction of any clotting dyscrasia as part of treatment.
Group and save in preparation for the possibility of transfusion.
Result
underlying prothrombotic disorder
ECG
Test
Perform as part of the cardiovascular examination.
May demonstrate arrhythmias that predispose to cardioembolic complications, such as atrial fibrillation or atrial flutter, or acute infarction that may be the aetiology of intestinal ischaemia.
Result
atrial fibrillation, atrial flutter, acute myocardial infarction
erect CXR
Test
Chest x-ray may show sub-diaphragmatic air, indicative of perforation of the bowel requiring prompt surgical intervention. X-rays are not a frequently used investigation for ischaemic bowel disease.
Result
free air if perforation present
sigmoidoscopy or colonoscopy
Test
Sigmoidoscopy or colonoscopy can be used to establish the diagnosis of colonic ischaemia, establish severity, and exclude alternative causes of colonic inflammation. However, if urgent surgical intervention is required due to the condition of the patient, surgery should not be delayed to carry out sigmoidoscopy or colonoscopy.
[Figure caption and citation for the preceding image starts]: Colonoscopy: demarcation between ischaemic and normal colonFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends].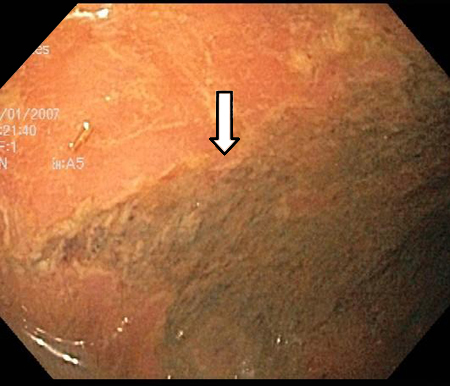 [Figure caption and citation for the preceding image starts]: Colonoscopy: denudation of colonic mucosaFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Colonoscopy: denudation of colonic mucosaFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends].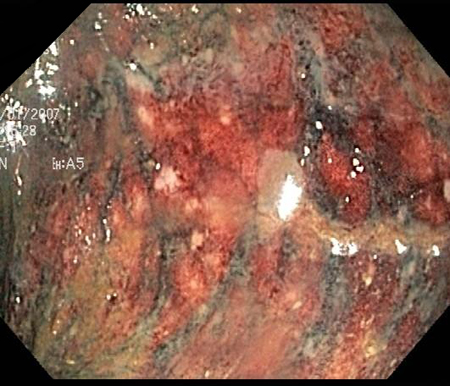 [Figure caption and citation for the preceding image starts]: Colonoscopy: mucosal sloughing and likely to be non-viable colonFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Colonoscopy: mucosal sloughing and likely to be non-viable colonFrom the collection of Dr Jennifer Holder-Murray; used with permission [Citation ends].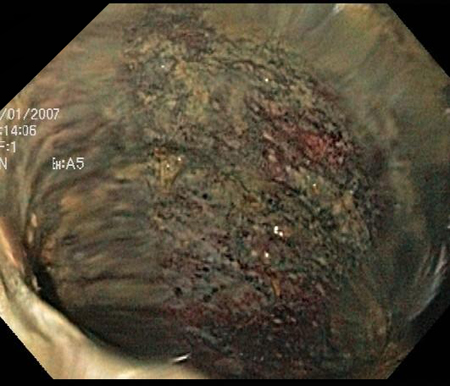
Result
mucosal sloughing or friability; mucosal petechiae; submucosal haemorrhagic nodules, erosions, or ulcerations; submucosal oedema; luminal narrowing; necrosis, gangrene
upper gastrointestinal endoscopy
Test
Perform upper gastrointestinal endoscopy in patients with suspected chronic mesenteric ischaemia, in order to rule out alternative diagnoses involving the upper gastrointestinal tract.[30]
Result
normal in patients with chronic mesenteric ischaemia
D-dimer
Test
May be elevated in intestinal ischaemia, but its use is limited because D-dimer is a very non-specific test.[8]
Result
may be elevated
Investigations to consider
mesenteric angiography
Test
Historically, mesenteric angiography has been the definitive test for diagnosing mesenteric ischaemia. In current practice it is usually preceded by positive CT angiography in the acute setting. Sensitivity is 74% to 100%, and specificity is 100%.
Mesenteric angiography can diagnose non-occlusive mesenteric ischaemia before infarction occurs. Look for:
Narrowing of the origins of the superior mesenteric artery branches
Irregularities in these branches
Spasm of the mesenteric arcades
Impaired filling of the intramural vessels.
Mesenteric angiography is often performed with the intention of proceeding to intervention. It enables treatment by infusion of vasodilators or thrombolytic agents (which have been shown to improve outcomes).
For the diagnosis of chronic mesenteric ischaemia, angiography needs to demonstrate severe occlusion of at least 2 of the 3 splanchnic vessels, although in the absence of symptoms an abnormal angiography result alone is not sufficient for diagnosis.[45]
Result
proximal defect of a mesenteric vessel or vasoconstriction of all mesenteric arcades
mesenteric duplex ultrasound
Test
Mesenteric duplex ultrasound is particularly useful if obstruction is proximal in the mesenteric vessels, but ultrasound cannot assess distal mesenteric blood vessel flow and non-occlusive aetiology of ischaemia.[9] This is mostly used in vascular units where it is the first-line investigation of choice for the assessment of chronic mesenteric ischaemia.[46]
Ultrasound of the bowel can be used to diagnose ischaemic colitis (providing the user has adequate expertise) and differentiate between left- and right-sided disease.[37] It is an alternative for patients unable to tolerate contrast media.[36] However, it is not considered a routine investigation and should only be performed by a radiologist with sufficient ultrasound expertise.
Result
reduced or lack of blood flow through proximal mesenteric vessels
magnetic resonance angiography
Test
Magnetic resonance angiography may have a role in diagnosing chronic mesenteric ischaemia.[30] However, CT angiography is a better examination than MRA for the diagnosis of chronic mesenteric ischaemia because of its capacity for higher resolution in combination with faster scans.
The time required to perform MRA examinations, and the possible need for bowel stimulation with a meal, limit the usefulness of MRA in the diagnosis of acute mesenteric ischaemia.
Result
narrowing or obstruction of mesenteric vasculature; decreased bowel wall enhancement
amylase
Test
Elevated serum amylase is found in approximately half of patients with acute mesenteric ischaemia.[8]
Result
possibly elevated
studies for ova, cysts, and parasites
faecal culture
Clostridium difficile toxin assay
abdominal x-rays
Test
Abdominal x-ray has a limited role in the diagnosis and evaluation of acute mesenteric ischaemia.[8][20]
A negative radiograph does not exclude the diagnosis.[8] Plain x-rays are often normal early in the course of ischaemia or when ischaemia is mild. X-rays are not a frequently used investigation for ischaemic bowel disease.
With worsening ischaemia, plain x-rays may show formless loops of bowel, ileus, or thickening of the bowel wall with thumbprinting sign suggestive of submucosal oedema or haemorrhage.[Figure caption and citation for the preceding image starts]: Plain abdominal x-ray: shows marked wall thickening of the transverse colon compatible with the finding of thumbprinting (white arrows)From the collection of Dr Amir Bastawrous; used with permission [Citation ends].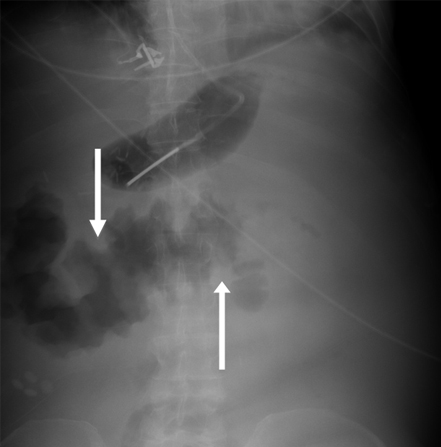
Result
air-fluid levels, bowel dilation, bowel wall thickening, pneumatosis
Use of this content is subject to our disclaimer